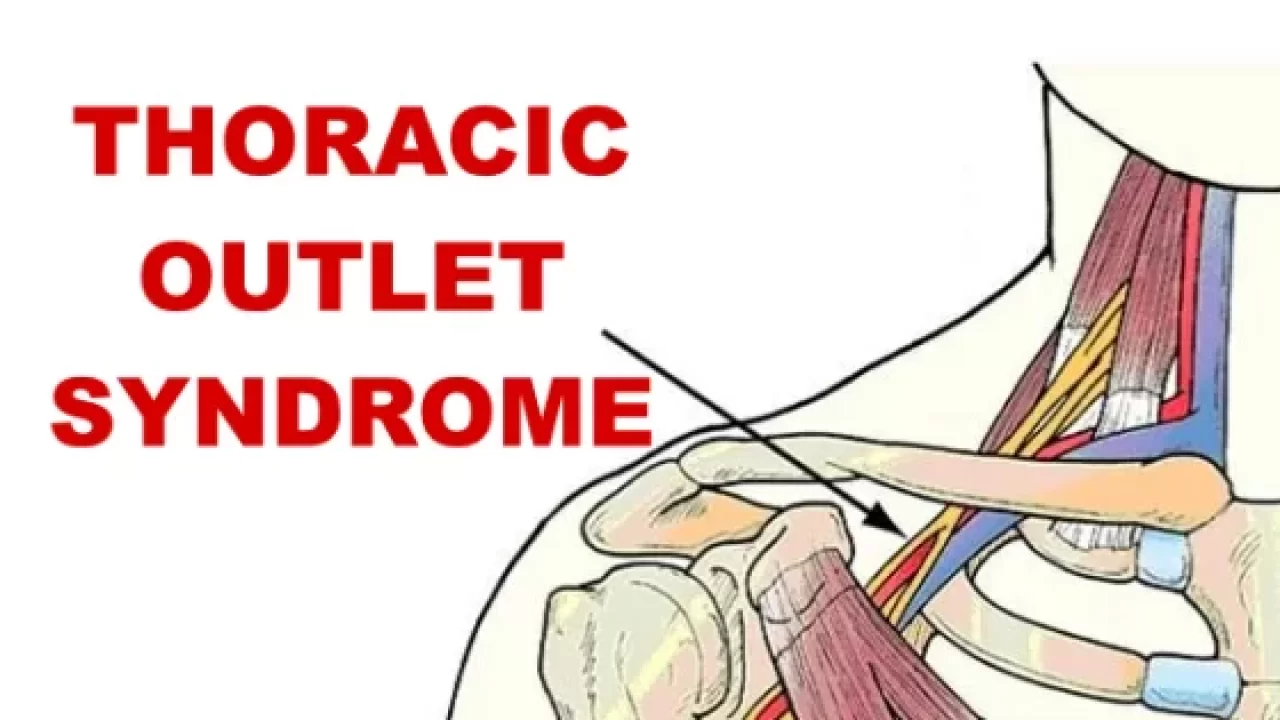
Thoracic Outlet Syndrome (TOS)
Table of Contents
What’s thoracic outlet syndrome?
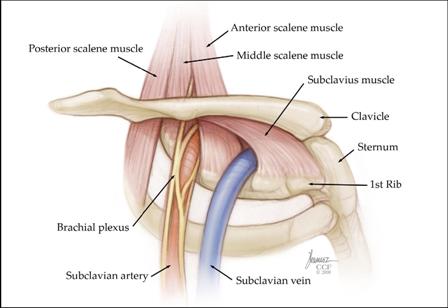
Thoracic outlet syndrome is a condition that results from compression of the nerves and/or blood vessels passing from the neck to the shoulder and arm. Symptoms include pain, numbness, tingling, and even weakness in the affected limb. The compression can be caused by several factors, including trauma or anatomical abnormalities. Treatment typically involves physical therapy and/or surgery to relieve pressure on the affected areas.
Thoracic outlet syndrome is a condition in which the neurovascular bundle, which includes the subclavian artery, subclavian vein, and brachial plexus, becomes compressed or obstructed. This can lead to pain in the neck, shoulder, upper back, and arms.
Common Symptoms include tingling sensations in the hands and fingers as well as numbness. Thoracic outlet syndrome is commonly caused by repetitive motions that involve lifting of the arms above the head. It can also be caused by trauma to the shoulder area.
DEFINITION:
The term ‘thoracic outlet syndrome’ describes compression of the neurovascular structures as they exit through the thoracic outlet (cervicothoracobrachial region). The thoracic outlet is marked by the anterior scalene muscle anteriorly, the middle scalene posteriorly, and the first rib inferiorly.
CAUSES ARE:
In general, the cause of thoracic outlet syndrome is compression of the nerves or blood vessels in the thoracic outlet, just under your collarbone (clavicle). The cause of the compression varies and can include:
- Anatomical defects:
Inherited defects that are present at birth (congenital) may include an extra rib located above the first rib (cervical rib) or an abnormally tight fibrous band connecting your spine to your rib.
2. Poor posture:
Drooping your shoulders or holding your head in a forward position can cause compression in the thoracic outlet area.
Trauma. A traumatic event, such as a car accident, can cause internal changes that then compress the nerves in the thoracic outlet. The onset of symptoms related to a traumatic accident often is delayed.

3. Repetitive activity:
Doing the same thing repeatedly can, over time, wear on your body’s tissue. You may notice symptoms of thoracic outlet syndrome if your job requires you to repeat a movement continuously, such as typing on a computer, working on an assembly line, or lifting things above your head, as you would if you were stocking shelves. Athletes, such as baseball pitchers and swimmers, also can develop thoracic outlet syndrome from years of repetitive movements.
4. Pressure on your joints :
Obesity can put an undue amount of stress on your joints, as can carrying around an oversized bag or backpack.\
5. Pregnancy:
Because joints loosen during pregnancy, signs of thoracic outlet syndrome may first appear while you’re pregnant.
TYPES OF TOS:
There are three types of TOS:
- Vascular:
This can be a compression of the artery and vein.
2. Neurogenic:
The nerves become compromised from an extra cervical rib, present at birth.
3. Disputed or painful form:
There is no neurological deficit but patients experience neurological symptoms and pain. Typically the patients’ electrodiagnostic studies (EMG / NCV) are normal, but they complain of pain.
Thoracic outlet syndrome symptoms :
Signs and symptoms of vascular thoracic outlet syndrome can include:
1. Discoloration of your hand (bluish color)
2. Arm pain and swelling, possibly due to blood clots
3. Blood clot in veins or arteries in the upper area of your body
4. Lack of color (pallor) in one or more of your fingers or your entire hand
5. Weak or no pulse in the affected arm
6. Cold fingers, hands, or arms
7. Arm fatigue with activity
8. Numbness or tingling in your fingers
9. Weakness of arm or neck
10. Throbbing lump near your collarbone
DIAGNOSIS:
A.Physical Examination
- Observation
- Posture
- Cyanosis
- Edema
- Paleness
- Muscle Atrophy
- Palpation
- Temperature changes
- Supraclavicular fossa
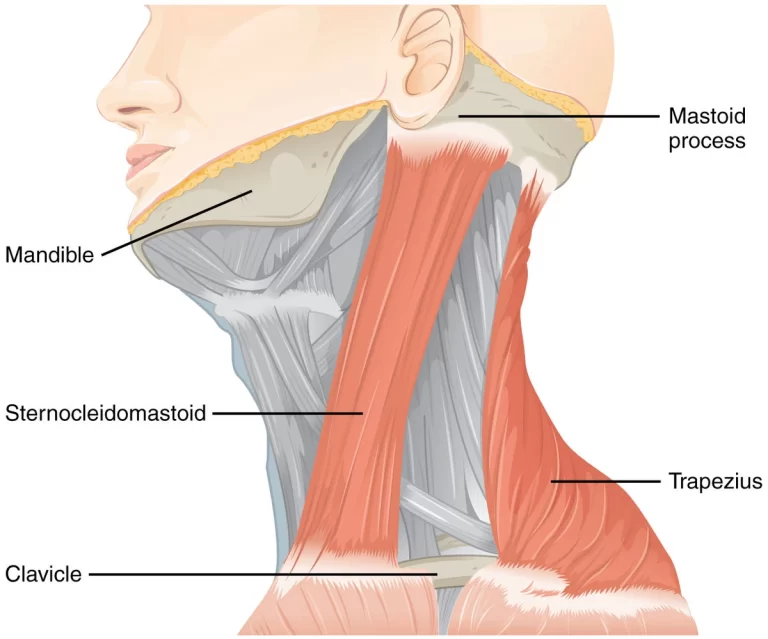
- Scalene muscles (tenderness)
- Trapezius muscle (tenderness)
- Neurological Screen
Thoracic outlet syndrome test
The following test are useful in the Diagnosis of Thoracic outlet syndrome.
B.SPECIAL TESTS ARE:
- Elevated Arm Stress/ Roos test:
the patient has arms at 90° abduction and the therapist puts downwards pressure on the scapula as the patient opens and closes the fingers. If the TOS symptoms are reproduced within 90 seconds, the test is positive.

2. Adson’s Test:

Palpate the radial pulse on the affected side with the elbow fully extended. Have the patient rotate their head to the side being tested and extend the neck. Next, abduct, extend, and laterally rotate the shoulder. From this position, have the patient take a deep breath and hold. Assess the pulse response. A positive test is a decrease in pulse vigor from the starting position to the final position.

3. Wright’s:
the patient’s arm is hyper-abducted. If there is a decrease or absence of a pulse on one side then the test is positive, showing the axillary artery is compressed by the pectoralis minor muscle or coracoid process due to stretching of the neurovascular bundle.
C.Diagnosis will include:
1. A comprehensive clinical exam, including neurological exams
2. Complete medical history
3. Imaging studies such as X-rays and/or MRI (magnetic resonance imaging)
4.Electrodiagnostic studies (EMG)
Treatment for thoracic outlet syndrome:
- Nonsurgical treatment for thoracic outlet syndrome:
There are several forms of treatment for patients with TOS. These may include:
Physical therapy with careful nerve stretching movements performed by a qualified and experienced physical therapist with experience treating TOS.
2. Injections with nerve-blocking agents to suppress pain and reduce swelling and compression.
3. Acupuncture:
Some patients with TOS have found relief using acupuncture.
4. Surgery for thoracic outlet syndrome (TOS):
When physical therapy and other forms of non-surgical treatment fail, surgery is the best option to restore function and alleviate pain.
Physiotherapy Treatment:
Stage 1:
The aim of the initial stage is to decrease the patient’s symptoms. This may be achieved by patient education, in which TOS, bad postures, the prognosis, and the importance of therapy compliance are explained. Furthermore, some patients who sleep with their arms in an overhead, abducted position should get some information about their sleeping posture to avoid waking up at night. These patients should sleep on their uninvolved side or in supine, potentially by pinning down the sleeves.
Exercises for thoracic outlet syndrome
Stage 2:
-Massage
-Strengthening of the levator scapulae, sternocleidomastoid, and upper trapezius.
Stretches for thoracic outlet syndrome
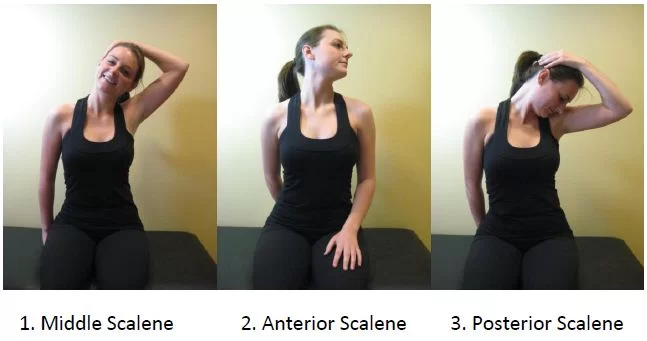
-Stretching of the pectoralis major/minor, lower trapezius, and scalene muscles (These muscles close the thoracic outlet).
– Postural correction exercises.
-Relaxation of shortened muscles.
-Aerobic exercises in a daily home exercise program.
-Shoulder exercises :
– to restore the range of motion and so provide more space for the neurovascular structures.
-Exercise: Lift your shoulders backward and up, flex your upper thoracic spine and move the shoulders forward and down. Then straighten the back and repeat 5 to 10 times.
-Exercise: Lower your chin 5 to 10 times against your chest, while you are standing with the back of your head against a wall. The effectiveness of this exercise can be enlarged by pressing the head down with hands.

-Activation of the scalene muscles is the most important exercise. These exercises help to normalize the function of the thoracic aperture as well as all the malfunctions of the first rib. Exercises are Anterior scalene (Press your forehead 5 times against the palm of your hand for a duration of 5 seconds, without creating any movement), Middle scalene (Press your head sidewards against your palm), Posterior scalene (Press your head backward against your palm.




I have this problem I don’t how to cure myself can someone help me please?