THORACIC DISC SYNDROME : Physiotherapy Treatment
Table of Contents
What is thoracic degenerative disc disease ?
Thoracic degenerative disc disease (TDDD) is a condition that causes the discs between the vertebrae in the upper part of the spine to wear out. It can cause pain, numbness, and other symptoms that affect movement. Thoracic degenerative disc disease is one of several types of degenerative disc disease (DDD).
Thoracic degenerative disc disease is a condition in which the intervertebral discs in the thoracic spine (the middle section of the spine) degenerate and become damaged.
This condition usually occurs due to a combination of factors, including age, injury, and genetics. When these discs degenerate, they can cause a variety of symptoms, including pain, numbness, and weakness.
The discs are made of two thick layers of fibrous tissue that are embedded with a gel-like substance. These discs have a very important function because they separate the bones in the spine which are held in place by the discs. The discs act like shock absorbers when the spine bends and straighten, and they also cushion the bones when a person moves from an upright standing position to one where their spine is bent to the side. When the discs in the thoracic area of the spine degenerate, pain can occur, but this is not the only symptom of this condition. These discs are essential to the proper functioning of the spinal column as they allow for the transfer of weight and pressure, protect the spinal cord, and allow for the proper functioning of the bones and muscles in the upper body.
The damage may be accompanied or not by nerve root compression, and is characterized by neck and shoulder pain and backache. Most of the thoracic disc degeneration is caused by heavy lifting or improper lifting techniques. Over time, the discs degenerate and become weak. The result is increased stress on the ligaments and joints in the neck and back, causing pain.
DEFINATION:
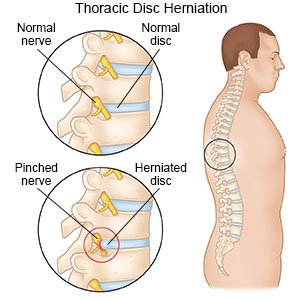
Thoracic discogenic pain syndrome may be a radicular or myelopathic pain. The radicular pain is mostly secondary to posterolateral herniations that compress spinal nerves as they exit through the intervertebral foramen.Symptomatic thoracic discogenic pain syndrome (TDPS) is a rare phenomenon making it challenging to diagnose. The rarity of TDPS is attributed to the particular orientation, structure, and function of the thoracic spine in the vertebral column.
The lordotic nature of the cervical and lumbar spine allows the imaginary line of gravity to run through, allowing them to bear most of the weight of the of the axial skeleton as compared to the thoracic and sacral spine.
Consequently, they are subject to a higher percentage of degenerated discs and subsequent discogenic pain syndrome.The majority of the thoracic disc herniation is asymptomatic, or the patient presents with nonspecific symptoms like chest wall pain, epigastric pain, upper extremity pain, and sometimes, a pain in the groin or the lower extremity.
While the rare nature, coupled with the atypical presentation, may lead to delay in diagnosis. Treatment of thoracic discogenic pain syndrome is conservative but sometimes surgical. Surgical interventions, with surgical intervention associated with many complications.
Pathophysiology
Thoracic discogenic pain syndrome may be a radicular or myelopathic pain.
The radicular pain is mostly secondary to posterolateral herniations that compress spinal nerves as they exit through the intervertebral foramen. Radicular pain will usually radiate towards the dermatome of the nerve roots innervated by the exiting nerve.
Myelopathic pain is seen in central herniations. The herniated disc compresses the spinal cord, leading to sensory and/or motor problems in the corresponding compressed area and below. This is particularly more severe in the thoracic spinal cord since the spinal canal in this region is smaller compared to the cervical and lumbar region. Hence, a slight compression will lead to symptoms.
Which are the causes of Thoracic Disc Syndrome ?
Intervertebral disc degeneration primarily causes thoracic discogenic pain syndrome.Thoracic disc lesions are primarily degenerative of nature and affect mostly the lower part of the thoracic spine. Three quarters of incidence occurs below T8, with T11-T12 being most common. The exact cause of disc degeneration is believed to be multifactorial, factors that can attribute include:
- Trauma
- Metabolic abnormalities
- Genetic predisposition
- Vascular problems
- Infections
The effects of trauma as previously mentioned is less devasting on the thoracic spine as compared to the cervical and lumbar spine because the thoracic spine participates in less weight-bearing activities and the rib cage and coronal orientation of the facet joints make it more stable, hence less prone to degenerative disc disease. With trauma, chronic overload from the lifting of heavy objects or chronic multi-trauma from individuals participating in sports leads to the repeated rotation of the axial spine, causing vertebral instability with alteration of the of the spinal alignment that accelerates the risk of developing disc degeneration.
Epidemiology
Why clinically significant thoracic disc disease is less common, has essentially two causes:
As opposed to the cervical or lumbar spine, the intervertebral foramina of the thoracic spine are located at the level of the body, as opposed to directly behind the discs.
There is relatively little movement in the thoracic motion segments, so the anatomical relationship of neural structures to their surroundings remains constant.
Thoracic disc herniation is rare and usually asymptomatic.
Often found incidentally with MRI.
Herniation of the intervertebral disc in the thoracic region makes up:
- 0.5% to 4.5% of all disc ruptures
- 0.25-0.75 of all symptomatic disc herniation
- 0.15% and 1.8% of all surgically-treated herniations.
- About 80% of patients usually present with problems in the third or fourth decades of life.
About 75% incidence occurs below the T8 with a peak around the T11 to T12 and about 63% are symptomatic and have an incidence of one in one million.
Note – in acquired deformities of the spine eg scoliosis, Scheuermann disease (which develop gradually) the nerve roots to adapt to the situation not necessarily causing thoracic syndrome.
Thoracic disc degeneration symptoms
The majority of the thoracic disc herniation are asymptomatic and are discovered incidentally with an MRI.Unlike the lumbar and cervical disc herniations, thoracic disc herniations have atypical symptoms and often a diagnosis of exclusion.
To accurately diagnose thoracic discogenic pain syndrome, a thorough history and physical examination should be done.
As part of the patient’s pain evaluation, assessment of the quality, intensity, distribution, alleviating, and aggravating factors is essential.
Degenerative thoracic syndromes can be classified as local, radicular (intercostal neuralgia) or pseudoradicular.
Patients with thoracic disc herniations may either present with a radicular and/or myelopathic pain depending on if the herniated disc compresses the nerve roots or the spinal cord itself, respectively. Dermatomes Grant.pngWith radicular pain, the patients will have pain that follows the dermatomal distribution.Essential landmarks for thoracic disc herniations to help with assessment include
- T-1 pain that radiates to the medial forearm,
- T-2 pain that radiates to the axilla,
- T-4 pain that radiates to the nipple area,
- T-10 pain that radiates to the umbilicus
- T-12 pain that is just above the inguinal ligaments.
- The most common initial pain is usually thoracic pain occurring in the midline area.
The pain may be:
unilateral or bilateral depending on the location and how significant the herniation is.intermittent and aggravated by coughing and straining.
In rare cases, radiation to the groin, flank, and even the lower extremities.
In upper thoracic and lateral disc herniations Radicular pain is more common and often reported in combination with some amount of axial pain. Sensory changes (e.g. parenthesias, dysesthesia) below the level of the lesion.Other symptoms include bladder and bowel dysfunction (15-20% of patients), hyperreflexia and gait impairment.
Red flags one should be aware of are:
- Myelopathy (injury to the spinal cord due to severe compression)
- Gait disturbance
- Paralysis
- Cardiovascular disturbances
- History of:Cancer; Trauma; Tumor; Infection; Constitutional symptoms (feeling ill); Weight loss; Laboratory abnormalities
Differential Diagnosis
Thoracic disc syndrome are relatively rare Symptoms in this area will more likely arouse suspicion of disease of the internal organs/ primary disorder of the nervous system. Important that the patient is examined thoroughly to rule out all other causes for symptoms. Rule out conditions such as
- Diabetes and shingles
- Other mechanical issues such as oblique muscle pain, rib fracture, fracture of the facet joints and clavicle
- Malignancies, like neurofibroma
- Herpes zoster (can cause segmentally radiating pain with postherpetic neuralgia)
- Costotransverse joint syndrome due to inflammatory changes or arthrosis
- Infections, tumors and dilated arteries of the chest wall Referred pain from the organs (zones of Head)
- Tietze syndrome
- Scheuermann kyphosis Pain referred around the chest wall tends to be costovertebral in origin.
PHYSICAL EXAMINATION
Start your examination with: History eg Chronic or acute, Specific inciting incident, Location of the pain and its radiation, The character of the pain and aggravating activities including static and dynamic load.
Observation (standing) Examination
Assessment of sensation with pinprick and touch in the upper extremity, thorax, and abdomen in the dermatomal
regions mentioned above to check for radiculopathy and also in the lower extremity to check for myelopathy.
Active movements (standing or sitting) – Forward flexion – Extension – Side flexion (left and right) – Rotation (left and right) – Combined movements (if necessary) – Repetitive movements (if necessary) – Sustained postures (if necessary)
Passive movements (sitting) – Forward flexion – Extension – Side flexion (left and right) – Rotation (left and right) –
Resisted isometric movements (sitting) – Forward flexion – Extension – Side flexion (left and right) – Rotation (left and right)
Functional assessment)
1) Special tests (sitting)
- adson’s test
- Costoclavicular maneuver
– Hyperabduction (EAST) test
– Roos test
2) Special tests (supine lying)
– First rib mobility
– Rib springing
– Upper limb neurodynamic (tension) test 4 (ULNT4)
– Federung test (segmental translation of the thoracic vertebrea) Sensitivity of the thorax and stomach After any assessment, the patient should be warned of the possibility of exacerbation of symptoms as a result of assessment.
Assess passive movements of the thoracic spine and the end feel:
• Forward flexion (tissue stretch)
• Extension (tissue stretch)
• Side flexion, left and right (tissue stretch)
• Rotation, left and right (tissue stretch)
Pain provocation by performing passive movements, in particular rotation, forward flexion, backward flexion and lateral flexion can indicate a spinal aetiology. Sensory symptoms can be present if the patient has a thoracic disc herniation. It can cause altered sensation to light touch or pinprick along a dermatomal pattern. Cord compression and myelopathy should be strongly considered if a sensory level is established such that sensation is consistently altered below a specific dermatome. Provocative manoeuvres such as the Spurling manoeuvre (cervical radiculopathy) and the Straight-Leg Raise test or the
Slump Test (lumbosacral radiculopathy) may exclude a thoracic disc syndrome.
Evaluation
In addition to a detailed neurological examination, an MRI of the thoracic spine is very sensitive and specific for diagnosing thoracic disc herniation. In some situations, thoracic discography can be performed to confirm the pain being of discogenic origin being that most thoracic discogenic syndrome can be asymptomatic.
Thoracic degenerative disc disease treatment
1) Medical Treatment :
- Over the counter medications for mild to moderate pain.
- Narcotics, if over the counter medications are not effective your physician may prescribe stronger pain medication.
- Anti-inflammatory drugs or prescription NSAIDS to reduce inflammation following acute injury.
- Muscle relaxers to reduce acute muscle spasm.
- Nerve pain medication by prescription, designed specifically to reduce pain from nerve damage.
- Injections like facet injections, nerve blocks or an epidural. These may involve the injection of corticosteroids to a specific structure to reduce local inflammation. Severe or Non-responsive Disc Conditions
The majority of thoracic disc herniations can be treated successfully without surgery. - In the case of conditions that do not respond to conservative care, surgery may be indicated. If you continue to experience some of the following symptoms:
- Increase in radiating or radicular pain
- Pain or nerve damage that gets worse
- The development of or an increase in weakness
- Increase in numbness or parasthesia
- Medical Proced Injections like facet injections, nerve blocks or an epidural. These may involve the injection of corticosteroids to a specific structure to reduce local inflammation.
- Caudal Epidural Injections
- Facet Joint Injections
- Interlaminar Caudal Epidural Steroid Injections
- Transforaminal Epidural Injections
- Selective Nerve Root Blocks
- Medial Branch Blocks
*Surgical Procedures
- Endoscopic Decompression
- Endoscopic Foraminotomy
- Percutaneous Decompression
- IDET Intradisc
- Eletrothermal Therapy
- Selective Endoscopic Discectomy
- Spinal Cord Stimulator
- Radiofrequency Ablation
- Epidural Lysis of Adhesions
PHYSIOTHERAPY TREATMENT
Physical therapy often plays a important role in Thoracic disc degeneration recovery. Its methods not only offer immediate pain relief, but they also teach you how to condition your body to prevent further injury.
There are a variety of physical therapy techniques. Passive treatments relax your body and include deep tissue massage, hot and cold therapy, electrical stimulation (eg, TENS), and hydrotherapy.
IFT (Interferential Therapy) :
IFT (Interferential Therapy) treatments relieve your body pain and include deep tissue massage and electrical stimulation (eg, TENS).

Your physical therapy program will usually begin with passive treatments. But once your body heals, you will start active treatments that strengthen your body and prevent further pain. Your physical therapist will work with you to develop a plan that best suits you.
Transcutaneous electrical nerve stimulation (TENS):
A TENS machine uses an electrical current to stimulate your muscles. It sounds intense, but it really isn’t painful. Electrodes taped to your skin send a tiny electrical current to key points on the nerve pathway. TENS reduces muscle spasms and is generally believed to trigger the release of endorphins, which are your body’s natural pain killer.
Passive Physical Treatments for Thoracic Disc Degeneration :
Deep Tissue Massage:
There are more than 100 types of massage, but deep tissue massage is an ideal option if you have a herniated disc because it uses a great deal of pressure to relieve deep muscle tension and spasms, which develop to prevent muscle motion at the affected area.
Hot and Cold Therapy:
Both hot and cold therapies offer their own set of benefits, and your physical therapist may alternate between them to get the best results.

Your physical therapist may use heat to increase blood flow to the target area. Blood helps heal the area by delivering extra oxygen and nutrients. Blood also removes waste byproducts from muscle spasms.
Conversely, cold therapy (also called cryotherapy) slows circulation. This reduces inflammation, muscle spasms and pain.
Your physical therapist may place an ice pack on the target area, give you an ice massage, or even use a spray known as fluoromethane to cool inflamed tissues.
Hydrotherapy:
As the name suggests, hydrotherapy involves water. As a passive treatment, hydrotherapy may involve simply sitting in a whirlpool bath or warm shower. Hydrotherapy gently relieves pain and relaxes muscles.
Active Treatments :
Active treatments help address flexibility, posture, strength, core stability, and joint movement. An exercise program may also be prescribed to achieve optimal results. This will not only curb recurrent pain but will also benefit your overall health. Your physical therapist will work with you to develop a program based on your specific diagnosis and health history.
Core stability exercise:
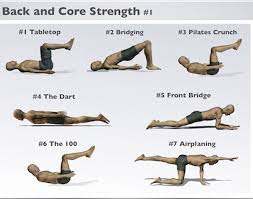
Many people don’t realize how important a strong core is to their spinal health. Your core (abdominal) muscles help your back muscles support your spine. When your core muscles are weak, it puts extra pressure on your back muscles. Your physical therapist may teach you core stabilizing exercises to strengthen your back.
Stretching exercise :
Learning proper stretching and flexibility techniques will prepare you for aerobic and strength exercises. Flexibility helps your body move easier by warding off stiffness.
Hydrotherapy :

: In contrast to simply sitting in a hot tub or bath like its passive counterpart, active hydrotherapy may involve water aerobics to help condition your body without unnecessary stress.
Muscle strengthening:
Strong muscles are a great support system for your spine and better handle pain.Your physical therapist will teach you ways to condition and strengthen your back to help prevent future pain. You may learn self-care principles so you understand how to best treat your symptoms. The ultimate goal is for you to develop the knowledge to maintain a pain-free lifestyle.
It’s essential that you learn how to exercise and condition your back after the formal physical therapy ends. If you don’t implement the lessons you learned during physical therapy, you won’t enjoy its long-term results. By taking care of your back .