Bunionette Deformity
Table of Contents
Description
A bunionette deformity, also known as a tailor’s bunion, is a foot condition characterized by the enlargement and misalignment of the fifth metatarsal bone at the base of the little toe.
A Bunionette deformity is similar to a bunion, but it occurs on the outside of the foot rather than the big toe. It is characterized by bone a lump of bump that occurs at the base of the fifth metatarsal, which is the long bone attached to the little toe. This bunion can become painful, inflamed, and swollen, causing discomfort when walking or wearing shoes.
Anatomy of a Bunionette Deformity
The anatomy of the bunionette deformity, also known as the tailor’s foot, involves specific structures in the foot. Let’s take a closer look at the main anatomical components of this condition:
Fifth metatarsal:
This bone connects the little toe to the midfoot and plays a crucial role in supporting the body’s weight during movement.
Metatarsal head:
The rounded end of the metatarsal bone articulates with the phalanges.
Bursa:
A bursa is a small fluid-filled sac located between the skin and the underlying bone. It acts as a cushion, reducing friction and pressure.
Protrusion of bone:
This is a feature of the bunionette deformity. This is a bony enlargement that forms on the outside of the foot at the base of the little toe. Bone spurs are a response to pressure, friction, and misalignment of the fifth metatarsal bone.
Soft tissues:
Muscles, tendons, and ligaments surroundings the 5th metatarsal and little toe are affected by the deformity and can contribute to pain and discomfort.
Joint Capsule:
The fibrous capsule surroundings the metatarsophalangeal joint, where the metatarsal bone connects to the proximal phalanx of the little toe.
- The appearance of the deformity is usually associated with mechanical tension and pressure on the outer surface of the foot, which leads to misalignment of the fifth metatarsal and the formation of a bony protrusion.
- It is important to note that the anatomy of a bunion deformity can vary from person to person, depending on the severity of the condition and the individual structure of the foot.
- If you suspect you have a sinus deformity or foot pain, it is best to see a physician who can perform a thorough examination and provide appropriate treatment options.
Epidemiology
Epidemiological studies focusing exclusively on bunionette deformities are relatively limited compared to studies on more common foot conditions such as bunions (hallux valgus). However, some general observations and information can be drawn from relevant studies and clinical experience:
Incidence:
Bunionette is less common than big toes. Hallux valgus (bunions) is estimated to affect about 23% of the adult population, but bunions are less common. The exact prevalence of bunion varies from region to region population and age groups.
Gender and age:
Deformities of both joints and tendons are seen more often in women than in men. The incidence tends to increase with age, with the highest incidence observed in older adults.
Footwear and lifestyle:
Factors such as footwear choice and lifestyle affect the incidence of muscle strains. Wearing narrow shoes and high heels can contribute to the development or worsening of the condition.
Genetics and foot structure:
There may be a genetic component to bunion development, as certain foot structures and biomechanics may predispose to the condition.
Occupational factors:
Tailors and people who work in occupations that involve prolonged standing or pressure on the side of the foot may have a slightly higher risk of developing tailor’s joints.
For the most up-to-date and accurate information on the epidemiology of bunion deformity, I recommend consulting a healthcare physician or seeking information from reputable health organizations.
If you are concerned about a knee deformity or any foot-related problem, it is recommended that you consult a qualified physician, such as a podiatrist, who can provide an accurate diagnosis and appropriate treatment plan.
Causes
Also known as tailor’s deformity or fifth metatarsal, impotence is usually caused by a combination of genetic factors and external influences. Below are some of the common causes of joint deformity:
Foot Structure and Genetics:
- Inherited foot structure and biomechanics can play an important role in limb development.
- People with certain foot shapes, such as a wider forefoot or a prominent fifth metatarsal, may be prone to this.
Shoes:
- Wearing ill-fitting shoes is a major factor in joint deformities.
- Shoes with narrow toes and high heels can squeeze the toes and put pressure on the outside of the foot, leading to misalignment of the fifth metatarsal and bone pronation.
Overpronation:
- Overpronation guides to exaggerated inward rolling of the foot during walking or running.
- This can increase pressure on the outer edge of the foot and help shape the limb.
Pressure and friction:
- Repetitive pressure and friction against the side of the foot, often caused by tight or ill-fitting shoes can cause irritation and inflammation of the fifth metatarsophalangeal joint and surrounding tissues.
Age and degeneration:
- As people age, the supporting structures of the foot, such as ligaments and tendons, can weaken and lose flexibility.
- This can contribute to misalignment and bunions of the fifth metatarsal bone.
Injury or trauma:
In some cases, a previous injury or trauma to the foot can cause changes in foot mechanics and increase the risk of bunion deformities.
Occupational factors:
Certain occupations that involve standing for long periods or putting pressure on the lateral aspect of the foot can contribute to bunions.
- It’s important to note that the exact cause of bunionette deformities can vary from person to person, and multiple factors may contribute to their development.
- Additionally, some individuals may be more genetically predisposed to developing foot deformities, including bunionette.
- If you suspect you have a bunionette deformity or are experiencing foot pain, it’s best to seek medical evaluation from a podiatrist or foot specialist who can provide a thorough examination and appropriate treatment options.
Symptoms of Bunionette deformity
Symptoms of bunionette, also known as tailor’s muscle or fifth metatarsal tendonitis, can range from mild to severe. The condition is characterized by a bony protrusion on the outside of the foot at the base of the little toe. Here are the typical symptoms associated with a bunion:
Bony lump:
- The most noticeable knee joint symptom is the formation of a bony lump on the outside of the foot near the base of the little toe.
- This lump is often red, swollen, and tender to the touch.
Pain:
- Pain is a common symptom of bunions.
- The pressure caused by the protrusion and misalignment of the fifth metatarsal bone can cause discomfort, especially when walking or wearing tight shoes.
Inflammation:
The affected area can become inflamed from friction and pressure, resulting in redness and swelling around the joint.
Difficulty with shoes:
Wearing shoes, especially shoes with narrow toes or heels, can aggravate the rabbit’s pain and discomfort. The bone spur can rub against the shoe and irritate it.
Corns and Calluses:
- Corns and calluses can form from increased pressure and friction on the rabbit, increasing discomfort. Limited toe movement:
- Movement of the fifth toe may be limited or difficult due to misalignment and swelling around the joint.
Bursitis:
In some cases, bursitis can develop in the bursa between the skin and the bone. Bursitis can cause more pain and swelling.
- It is important to note that bunions can vary in severity and some people may not experience significant pain or symptoms.
- However, if the disease is not treated or if the condition worsens, the symptoms may worsen over time.
- If you have any of these symptoms or suspect that you have a joint deformity, it is recommended that you see a podiatrist or podiatrist.
- They can provide an accurate diagnosis and recommend appropriate treatment options to relieve discomfort and prevent the progression of the deformity.
Metatarsalgia:
- Metatarsalgia refers to pain and inflammation in the foot that can be associated with bunions.
- A proper evaluation by a healthcare professional, often a podiatrist or orthopedist, can help differentiate these conditions and determine the most appropriate treatment plan.
- Diagnostic tools such as X-rays and other imaging studies can be used for differential diagnosis.
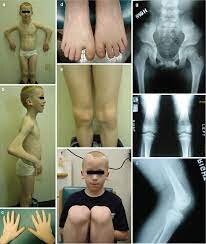
Diagnosing a Bunionette Deformity
Diagnosing a buninette deformity, also known as tailor’s or fifth foot muscle, usually involves a combination of a complete medical history, physical examination, and sometimes imaging studies. The diagnosis is usually made as follows:
Physician:
The healthcare provider begins by discussing the patient’s symptoms and medical history. They know about possible foot pain, swelling, difficulty in using shoes, and the duration of symptoms.
Physical Examination:
A full physical examination of the foot is performed. The healthcare provider will examine the affected foot and look for a visible bony elevation or swelling on the lateral side of the foot at the base of the little toe.
Palpate:
The doctor will palpate (touch and feel) around the fifth metatarsal joint to look for tenderness, inflammation, or bursitis.
Range of motion assessment:
The range of motion of the fifth toe and the affected joint is assessed to check for possible limitations of motion.
Shoe evaluation:
A healthcare provider can examine the patient’s shoes to determine if tight or ill-fitting shoes may be contributing to the problem.
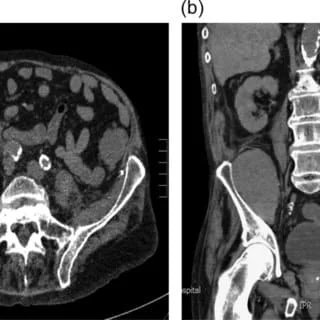
X-rays:
- In some cases, X-rays may be ordered to assess the alignment of the bones in the foot and determine the severity of the joint deformity.
- X- rays can also help rule out other foot conditions with similar symptoms, such as fractures or arthritis.
Differential diagnosis:
A healthcare provider will perform a differential diagnosis to rule out other conditions that may cause similar symptoms as mentioned in the previous answer.
- Based on the history, physical examination, and imaging findings, the healthcare provider can confirm the diagnosis of a joint deformity.
- The severity of the deformity is assessed and a treatment plan adapted to the specific needs and symptoms of the patient is recommended.
- If you suspect that you have humerus deformity or are experiencing foot pain, it is imperative to seek professional evaluation.
- A podiatrist or podiatrist is best able to accurately diagnose the condition and provide appropriate treatment options.
Treatment of Bunionette Deformity
Medical treatment for bunion deformities, also known as tailor’s foot or fifth metatarsal box, aims to relieve pain, reduce inflammation and improve the patient’s ability to walk comfortably. Although conservative treatments are often the first course of action, the effectiveness of these treatments can vary depending on the severity of the deformity and individual factors.
Here are some common treatments for joint deformity:
Shoe modification:
Wearing well-fitting shoes with a wider toe box can help reduce pressure on the bunion and improve comfort. Try to avoid wearing high heels and narrow toes of shoes are crucial to prevent further irritation.
Orthotic devices:
Custom orthotic inserts or cushions can be used to provide support and cushion, distribute pressure from the affected area and improve foot alignment.
Pain management:
Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, can help control pain and reduce inflammation.
Ice therapy:
Applying ice to the area of the swelling for 15 to 20 minutes several times a day can help reduce swelling and ease discomfort.
Injection therapy:
In some cases, corticosteroid injections may be given to reduce inflammation and relieve pain. However, repeated injections should be avoided as they can weaken the tissues.
Physical therapy:
Specific stretching and strengthening exercises for the foot and lower leg can improve foot mechanics, relieve pain and prevent progression of the deformity.
Padding and taping:
Using padding on the affected area can reduce friction and pressure. Bandaging the toe into an anatomically aligned position can also provide relief.
Shoe inserts:
Shelf cushions, pads, or splints designed to align the toes can help manage symptoms.
Shoe Stretching:
In some cases, shoe stretching techniques can help create more space in the toe box for the bunion.
- If conservative therapy does not provide adequate relief, or if bunionette deformity is severe and significantly affects the patient’s daily activities, surgery may be considered.
- Surgical options depend on the case and may include bone realignment, removal of bone exposure, and correction of soft tissue imbalances.
- It is important to consult with a podiatrist or podiatrist to determine an accurate diagnosis and individualized treatment based on the severity of the joint deformity and the specific needs of the patient.
- Early intervention and appropriate treatment can lead to better outcomes and a better quality of life.
Physiotherapy treatment
Physical therapy can play a supportive role in the treatment of a bunion deformity by helping to relieve pain, improve foot mechanics, and improve overall foot function. Here are some physical therapy procedures that can be helpful for people with joint deformities:
Manual therapy:
A physical therapist can use hands-on techniques such as joint mobilization and soft tissue manipulation to improve joint mobility, reduce stiffness, and relieve tension around the affected area.
Joint mobilizations
- Ankle mobilization is a manual therapy technique used by physical therapists and other health professionals to improve joint mobility, reduce stiffness and relieve pain in the foot and ankle area.
- The goal of joint mobilization is to restore normal joint motion, promote proper alignment, and improve overall foot function.
- It is commonly used to treat a variety of foot conditions, including bunions, plantar fasciitis, ankle sprains, and osteoarthritis.
- During ankle mobilization, the therapist applies gentle, controlled forces to the affected joint or joints. These techniques may include:
Oscillating movements:
The therapist applies rhythmic, repetitive movements to the joint, which helps reduce stiffness and improve joint mobility.
Grade I mobilizations (sliding): This involves gentle, low-amplitude gliding movement of the joint within its painless range of motion.
Grade II mobilizations (grip): Traction involves a slight increase in sliding force to stretch the joint capsule and surrounding soft tissues.
Level III mobilizations (joint play): The therapist uses moderate force to induce joint movements beyond the patient’s passive range of motion.
Level IV mobilizations (manipulation): This technique involves high-speed, low-amplitude thrusts on the joint to restore normal joint mechanics.
- Manipulations are usually performed by qualified specialists, such as chiropractors.
- The choice of mobilization technique and the force used depends on the specific condition of the patient, the severity of the problem, and the judgment of the therapist.
- The overall goal is to reduce pain, improve joint function and facilitate better movement patterns.
- It is important to note that ankle mobilization is performed by a qualified and trained health professional, such as a physical therapist or chiropractor.
- Self-mobilization attempts can be dangerous and cause further injury.
- Mobilization is usually part of a comprehensive treatment plan, which may also include stretching, strengthening exercises, and other techniques that can effectively treat foot problems.
- If you have foot pain or a foot-related condition, consult a doctor for proper evaluation and personalized treatment.
Soft tissues manipulation
- Ankle mobilization is a manual therapy technique used by physical therapists and other health professionals to improve joint mobility, reduce stiffness and relieve pain in the foot and ankle area.
- The goal of joint mobilization is to restore normal joint motion, promote proper alignment, and improve overall foot function.
- It is commonly used to treat a variety of foot conditions, including bunions, plantar fasciitis, ankle sprains, and osteoarthritis.
During ankle mobilization, the therapist applies gentle, controlled forces to the affected joint or joints. These techniques may include:
Oscillating movements:
The therapist applies rhythmic, repetitive movements to the joint, which helps reduce stiffness and improve joint mobility. Performed the same as mobilization techniques.
- Manipulations are usually performed by qualified specialists, such as chiropractors.
- The choice of mobilization technique and the force used depends on the specific condition of the patient, the severity of the problem, and the judgment of the therapist.
- The overall goal is to reduce pain, improve joint function and facilitate better movement patterns.
- It is important to note that ankle mobilization is performed by a qualified and trained health professional, such as a physical therapist or chiropractor.
- Self-mobilization attempts can be dangerous and cause further injury.
- Mobilization is usually part of a comprehensive treatment plan, which may also include stretching, strengthening exercises, and other techniques that can effectively treat foot problems.
- If you have foot pain or a foot-related condition, consult a doctor for proper evaluation and personalized treatment.
Stretching exercises:
Special stretching exercises may be prescribed to improve the flexibility of the toes, ankles, and calf muscles. These stresses can help reduce pressure on the rabbit and promote better leg function.
Stretching the muscles of the ankle, toe, and calf is important to maintain flexibility, prevent injury and promote overall foot health. Here are some effective stretches for these areas:
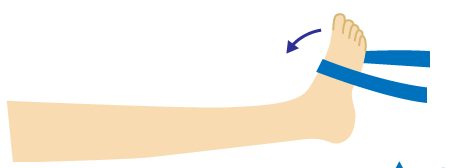
Ankle dorsiflexion stretching:
- Start with sitting or standing with one leg extended in front of you. Bend the leg up, bringing the toes to the calf.
- Gently pull your toes toward your calf with your hand until you feel a stretch in front of your ankle.
- Maintain the stretch for 10-20 seconds and repeat 2-3 times on both legs.
Plantar fascia stretching:
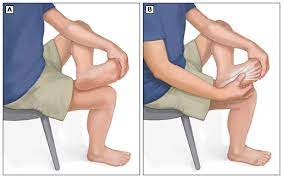
- Start with sitting with one leg crossed over the opposite knee.
- Grab the toes and gently pull them back toward your calf until you feel a stretch in the bottom of your calf.
- Maintain the stretch for 10-20 seconds and repeat 2-3 times on both legs.
Toe extension:
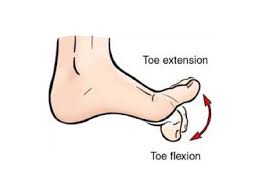
- Start with sitting with one leg stretched out in front of you.
- Cross the leg over the opposite knee.
- Gently press the toes with your fingers, extending them away from the foot.
- Maintain the stretch for 10-20 seconds and repeat 2-3 times on each leg.
Gastrocnemius Stretch:

- Stand against a wall with your hands against it.
- Step one foot backward, keeping the heel on the ground.
- Flex the front knee and keep the other leg straight. Lean forward slightly to feel the stretch in the calf of the back leg.
- Maintain the stretch for 10-20 seconds and repeat 2-3 times on each leg.
Soleus Stretching:
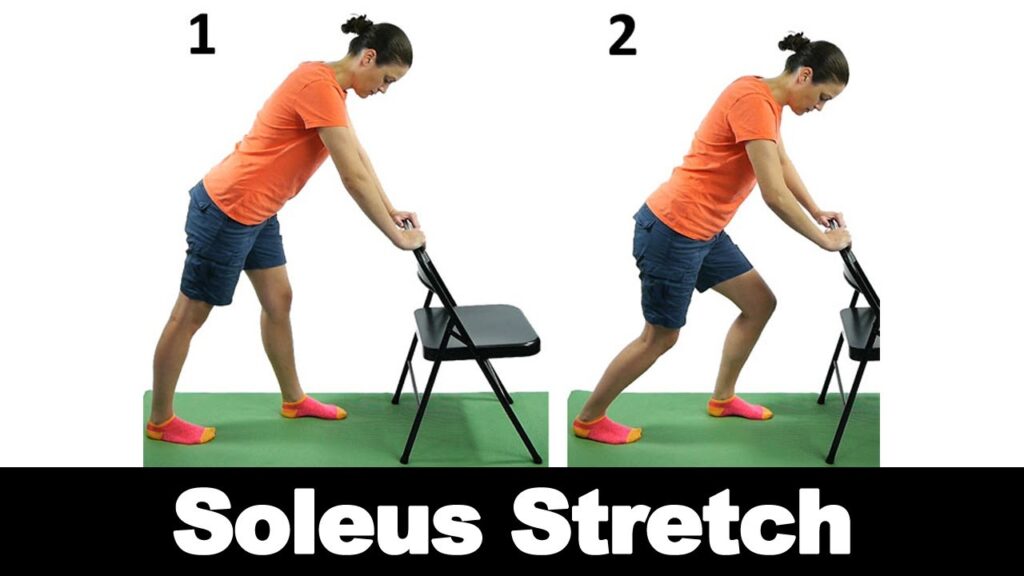
- Take the same position as the gastrocnemius stretch.
- Bend the back knee slightly, keeping the heel on the ground.
- Lean forward, and feel the stretch in the lower leg.
- Maintain the stretch for 10-20 seconds and repeat 2-3 times on both legs.
Achilles tendon stretch:

- Start with standing with one foot forward and the other behind.
- Bend both knees slightly.
- Bend forward, keeping the back on the ground, until you feel a stretch in your Achilles tendon.
- Hold the stretch for 10-20 seconds and repeat 2-3 times on both legs.
- Regular stretches can improve flexibility, reduce muscle tension and maintain proper foot mechanics.
However, it is important to stretch easily and in painless movements. If you have a foot or lower leg condition or experience pain while stretching, talk to a doctor or physical therapist before starting a stretching program. They can offer guidance and tailor a stress routine to your needs.
Strengthening exercises:
Strengthening the foot and calf muscles can provide better support and stability to the foot. Exercises
targeting the inner leg muscles can help maintain proper foot alignment. Strengthening the leg and calf muscles is critical to improving foot stability, balance, and overall foot function. Strong leg and foot muscles can also help prevent injury and provide better arch support. Here are some effective leg and calf strengthening exercises:
Toe curls:
- Start with sitting in a chair with your feet on the floor.
- Slowly bend his toes, trying to keep the floor under them.
- Keep the contraction for a few seconds and then release.
- Repeat 10-15 times.
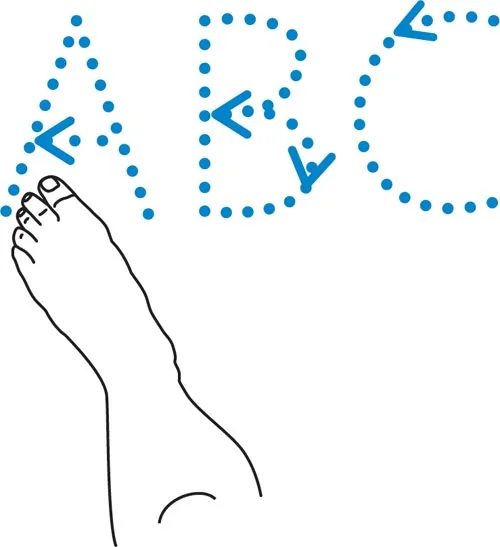
Ankle Alphabet:
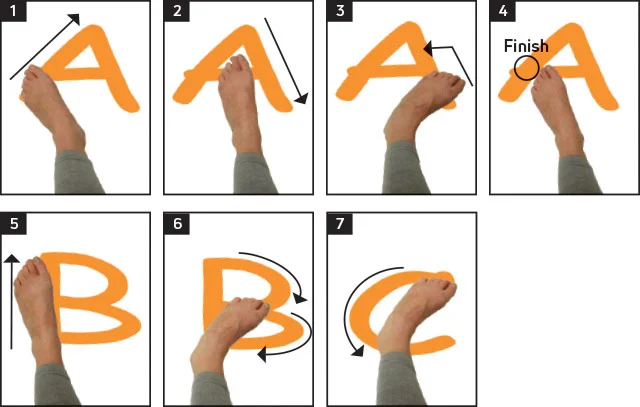
- Sit or lie with one leg extended.
- Imagine that your big toe is a pencil and “write” the alphabet in the air with your foot.
- Finish the whole alphabet on both legs.
Heel lift:

- Begin with standing with the feet shoulder-width apart.
- Gradually rise to the toes and lift the heels off the ground.
- Keep the position for a point and then lower the heels back down.
- Repeat -1o times.
Foot tapping:
- Start with sitting in a chair with your feet on the floor.
- Lift your toes off the ground, keeping your heels in place.
- Tap your toes repeatedly on the floor for 20-30 seconds.
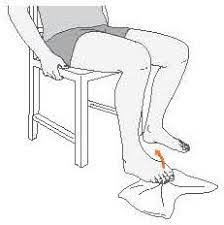
Resist ankle rotation:
- Sit in an armchair that is tied around your leg.
- Hold the ends of the tape with your hands.
- Move your foot inward (inversion) against the resistance of the strap and then outward (turn).
- Repeat 10-15 times with each leg.
Calf Raise:

- Stand with your feet shoulder-width apart, facing a wall, or holding on to strong support.
- Stand on the toes and gradually lift the heels off the ground.
- Slowly lower your heels back down.
- Repeat 10-15 times.
Towel curls:
- Sit on a chair with a small towel on the floor before you.
- Place your feet on the towel and curl the towel toward you with your toes.
- Repeat 10 -15 times with each leg.
- Do these exercises regularly, at least 2-3 times a week, to strengthen your legs and calf muscles.
Start with a manageable number of repetitions and gradually increase as the exercises improve. If you have foot problems or concerns, consider consulting a physical therapist or doctor before starting a strengthening program to make sure it’s safe and appropriate for your specific needs.
Gait analysis:
- A gait analysis can assess how a person walks and identify abnormal foot mechanics or imbalances that may be affecting it. deformation of buns.
- Based on the analysis, the physical therapist can recommend corrective exercises or changes to improve walking mechanics.
Advice on footwear:
A physiotherapist can advise on suitable footwear that provides better support and adaptability deformation of buns.
Orthotics:
Custom orthotic inserts or orthotics may be prescribed to help align the foot, redistribute pressure and improve foot health.
Taping and Padding:
A physical therapist can use tapping techniques to support foot alignment and reduce pressure on the hamstrings. Padding or taping can also help protect the area from friction and irritation.
Balance and proprioception training:
Improving balance and proprioception (awareness of body position) can improve leg stability and reduce the risk of falls or injury.
Education:
A physical therapist can teach self-management strategies, including home exercises, proper footwear choices, and lifestyle changes to effectively manage symptoms.
- It is important to note that physical therapy alone may not completely correct the joint deformity, especially in severe cases.
- However, when combined with other conservative treatments or post-operative rehabilitation, physiotherapy can significantly improve leg function, reduces pain, and prevents the progression of the disease.
- As with any condition, it is important to consult with a qualified physical therapist or podiatrist to develop an individualized treatment plan tailored to your specific needs and condition.
FAQ
Heredity, arthritis, or misalignment of the foot may cause bunions and bunionette. The most common cause, however, is footwear that squeezes the toes into pointy or narrow toe boxes, forcing the toes to fold over each other to fit in.
Bunionette surgery is usually an outpatient, so you can be discharged at the same time as your operation. This involves the removal of the bunionette’s bony prominence.
Wear shoes with a large toe box, a low heel, and a soft sole. Bunion discomfort is usually eased by wearing larger shoes with more toe space and utilizing other easy therapies to relieve strain on the big toe.
Consider bunion pads.
Keep an ice pack handy.
Take paracetamol or ibuprofen as needed.
Make an effort to lose weight.
Bunion surgery has always been unpleasant and time-consuming. Some patients, however, may benefit from newer, less intrusive treatments that provide considerable advantages.
Recovering from the osteotomy may take up to 8 weeks, and it is suggested not to commit to exercise while weight-bearing for 4 to 6 weeks.