Wartenberg’s syndrome (superficial radial nerve neuritis)
Table of Contents
What is a Wartenberg’s Syndrome?
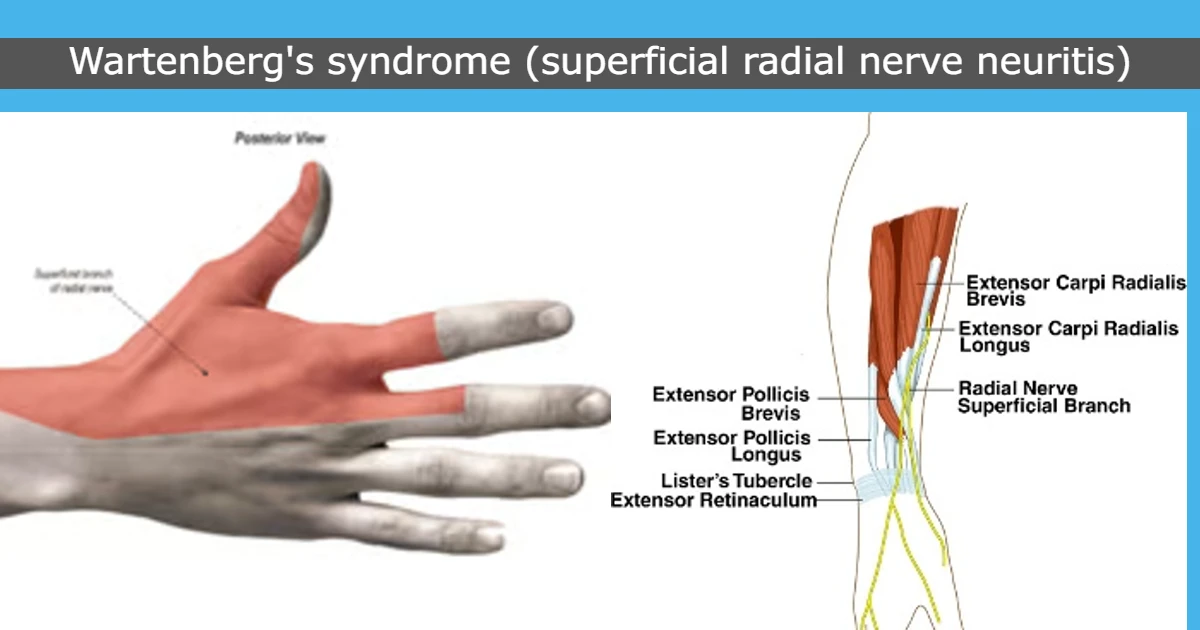
Wartenberg’s Syndrome is a condition in which the superficial branch of the radial nerve is compressed which causes Pain over the distal radial side forearm (Just above the wrist) with burning or prickling sensation or loss of sensation (paresthesia) over The back side of the hand.
When a superficial branch of the radial nerve is compressed, only the sensory part is affected while motor functions are intact. It is also called “cheiralgia paresthetica” or superficial radial nerve neuritis.
Wartenberg’s Syndrome is mostly confused with Wartenberg’s Sign where the slightly greater abduction of the fifth finger is mainly due to paralysis palmar interosseous muscle which works as adduction of the finger and common action of the extensor muscles(digiti minimi, digitorum communis) of finger supplied by the radial nerve.
Doctors usually diagnose the patient after examining the patient’s symptoms like pain and paresthesias over the dorsoradial hand without any motor function affected.
Treatment is also symptomatic like rest, analgesics, wrist splints, and CSIs while surgical decompression is the last option.
History:
In 1932, Wartenberg reported five cases of isolated neuropathy of the Superficial Radial Nerve (SRN). He was so influenced by the similarity to the isolated involvement of the lateral cutaneous nerve of the thigh, Meralgia Paraesthetica, that he proposed the name Cheiralgia Paraesthetica.
The condition is also called Wartenberg’s Disease, However, Wartenberg was not the first to take awareness of it. He mentions the early authors in his reports.
Related Anatomy:
The Superficial Radial Nerve is the superficial sensory branch of the radial nerve. The radial nerve is divided into 2 branches – the Superficial Radial Nerve (SRN) and Posterior Interosseous Nerve (PIN.
Superficial Radial Nerve travels distally into the forearm deep to the brachioradialis muscle. Nearby 9 cm proximal to the radial styloid (wrist joint), the SRN becomes a subcutaneous branch traveling between the brachioradialis and Extensor Carpi Radialis Longus tendons. The SRN again passes in the subcutaneous tissues and gives branches into dorsal digital nerves that work for afferent sensory input from the backside of the thumb, index, and middle fingers proximal to the proximal IP (interphalangeal) joints.
What are the Causes of Wartenberg’s syndrome?
The SRN can be compressed at any point along its route in the forearm, but it is mostly at greatest risk at the posterior border of the brachioradialis muscle as the nerve moves from a deep to a subcutaneous branch.
Injury is also a common cause for SRN compression, which can lead to direct compression on the nerve such as by a wristband or handcuffs, or from a overstretch injury to the nerve such as during a closed reduction of a forearm fracture.
SRN is compressed by scissoring movement of brachioradialis and ECRL tendons during forearm pronation and also by fascial bands at its leave point in the subcutaneous area.
It is also associated with De Quervain’s disease in 20-50%. Steroid injections into the tendon sheath for the treatment of de Quervain’s tenosynovitis can injure the nerve and can lead to subdermal atrophy leading to the injury of the nerve.
Other causes are:
- Minor or Major injury around the wrist
- Overuse of wrist joint mainly repetitive wrist flexion, ulnar deviation, or forearm pronation
- Tight plaster casts
- Forearm fractures
- Wearing tight bracelets, watches, handcuffs, etc.
Symptoms of Wartenberg’s syndrome
The most common symptoms such as pain, tingling, and numbness over the dorsolateral area of the hand, wrist, and fingers.
The symptoms may start from the dorsal radial forearm into the thumb, index, and long fingers.
Most of the time, the patient’s symptoms are not in a specific area. The patient often reports the pain as burning or shooting pain instead of dull and achy pain.
Other symptoms are the sensation of tingling, and numbness which is rarely seen. The symptoms may be acute, intermittent, or chronic pain, which primarily depends upon the cause of irritation.
Other associated symptoms are tenderness, neuropathic pain, dysesthesias, and hypoesthesias. Certain movements, such as flexion and ulnar deviation of the wrist, increase the symptoms.
Differential Diagnosis:
De Quervain’s Syndrome is the inflammation of the two tendons that are responsible for the movement of the thumb. The pain, Tenderness are present at the top of the forearm.
Lateral antebrachial cutaneous nerve (LACN) neuritis
The lateral antebrachial cutaneous nerve (LACN), a branch of the musculocutaneous nerve, supplies sensory stimulation to the lateral forearm. Causes of LACN are found mostly in venipuncture, elbow surgery, and injury.
Positive Tinel’s sign over LACN can be mistaken for positive Tinel’s as compared to SRN.
Intersection syndrome of the wrist:
Intersection syndrome of the wrist is a condition in which the first and second compartments of the dorsal wrist extensors are affected causing inflammatory tenosynovitis. The cause of this condition is overuse- repetitive friction at the point in which the tendons of the first dorsal compartment cross over the second, which causes inflammatory tenosynovitis.
Patients with SRN compression mostly show pain with abnormal sensation on the dorsal radial forearm extending to the thumb and index finger, however, the symptoms may differ depending upon the cause and anatomy. When such symptoms present together with the weakness of the Posterior Interosseous Nerve (PIN)-innervated muscles, the Doctor should think about alternative diagnoses, such as a more proximal lesion (of the cervical spine, posterior cord of the brachial plexus, or radial nerve) or maybe a mass in the radial tunnel area where it affects both the PIN and SRN.
Diagnosis of Wartenberg’s syndrome
Diagnosis of this condition is mostly with a careful history and physical examination by Doctor.
Physical exam:
Provocative tests:
Positive Tinel’s sign over the superficial sensory radial nerve is the most common examination test the Clinician performs. A positive Tinel sign means that percussion in your nerve causes a tingling sensation in the area of the nerve.
For that Clinician perform wrist flexion, ulnar deviation, and pronation for one minute.
Finkelstein test
Finkelstein test is a useful test to check & diagnose De Quervain’s Tendonitis/first dorsal compartment tendonitis which is described by the Swiss surgeon of Fritz de Quervain.
This test also increases symptoms in 96% of patients because of traction on the nerve
Imaging test:
X-Ray is advised if you have a history of injury or trauma
It is helpful in forearm fracture-related conditions.
Other Studies
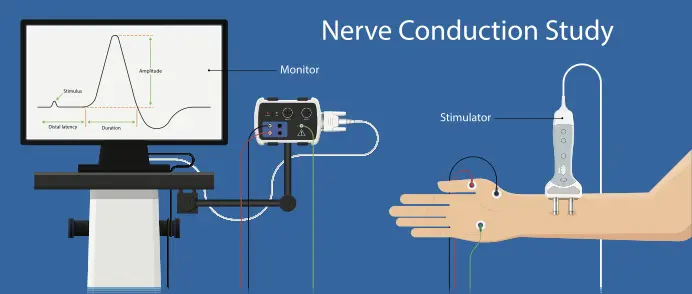
Electrodiagnostic tests:
EMG and NCV Test – Electromyography (EMG) and NCV measure muscle response or electrical activity in reaction to nerve stimulation of the muscle. The test is used to diagnose neuromuscular abnormalities.
Diagnostic injection:
A diagnostic local anesthetic injection is a useful test where it may relieve pain temporarily.
Treatment of Wartenberg’s syndrome
Treatment of This condition mostly depends upon cause and Symptomatic.
Conservative Management
- Removal of tight wristwear
- Rest or Activity modification
- Splint
- Pain-relieving Medicines mainly nonsteroidal anti-inflammatory drugs (NSAIDs)
Corticosteroid injections are the second line of treatment.
Physiotherapy Treatment in Wartenberg’s syndrome
Physiotherapy treatment also depends upon the symptoms, Pain-relieving Electrotherapy modalities such as Transcutaneous electrical nerve stimulation (TENS), and Interferential therapy (IFT) are useful to relieve pain and tingling numbness with activity modification exercise.
Stretching and strengthening exercises of the wrist muscles are useful.
Pain-free Stretching of the Radial nerve.
Surgical treatment:
Surgical decompression (neurolysis) of the SRN is advised if symptoms are seen after 6 months and conservative treatment does not help in recovery. Surgical decompression of the nerve is mostly useful in post-traumatic conditions in which scar tissue may be the critical compression of the nerve.
Surgery will be done between the brachioradialis and extensor carpi radialis longus muscles where surgeons do neurolysis and release of the fascia.
Complications:
- Failed decompression
- Persistent pain and numbness
- Wound dehiscence
- Infection
Prognosis
- Spontaneous recovery of symptoms is most commonly seen after conservative treatment
- Treatment result – 74% success after surgical decompression



2 Comments