Acute Respiratory Distress Syndrome (ARDS)
- Acute respiratory distress syndrome (ARDS) is a life-threatening lung injury caused by sepsis, pneumonia, the coronavirus (COVID-19), and another condition. Acute respiratory distress syndrome (ARDS) tends to develop within a few hours to a few days of the event that caused it and can worsen rapidly.
- Acute respiratory distress syndrome (ARDS) patients may have to be put in an intensive care unit (ICU) and on a ventilator to help them breathe.
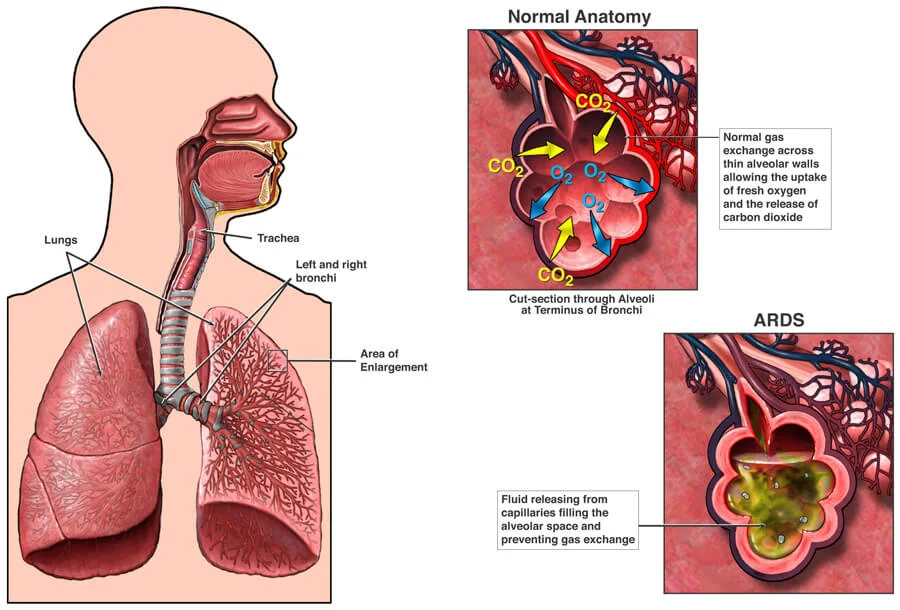
- Acute respiratory distress syndrome (ARDS) is a serious lung disease. It happens when fluid fills up the air sacs in your lungs.
- Too much fluid in your lungs can lower the amount of oxygen or increase the amount of carbon dioxide (CO2) in your bloodstream. Acute respiratory distress syndrome (ARDS) can prevent your organs from getting the oxygen they need to function, and it can eventually cause organ failure.
- Acute respiratory distress syndrome (ARDS) most commonly affects hospitalized people who are very ill. It can also be caused by severe trauma, and can sometimes begin as “walking pneumonia,” or even as an infection somewhere else in the body.
- Symptoms usually happen within a day or two of the original illness or trauma, and they may include extreme shortness of breath and gasping for air.
- Acute respiratory distress syndrome (ARDS) is a medical emergency and a potentially life-threatening condition.
Table of Contents
What is acute respiratory distress syndrome (ARDS)?
- Acute respiratory distress syndrome, or ARDS, is an inflammatory lung injury that occurs when fluids build up in small air sacs (called alveoli) in the lungs. Acute respiratory distress syndrome (ARDS) prevents the lungs from filling up with air and causes dangerously low oxygen levels in the blood (hypoxemia).
- This condition prevents other organs such as the brain, heart, kidneys, and stomach from getting the oxygen they need to function. Acute respiratory distress syndrome (ARDS) is dangerous and can lead to a number of serious and life-threatening problems.
- Acute respiratory distress syndrome (ARDS) typically happens in hospital settings while the patient is being treated for infection or trauma. If you’re not hospitalized and experience symptoms of Acute respiratory distress syndrome (ARDS), get medical attention immediately.
What causes acute respiratory distress syndrome (ARDS)?
- Acute respiratory distress syndrome (ARDS) is caused when fluids leak from little lung vessels into lung air sacs (alveoli). When the protective membrane between blood vessels & air sacs is compromised, levels of oxygen in the blood are reduced.
- Acute respiratory distress syndrome (ARDS) is primarily caused by damage to the small blood vessels in your lungs. Fluid from these vessels exudes into the air sacs of the lungs. These air sacs are where oxygen goes and carbon dioxide is removed from your blood.
- When these air sacs fill with fluid, decrease oxygen gets to your blood.
Causes of acute respiratory distress syndrome (ARDS) involve:
- Sepsis: The most common cause of acute respiratory distress syndrome (ARDS), is a serious infection in the lungs (pneumonia) or other organs with widespread inflammation.
- Aspiration pneumonia: Aspiration of stomach contents into the lungs may cause severe lung damage and acute respiratory distress syndrome (ARDS).
- The coronavirus (COVID-19): The infection COVID-19 may develop into severe acute respiratory distress syndrome (ARDS).
- Pancreatitis (serious inflammation in the pancreas), and massive blood transfusion.
- Major trauma and burns: Accidents and falls may directly damage the lungs or another organ in the body that triggers severe inflammation injury in the lungs.
- Inhalational injury: Breathing and exposure to increase concentrations of chemical fumes or smoke.
- Drug overdose: An overdose on drugs such as cocaine and opioids.
- inhaling toxic substances, like salt water, chemicals, smoke, and vomit
- developing a serious blood infection
- developing a serious infection of the lungs, such as pneumonia
- receiving an injury to the chest or head, like during a car wreck or contact sports
- overdosing on sedatives or tricyclic antidepressants.
Is acute respiratory distress syndrome (ARDS) infectious?
- As a lung condition, acute respiratory distress syndrome (ARDS) can occur in both males and females. It is not contagious and cannot be transferred from person to person.
- It Is not considered an inherited disease. It commonly develops later in a person’s life. However, it is important to note that acute respiratory distress syndrome (ARDS) is a byproduct of lung damage and can affect people of any age.
What are the symptoms of Acute Respiratory Distress Syndrome (ARDS)?
Symptoms of Acute Respiratory Distress Syndrome (ARDS) depend on the cause and seriousness of the case, as well as pre-existing lung or heart conditions. Symptoms involve:
- Serious shortness of breath or breathlessness.
- Rapid & labored breathing.
- High-level tiredness and muscle fatigue.
- Confusion.
- Rapid heart rate.
- The bluish color of fingernails and lips is due to the low oxygen level in the blood.
- Cough and chest pain.
- If acute respiratory distress syndrome (ARDS) is caused by a severe infection (sepsis), symptoms of sepsis may also be present (fever, low blood pressure).
How fastly can acute respiratory distress syndrome (ARDS) develop?
- Acute respiratory distress syndrome (ARDS) tends to develop within a few hours to a certain day of the event that caused it. Acute respiratory distress syndrome (ARDS) can worsen rapidly.
What tests are done to diagnose acute respiratory distress syndrome (ARDS)?
- Acute respiratory distress syndrome (ARDS) is a medical emergency, and an early diagnosis may help them survive the condition.
- A doctor can diagnose acute respiratory distress syndrome (ARDS) in several different ways, though figuring out its cause is often difficult. There is no definitive test for diagnosing this condition.
When symptoms of acute respiratory distress syndrome (ARDS) occur, a combination of tests may be done:
- Chest X-ray to calculate fluids in the lungs.
- A blood test to determine the oxygen level in the blood to help determine the severity of acute respiratory distress syndrome (ARDS).
- Echocardiogram (ultrasound of the heart) to assess heart function.
- Sometimes, symptoms and signs of acute respiratory distress syndrome (ARDS) may require additional tests to diagnose other causes that are similar to acute respiratory distress syndrome (ARDS).
- A computerized tomography (CT scan) may be done to obtain detailed information about the lungs.
- A sampling of secretions from the airways may be taken to find the cause of infection.
Low blood pressure and low blood oxygen can be signs of acute respiratory distress syndrome (ARDS). The doctor may rely on an electrocardiogram and echocardiogram (ECG) to rule out a heart condition. If a chest X-ray or CT scan then reveals fluid-filled air sacs in the lungs, a diagnosis of acute respiratory distress syndrome (ARDS) is confirmed.
A lung biopsy can also be leaded to rule out other lung diseases. However, this is certainly done.
Risk factors for ARDS
Acute respiratory distress syndrome (ARDS) is commonly a complication of another condition. These factors increase the risk of developing acute respiratory distress syndrome (ARDS):
- age over 65 years
- chronic lung disease
- a history of alcohol misuse or cigarette smoking.
Acute respiratory distress syndrome (ARDS) can be a more serious condition for people who:
- have toxic shock
- are older
- have liver failure
- have a history of alcohol misuse.
How is acute respiratory distress syndrome (ARDS) treated?
- Acute respiratory distress syndrome (ARDS) is usually treated in the intensive care unit (ICU) along with treatment of the underlying cause.
- Mechanical ventilation (a ventilator) is sometimes used in caring for patients with acute respiratory distress syndrome (ARDS). For milder cases of acute respiratory distress syndrome (ARDS), oxygen may be given through a fitted face mask or a cannula fitted over the nose.
- Steps to minimize complications (see below) from acute respiratory distress syndrome (ARDS) are commonly used.
These involve:
- Sedation to manage pain.
- Breathing tests to determine when it is safe to remove the tube and ventilator.
- Blood thinners to cure clots.
- Minimizing fluid buildup in the lungs.
- Minimizing stress ulcers in the stomach.
- Active mobility and physical therapy to cure muscle weakness.
- No direct drug therapy has been shown to improve survival in acute respiratory distress syndrome (ARDS), but researchers continue to work on finding treatment.
Oxygen
- The primary goal of acute respiratory distress syndrome (ARDS) treatment is to ensure a person has enough oxygen to prevent organ failure.
- A doctor may administer oxygen (O2) by mask. A mechanical ventilation machine can also be used to force air into the lungs and decrease fluid in the air sacs.
Management of fluids
- Management of fluid intake is another acute respiratory distress syndrome (ARDS) treatment strategy.
- This can assist ensure an adequate fluid balance. Too much fluid in the body can conduct to fluid buildup in the lungs.
- However, too small a fluid can cause the organs and heart to become strained.
Medication
People with acute respiratory distress syndrome (ARDS) are often given medication to deal with side effects. These involve the following types of medications:
- pain medication to relieve discomfort
- antibiotics to treat an infection
- blood thinners to keep clots from forming in the lungs or legs.
Pulmonary rehabilitation
- People recovering from acute respiratory distress syndrome (ARDS) may need pulmonary rehabilitation. This is a way to strengthen the respiratory system and improve lung capacity. These programs can include exercise training, lifestyle classes, and support teams to aid in the recovery from acute respiratory distress syndrome (ARDS).
Advances in acute respiratory distress syndrome treatment
- Since the first acute respiratory distress syndrome (ARDS) caseTrusted Source in 1967, researchers have tried to better understand and manage the disease. This has helped physicians and scientists learn the markers and risk factors of acute respiratory distress syndrome (ARDS), and figure out the most effective diagnosis and treatment methods.
- There is significantly more research to be done about acute respiratory distress syndrome (ARDS), and experts are working to find effective ways in determining subphenotypes and endotypes within acute respiratory distress syndrome (ARDS) cases. This is to determine which treatment method is good for each individual.
- Additionally, there is the ongoing development of different medications and stem cell therapy. Experts are also replicating before-treatment methods that have proven successful for future cases.
Diagnostic Procedures
- According to the National Heart, Lung, and Blood Institute, a diagnosis will be made via the examination of your medical history, physical exam, & test results.
Medical History
- History of heart failure
- Has the patient had any direct or indirect clinical risk factors for acute respiratory distress syndrome (ARDS)?
Physical Examination
- Added breath sounds on auscultation (ex. crackling),
- Heart auscultation,
- Cyanosis.
Possible Interventions for acute respiratory distress syndrome (ARDS)
NB Consider the risk vs reward of your intervention, mainly when the lungs are as brittle
- Suctioning (Open / Closed)
- Ventilator Hyperinflation (VHI)
- Positioning (see below).
Ventilator Hyperinflation (VHI)
- A systematic review by Anderson et al (2015) considered that both manual and ventilator hyperinflation have similar effects on secretion clearance, pulmonary compliance, improved atelectasis, and oxygenation without a detrimental risk to cardiovascular stability.
- However, a manometer should be used throughout the intervention with important attention paid to contraindications.
- Due to the high levels of PEEP that are required to maintain lung recruitment for an acute respiratory distress syndrome (ARDS) patient, using the ventilator to deliver the hyperinflation is ideal.
- Also, Ventilator Hyperinflation (VHI) allows the continuous monitoring and monitoring of airway pressures allowing the delivery to be titrated accordingly.
Prone Positioning
Placing the acute respiratory distress syndrome (ARDS) patient prone will result in a significant increase in PaO2 for approximately 70% of the patients. By placing the patient in a prone, there is an improvement in the recruitment of the dorsal part of the lung resulting in a more evenly distributed perfusion and improving V/Q matching. Evidence has shown that prone positioning is beneficial, particularly for those who are severely hypoxaemic/severe acute respiratory distress syndrome (ARDS), with reductions in ICU mortality without increased airway complications.
- Explain to the patient, with reassurance, that they will be safe and acquire consent if they are able to communicate.
- Close your eyes and protect them with gel or a pad.
- Place the patient’s palms oppose their thighs, thumbs upwards, elbows straight, and shoulders neutral.
- Slide the patient to the last using a Sliding sheet.
- Roll the patient into the lateral position using the underneath sheet.
- Roll patient into prone.
- ‘Swimmers position’ – elbow in which the head is semi-rotated should be flexed to no more than 90° to avoid ulnar nerve stretch, and another arm internally rotated by the side.
- Make sure that women’s breasts or men’s genitals are not compressed.
- Place two pillows under each shin to prevent peroneal nerve stretch, positioning them to avoid knee and toe pressure from the mattress.
Mechanical Ventilation
- As a result of the acute onset of hypoxaemic respiratory failure with improved work of breathing, mechanical ventilation is commonplace.
- The pathophysiology of acute respiratory distress syndrome (ARDS), and in particular the fibrosing aspect means that the method and delivery of support require careful consideration to ensure that ventilator-induced lung injury (VLII) does not happen.
- In the acute respiratory distress syndrome (ARDS) patient, the PEEP and tidal volume have to be reduced to reflect the available parts of the lung that are available for aeration.
- If not, this can conduct in an over-stretching of the lung, known as volutrauma due to decreased lung compliance. Repeated opening and closing of the alveoli during tidal inflation can also cause injury to the lung tissue, called alert trauma.
- If the mechanical support is not titrated to the patient, both alert trauma and volutrauma can improve the cytokines within the lung tissue which then may enter the systemic circulation and potentially conduct multiple organ failure.
- Although perhaps oversimplified, the graph below attempts to highlight the optimal area for ventilation of the acute respiratory distress syndrome (ARDS) patient. The reduced inflection point (LIP) is thought to be the pressure at which lung tissue is recruited.
- The upper inflection point (UIP) is the approximate pressure at which the alveoli become distended which can potentially conduct damage. Therefore, the most optimum position to ventilate would be between the 2 inflection points, on the steepest most compliant aspect of the curve.
Inverse Ratio Ventilation (IRV)
- This mode of ventilation needs the alteration in the normal inspiratory/expiratory ratio of 1:2 to either 1:1 or 2:1. While this mode of ventilation aims to increase the aeration and collateral ventilation of the poorly compliant lung, decreased expiration time may result in an increased in the PCO2.
- However, if hypercapnic acidosis occurs steadily then the intracellular acidosis will be well compensated, however, any form of hypercapnia should be avoided in this with or those at risk of developing raised intracranial pressures. This is known as permissive hypercapnia.
- A recent although the small study by Kotani et al (2016) showed that IRV provided acceptable gas exchange without complications for 13 people with acute respiratory distress syndrome (ARDS).
Airway Pressure Release Ventilation (APRV)
- This form of mechanical ventilation includes the delivery of CPAP with an intermittent release phase. Delivering CPAP over long periods is thought to maintain adequate lung volume and alveolar recruitment where the release is designed to aid the removal of carbon dioxide (CO2).
- Inspiration starts from a more beneficial pressure-volume relationship thus assisting oxygenation.
High-Frequency Oscillation (HFO)
- With High-Frequency Oscillation (HFO), a continuous distending pressure (CDP) is set and small tidal volumes are delivered at high frequencies with an oscillatory pump.
- Like the others, before described, this is another form of lung protective ventilation with constant lung recruitment. While a systematic review by Sud et al (2010) found that High-Frequency Oscillation (HFO) may improve survival and is unlikely to cause harm, only 8 studies were analyzed with certain patients and wide confidence intervals. There were no reports of blinding outcome assessors putting trials at risk of bias.
Extracorporeal Membrane Oxygenation (ECMO)
- Extracorporeal Membrane Oxygenation (ECMO) can be used for those patients who have severe respiratory failure and is used when conventional therapy cannot maintain adequate oxygenation.
- Extracorporeal Membrane Oxygenation (ECMO) can fully replace the function of the lungs, however, due to various complications, there needs to be consideration of the risk vs benefit.
- Extracorporeal Membrane Oxygenation (ECMO) consists of an extracorporeal blood circuit formed via an oxygenator and a pump. Two vascular accesses are established, 1 removes the venous blood and one infuses the oxygenated blood.
- Later the blood has been removed from a major vein, it is pumped through a circuit that contains an oxygenator that oxygenates the blood and removes the carbon dioxide (CO2). The blood is then returned via the other cannula.
Inhaled Nitric Oxide
- Not only is nitric oxide an endothelium-derived smooth muscle relaxant, but it also helps with neurotransmission, host defense, platelet aggregation, and bronchodilation.
- Inhaled nitric oxide may be delivered continuously or using intermittent inspiratory injection and a rise in PaO2 of 20% is considered a positive response. 40% – 70% of acute respiratory distress syndrome (ARDS) patients have improved oxygenation following inhaled nitric oxide and is only commonly used in patients with severe hypoxemia as a temporary rescue.
Role of the Physiotherapist
- Input from physiotherapy is sometimes limited and minimal often due to the need for high PEEP and high oxygen requirements. As it is an interstitial pathology secretions are not commonly a problem. Treatment may consist of positioning only, e.g. prone lying to optimize gas exchange.
- Caution is required with hands-on techniques as you want to ensure you do not de-recruit lung units losing the splinting effect of the ventilator PEEP. If secretions become an issue, ensure adequate humidification along with other techniques to increase sputum clearance.
- Minimal suctioning via ETT. A state-of-art review proposes avoiding repeated airway clearance in infants and children with acute pulmonary disease.
What complications can grow from acute respiratory distress syndrome (ARDS)?
- Complications and problems from acute respiratory distress syndrome (ARDS) may develop while a patient is in the hospital or after discharge.
- In some cases, an acute respiratory distress syndrome (ARDS) diagnosis can cause or be linked to other health conditions that will need to be addressed.
These complications can involve:
- Blood clots or deep vein thrombosis.
- Collapsed lung (pneumothorax). This may outcome from pressure applied by the ventilator to the injured stiff lungs.
- Confusion (delirium).
- Muscle weakness.
- Scarred lungs or lung fibrosis.
- Post-traumatic stress disorder (PTSD).
- Anxiety and depression.
- multiple organ failure,
- pulmonary hypertension (increase in blood pressure),
- blood clots forming during treatment,
- and atelectasis (collapse of the lung’s tiny air pockets).
It is worth noting that not everyone will experience complications, and studies have shown that certain populations can be at higher risk. For example, it is possible that men diagnosed with acute respiratory distress syndrome (ARDS) Trusted Source may experience complications from the condition at a higher rate than women.
What is the outlook for acute respiratory distress syndrome?
- Acute respiratory distress syndrome (ARDS) can be life-threatening and deadly. Yet improved care and ventilator treatments — including prone ventilation with patients lying face down to improve oxygen flow — are now helping more people survive and reduce the risk of complications from acute respiratory distress syndrome (ARDS).
- Recovery from acute respiratory distress syndrome (ARDS) may take a long time. Most of the patients can be removed from the ventilator and breathe freely.
- Some recover completely, yet others may develop chronic lung problems that require care by lung doctors (pulmonologists). Certain patients may develop post-intensive care syndrome (PICS) and can experience post-traumatic stress disorder, physical weakness, anxiety, and depression.
- A 2021 study estimated that 30 to 40 percent trusted Source of people with acute respiratory distress syndrome (ARDS) die from it. However, the risk of death is not the same for all people who develop acute respiratory distress syndrome (ARDS).
- The death rate is linked to both the cause of acute respiratory distress syndrome (ARDS) and the person’s overall health. For example, a young person with trauma-induced acute respiratory distress syndrome (ARDS) will have a better outlook than an older person with a widespread blood infection.
- Many survivors of acute respiratory distress syndrome (ARDS) fully recover within a few months. However, certain people may have lifelong lung damage.
Other side effects may involve:
- muscle weakness
- fatigue
- impaired quality of life
- compromised mental health.
Preventing acute respiratory distress syndrome (ARDS)
There is no way to prevent acute respiratory distress syndrome (ARDS) completely. However, you may be able to lower your risk of acute respiratory distress syndrome (ARDS) by doing the following:
- Look for prompt medical assistance for any trauma, infection, or illness
- If you smoke, consider ending smoking cigarettes
- Try to remain away from secondhand smoke
- Avoid alcohol. Chronic alcohol use may improve your mortality risk and prevent proper lung function
- Get your flu vaccine annually and pneumonia vaccine every five years. This reduces your risk of lung infections.
Conclusions
- Even though many risk factors for acute respiratory distress syndrome (ARDS) are known, there is no way of preventing acute respiratory distress syndrome (ARDS).
- Careful management of fluids in high-risk patients can be assisted.
- Steps should be taken to cure aspiration by keeping the head of the bed elevated before feeding.
- Lung protective mechanical ventilation strategy in patients without acute respiratory distress syndrome (ARDS) who are high risk would help prevent acute respiratory distress syndrome (ARDS).
NOTE
- Time in the ICU can be traumatic and very hard. People recovering from acute respiratory distress syndrome (ARDS) may not be able to go back to everyday life and work quickly and need support. Getting professional assistance and advice is important along the road to recovery from acute respiratory distress syndrome (ARDS).
FAQs
Acute respiratory distress syndrome (ARDS) happens when the lungs become severely inflamed from an infection or injury. The inflammation causes fluid from nearby blood vessels to leak into the tiny air sacs in your lungs, making breathing increasingly difficult. The lungs can become inflamed after pneumonia or severe flu.
Acute respiratory distress syndrome (ARDS) is a progressive disease with four stages (exudative, fibroproliferative, fibrosing alveolitis, and recovery stage).
The first symptom of acute respiratory distress syndrome (ARDS) is usually shortness of breath. Other symptoms of acute respiratory distress syndrome (ARDS) are low blood oxygen, rapid breathing, and clicking, bubbling, or rattling sounds in the lungs when breathing.
Though there is no cure for acute respiratory distress syndrome (ARDS), it’s not uniformly fatal. With treatment, an estimated 60% to 75% of those who have acute respiratory distress syndrome (ARDS) will survive the disease. “We know how to support people through acute respiratory distress syndrome (ARDS) very well,” says Lauren Ferrante, MD, MHS, a Yale Medicine pulmonary and critical care specialist.
It is important to note that most people survive acute respiratory distress syndrome (ARDS). They will not require oxygen on a long-term basis and will regain most of their lung function. Others will struggle with muscle weakness and may require re-hospitalization or pulmonary rehabilitation to regain their strength.
The first symptom of acute respiratory distress syndrome (ARDS) is usually shortness of breath. Other symptoms of acute respiratory distress syndrome (ARDS) are low blood oxygen, rapid breathing, and clicking, bubbling, or rattling sounds in the lungs when breathing. Acute respiratory distress syndrome (ARDS) can develop at any age.
The goal of treatment for acute respiratory distress syndrome (ARDS) is to improve oxygen levels and treat the underlying cause. Oxygen therapy is the main treatment for acute respiratory distress syndrome (ARDS).




One Comment