Elephantiasis
Table of Contents
What is an Elephantiasis?

- Elephantiasis is the enlargement and hardening of limbs or body parts due to tissue swelling.
- It is characterised by oedema, hypertrophy, and fibrosis of skin and subcutaneous tissues, due to obstruction of lymphatic vessels.
- Elephantiasis, also known as lymphatic filariasis, is a very rare condition that’s spread by mosquitoes.
- It may affect the genitalia.
- The term elephantiasis is often used in reference to parasitic worm infections, but may refer to variety of diseases where parts of a person’s body swell to massive proportions
- The common name is often used because if you have it, your arms and legs can swell and become much bigger than they should be.
- Your sex organs and breasts may also swell up.
- The affected skin can thicken and harden to look something like an elephant’s skin.
- It’s more common to people who live in tropical or subtropical areas.
- If you have it, there are medicines and treatments to help with the swelling and discomfort.
Pathophysiology
- Usually, to get elephantiasis, you would have to be bitten by a lot of mosquitoes over a long time, in a country where certain types of roundworms are known to exist.
- It starts when mosquitoes infected with the roundworm larvae bite you.
- The tiny larvae survive in your bloodstream and grow.
- They finish maturing in your lymph system. They can live there for years and cause a lot of damage to your lymph system.
- This is what causes the swelling.
- Lymphatic filariasis is caused by three types of microscopic, thread-like worms, namely Wuchereria bancrofti, Brugia malayi, and Brugia timori.
- The overwhelming majority of cases (90 percent) are due to Wuchereria bancrofti.
Causes of Elephantiasis
Some conditions that present with elephantiasis include:-
- Elephantiasis nostras, due to longstanding chronic lymphangitis
- Elephantiasis tropica , caused by a number of parasitic worms, particularly Wuchereria bancrofti. More than 120 million people, mostly in Africa and Southeast Asia, are affected.
- Nonfilarial elephantiasis , an immune disease affecting the lymph vessels
- Leishmaniasis
- Elephantiasis, Grade 3 lymphedema which may occur in people with breast cancer
- Genital elephantiasis, end result of lymphogranuloma venereum[citation needed]
- Proteus syndrome, a genetic disorder. A notable sufferer of Proteus syndrome was the so-called Elephant Man
Other causes may include:-
- Repeated streptococcal infection
- Lymphadenectomy
- Hereditary birth defects
- Pretibial myxedema
Risk factors:
Elephantiasis can affect anyone who is exposed to the parasites that cause the disease.The risk of exposure is greatest for people who:-
- live long-term in tropical and subtropical regions are regularly bitten by mosquitoes
- live in unhygienic conditions
- The regions where these roundworms are found include:-
- Africa
- India
- South America
- Southeast Asia
Living With Elephantiasis:
Elephantiasis can be disabling. Sometimes it’s hard to move the affected body parts, which means it could be difficult to work.
It might even be hard to get around in your home.
You might also worry about how your condition looks to other people.
This can cause anxiety and depression. If you have elephantiasis and want information about support groups, ask your doctor.
You can also go online to find resources that might help.
Symptoms of Elephantiasis
- You may not know you have elephantiasis until you notice the swelling.
- Not only will those body parts begin to look bulky and lumpy with stiff, tough skin, there is also pain in the swollen area.
- You may also have chills, fever, and just feel bad all over
- Most cases of lymphatic filariasis infection don’t have any symptoms at all.
- Those infected with the microscopic worms likely aren’t aware that they are infected, but they can still pass on the parasite to others.
- When symptoms do occur (often years later), they can lead to extensive disfigurement and disability.
- These symptoms can last for weeks at a time and can be so debilitating that they keep people from working.
- The three most visible and concerning manifestations of lymphatic filariasis are lymphedema, elephantiasis, and hydrocele.
LYMPHEDEMA:

- While many people use lymphatic filariasis and elephantiasis interchangeably, it’s actually lymphedema that gives the appearance of more elephant-like features.
- Lymphedema is when there is intense fluid collection and swelling in parts of the body, most often in the legs, breasts, or genitals.
- This inflammation can sometimes be accompanied by fever and be quite painful.
- An estimated 15 million people currently live with lymphoedema worldwide, and the majority of those who develop this condition do so years after first becoming infected with the parasite.
Diagnosis:
- There are two primary ways lymphatic filariasis is typically diagnosed:-
- blood smears or
- assays.
- The worms can’t be seen by the naked eye, but you can catch a glimpse of them under a microscope.
- This diagnostic method uses a small amount of blood (taken by a finger prick, for example) smeared onto a slide, which is then looked at through a microscope.
- The worms are only active at night, so the sample should be taken then.
- This is the cheapest and more practical way to test for the parasite.
- Alternatively, serologic testing can also be used for diagnosis.
- When you’re infected with a parasite, the human body often makes antibodies to try to fight it off.
- These antibodies can be detected using routine assays done on blood samples.
- This method, however, tends to be used primarily by public health officials attempting to monitor and map the transmission of the parasite in a given region. Because many people don’t present symptoms until years after they’re infected, tests might come back negative even if their condition is the result of the parasite.
- Your doctor can find out if you elephantiasis by giving you a physical exam.
- She will ask about your medical history, and whether you’ve traveled to a place where you were more likely to have gotten elephantiasis.
- She also will have blood tests done to see if roundworms are in your bloodstream.
- These tests need to be done at night, because that’s when these parasites are active.
Nonspecific test abnormalities:
- Eosinophilia (>3000/microliter)
- Microscopic hematuria
- Microscopic proteinuria
Blood smears:
- Samples are drawn ideally between 10pm and 2am due to peak biting time of mosquito vectors
- 20 microliters of blood can detect microfilariae, but a 1 mL blood sample may be required to make a diagnosis
- >10,000 microfilariae per 1 mL of blood can be found in endemic regions
- Samples are stained and centrifuged
- Microfilariae species can be differentiated by morphological characteristics
Antibody tests:
- Serologic testing for filarial antibodies can detect elevated levels of IgG and IgE
- Poor specificity
- Cannot distinguish between filarial types
- Cannot differentiate between past and present infections
- Newer tests are being developed that look at specific anti-filarial IgG4 antibodies for showing active infections
Antigen tests:
- Detect the presence of adult worms
- Circulating Filarial Antigen (CFA) tests are considered the gold standard for diagnosing Wuchereria bancrofti infections
- No antigen testing currently available for Brugian malayi filariasis
Radiology:-
- Ultrasound can be used to detect adult worms and vessel destruction
- Ultrasound can localize worms in epididymal and breast lymphatics
- “Filarial dance”, or the constant movement of live worms, can be picked up with ultrasound imaging and is sometimes used to monitor effectiveness of certain treatments
- Lymphoscintigraphy is used for assessment of the extent of lymphatic destruction
- Elephantiasis:
- Elephantiasis is when the skin and underlying tissues become abnormally thick.
- This is often the result of secondary bacterial infections that happen because the body’s immune system is damaged due to the parasite.
- Hydrocele:-
- Some men infected with the parasite develop swelling in their scrotum.
- An estimated 25 million men worldwide are believed to have hydrocele as a result of lymphatic filariasis.
- Tropical Pulmonary Eosinophilia Syndrome
- This complication is generally found in infected individuals living in Asia, and consists of shortness of breath, coughing, and wheezing.
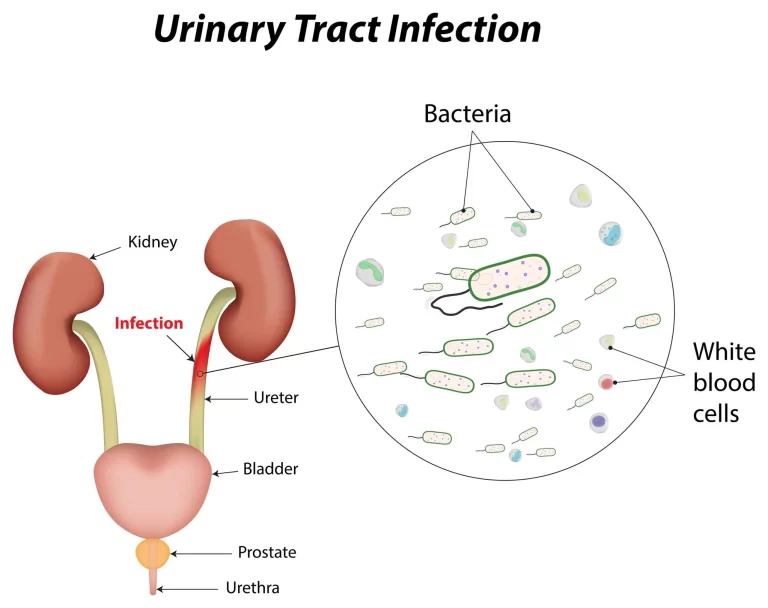
- TRANSMISSION:
- Much like malaria, these roundworms spread from person to person through mosquito bites.
- Several different kinds of mosquito species can transmit the parasite, including Anopheles and Aedes (which can transmit viruses like dengue and Zika).
- Mosquitoes aren’t just carriers, they’re also an important part of the worm’s life cycle.
- When the insects bite someone who is infected, they take in the immature larvae of the parasite (called microfilariae).
- For one to two weeks, the larvae go through a transformation inside the mosquito, and when the bug bites someone else, the now-infective larvae get transferred to the skin and make their way into the body.
- Once inside, the worms grow into adult worms and cluster in the lymphatic system, sending out microfilariae into the bloodstream, which can then be picked up by mosquitoes.
- And on and on it goes. This can happen even if someone doesn’t have any symptoms, and adult worms can live and reproduce inside the human body for six to eight years.
Treatment of Elephantiasis
Medications
- Several medications can be taken to kill the parasite’s microfilariae and some (though likely not all) adult worms.
- Side effects of the drugs can sometimes be worse if an individual has co-infections with other diseases, so different regions are recommended to receive different treatment combinations.
- These include:-
- Albendazole, on its own in areas with loiasis (or African eye worm)
- Ivermectin, which is primarily used with albendazole in areas with onchocerciasis (or river blindness)
- Diethylcarbamazine citrate, often used with albendazole in areas without onchocerciasis
- In certain areas without onchocerciasis, all three medications might be recommended.
- Some research also indicates that taking 200 milligrams a day of doxycycline can help kill adult worms, though it is not yet a first-line treatment option recommended by the World Health Organization.
- People with an active infection can take medications to kill the worms in the blood.
- These medications stop the spread of the illness to others, but they do not completely kill off all the parasites.
- Antiparasitic drugs that may be prescribed include:-
- diethylcarbamazine (DEC)
- ivermectin (Mectizan)
- albendazole (Albenza)
- doxycycline
- Other symptoms may be managed with:-
- antihistamines
- analgesics
- antibiotics
Other treatment
- Not everyone with elephantiasis will need medication.
- This is because they may no longer carry the worms in their system despite the presence of symptoms.
- People can manage the swelling and skin infections in these cases by:-
gently washing the swollen and damaged skin every day with soap and water
– moisturizing the skin
– elevating swollen limbs to improve the flow of fluid and lymph
– disinfecting wounds to prevent secondary infections
– exercising regularly to support the lymphatic system, as directed by a doctor
– wrapping the limbs to prevent further swelling, as instructed by a doctor - Surgery may be recommended in rare cases to remove damaged lymphatic tissue or relieve pressure in certain areas, such as the scrotum.
- Some people with elephantiasis may wish to seek emotional and psychological support in the form of
– individual counseling
– support groups
– online resources - During the onset of the ailment, it is best that early diagnosis be served.
- At the first stage of the infection, antibiotics could be prescribed by the doctors.
- The most common form of antibiotic suggested by doctors is doxycycline.
- This further kills the bactria that lives within the worms which means that the treatment affects the operational function of the foreign substances from the roots of the problem.
- This then slows down the growth of the worms likely weakening the capability of the worms to reproduce.
- Another possible prescription could include albendazole which is a combination of diethylcarbamazine and ivermectin.
- This medication is directed towards killing the spreading young worms that are expected to be released by the old worms which are likely the ones spreading in the affected area.
- These medications however cannot kill the full-grown worms hence making it hard for completely stopping the disease from spreading.
- In more serious cases, standard therapies could include chemotherapy which are designed to attack the adult worms hence serving as a symptomatic treatment that could repair the damage that the infection has already caused in the decay of the different parts of the body.
- Revitalizing the immune system through killing the foreign elements in the system could further increase the capability of the body to fight the effects of the impending infection from the worms.
- Along with the therapy comes the implication of applying medication that supports the process.
- During the current years of further research on the development of therapies that could provide more effective support for the need of the suffering patients to recover from the matter, it has been realized that a particular consideration on massage therapy could alleviate certain developmental progression of the infection.
- Strengthening the muscles of the infected area apparently also improves the process of protection that the lymphatic vessels establish against the impending effects of the worms in the system.
- physiotherapy in elephantiasis:-
- Lymphoedema is a high protein oedema caused by a low output failure of the lymphatic system.
- Complex Physical Therapy is a conservative treatment that is designed to increase the transport capacity of the lymphatic system and remove the stagnant plasma proteins from the tissues.
- The treatment consists of massage, compression bandaging, an active exercise programme and care of the skin.
- Sometimes this is assisted by the use of a mercury compression pump and the prescription of one of the benzo pyrone drugs by the referring medical officer.
- The treatment is given daily for one hour, six days a week, usually over four weeks. At the completion of treatment, the limb is fitted with support hosiery.
- Physical therapy management of the disease primarily consists of treatment from a lymphedema therapist, along with education of proper skin care and hygiene.
- Appropriate exercise prescription and wound care management are also indicated.
- There is no physical therapy intervention indicated for hydrocele; those infected usually do not respond well to DEC, and surgery is required in some cases
- Breathing exercise Purpose:- to increase chest wall mobility before removing the drainage tube
– Methods: deep breathing and pursed lip breathing exercises at least 6 times a day - Postsurgical positioning Purpose:- to reduce wound edema post surgery before removing the drainage tube
– Methods: keep the arm elevated above the heart - Massaging of scar tissue and stretching of the soft tissue Purpose:- to soften scar tissue
Methods: (1) use the pads of the fingers to massage the scar and the surrounding tissue in circular, vertical, and horizontal motions; and (2) passive and active stretching and transverse strain of the major and minor pectoral muscles
Duration: average 10–15 minutes - Mobilization of the shoulders :- to restore range of shoulder motion
– Methods: active or passive mobilization of the shoulders in all planes of motion, including flexion, extension, adduction, abduction, and internal and external rotation
– Duration: average 5–10 minutes per section - Clinical Care:
- Lymphedema management
- Wash and dry affected area twice daily
- Elevate lower extremities at night
- Exercise and move affected limb regularly
- Antibiotics/Topical medications for small wounds
- Comfortable shoes
Preventive Chemotherapy:
- To prevent the spread of lymphatic filariasis, a combination of medications are often given routinely and proactively to everyone in a given area—regardless of whether they have been diagnosed with the condition.
- While this won’t cure everyone who has lymphatic filariasis or its various complications, it can help prevent the spread of the parasite because it effectively eliminates the microfilariae that can be carried by mosquitoes and passed from person to person.
Vector Control:
- Mosquitoes are integral to the transmission of lymphatic filariasis, and other harmful pathogens like malaria, West Nile virus, and dengue fever, so reducing their populations and warding against bites is an important prevention strategy.
- This can be done by:
Using mosquito nets treated with insecticide
Spraying in and around residential areas
Wearing bug spray with DEET (if available) and long pants and sleeves - While this likely won’t eliminate lymphatic filariasis entirely, it can help reduce the chances someone becomes infected with the parasite. Coping:-
- The symptoms associated with lymphatic filariasis can often be excruciating, but they can be managed (or prevented entirely) with a few basic strategies:
- Practice good hygiene, including frequent hand-washing and cleaning affected areas with soap and water to prevent infections.
- Elevate swollen body parts.
- Do light exercise where you move the affected area.
- Wrap the swollen area snuggly with bandages to encourage the draining of fluids.
- Take any medication recommended by a health care provider exactly as prescribed.
- If you have lymphedema, these techniques may need to be used for the remainder of your life.
- Lymphatic filariasis is extremely rare in North America and Europe.
- In order to become infected with the parasite, you have to be bitten by infected mosquitoes repeatedly and over a long period of time.
- If you’re just making short-term trips to areas where lymphatic filariasis is common, there’s little reason to be concerned about getting sick from the parasite.
Prevention:
- The best way to prevent elephantiasis is to avoid mosquito bites.
- People who visit or live in countries at risk should:
– sleep under a mosquito net
– cover up their skin with long sleeves and trousers
– use insect repellent
- as of now, only the course of identifying the development of research on elephantiasis is considered to be the source of an ideal form of prevention.
- Increasing knowledge about this ailment hence equipping people with the idea on when to be checked for early diagnosis is exposed as the most effective source of prevention.
- Other than this, no vaccinations have been developed yet which means that it is only the occurrence of careful consideration upon one’s health that could protect one from incurring the ailment.
- Ones the ailment has already been developed, it is strongly advised that constant cleaning and of the area infected be imposed so as to prevent the distribution of the infection to other parts of the body.
- Like other ailments, it is also considered that early diagnosis of the disease could be the course taken into consideration hence lessening the health dilemma that shall affect the individual already suffering from the ailment. Preventing the infection from spreading is the primary course of defense that doctors suggest so as not to further deepen the effect of the said ailment on the individual.
- Prevention for travelers:
- Chronic conditions of LF is generally not a concern for those people who wish to visit endemic regions of the world because they do not stay long enough to accumulate a harmful amount of microfilariae, although the following mild, allergic-like symptoms have been – reported:- lymphangitis/lymphadenitis, urticaria (hives), rash, and peripheral eosinophilia.
- Recommendations for travelers are as follows:- wear long sleeves and long pants, sleep under a mosquito net or in air conditioning, use bug repellent, and stay indoors or away from mosquito breeding grounds between dusk and dawn (they’re preferred biting time)
Takeaway:
- Elephantiasis is a tropical disease spread through mosquito bites.
- People living in affected tropical or subtropical areas are most at risk of infection.
- However, short-term visitors to these regions have a very low risk of getting elephantiasis or related conditions, according to the CDC.
- People with symptoms of the condition, including swelling and skin thickening, should see their doctor immediately.
- Elephantiasis symptoms can be managed through medications, lifestyle changes, and emotional support.
How the Parasite Affects the Body:
- The reason the worms can be so destructive in the human body is because they make their home in the lymphatic system.
- This complex network of organs and tissues are responsible for, among other things, protecting the body from disease and regulating fluid in your tissues.
- In some cases, the swelling that takes place after a lymphatic filariasis infection is actually the result of our own body’s immune system trying to rid itself of the worm.
- Sometimes, however, the inflammation is caused by an opportunistic bacterial infection that the body’s immune system was too damaged to stop.
- These secondary infections are what causes the elephantiasis, or hardening of the skin and tissues.
- For these effects to happen, however, you have to be bitten by infected mosquitoes repeatedly, over the span of several months.
complications:
- Elephantiasis may cause anxiety about appearance.
- Elephantiasis may cause anxiety about appearance.
- Without medical treatment, the microscopic parasites may live for years in the lymphatic system, causing destruction and damage.
- The lymph system is responsible for transporting excess fluid and proteins and fighting infections.
- Fluid builds up when it does not function correctly.
- The accumulation of fluid leads to swelling of the tissue and reduced immune function.
- Elephantiasis is associated with several physical and emotional complications, including:-
- Disability:- Elephantiasis is a leading cause of permanent disability across the globe. It may be difficult to move the affected body parts, which makes working or engaging in household tasks more difficult.
- Secondary infections:- Fungal and bacterial infections are prevalent among those with elephantiasis because of damage to the lymph system.
- Emotional distress:- The condition can cause people to worry about their appearance, which could lead to anxiety and depression.
Differential Diagnoses
Most highly suspected causes of Lymphadenopathy:-
- Mononucleosis
- Epstein-Barr Virus
- Toxoplasmosis
- Cytomegalovirus
- HIV
- Cat-scratch disease
- Pharyngitis
- Tuberculosis
- Secondary syphilis
- Hepatitis B
- Lymphogranuloma venereum
- Chancroid
- SLE
- Rheumatoid Arthritis
- Lymphoma
- Leukemia
- Serum sickness
- Sarcoidosis
- Kawasaki disease
Systemic Involvement:
- Lymphatic:- Adult filariae can live in the lymphatic system for up to 7 years while continuing to reproduce, leading to obstruction of drainage and destruction of vessels.
- Renal:- Intestinal lymph fluid can be deposited into the renal pelvis and eventually make its way to the urine to be excreted by the body (chyluria). This can lead to hypoproteinemia, hematuria, and anemia as large amounts of fat and protein are lost through the urine and lymph fluid.
- Dermatological:- Pitting edema, hyperpigmentation, and hyperkeratosis are present as a result of the associated lymphedema. In severe cases, affected individuals develop elephantiasis.
- Reproductive:- In females, involvement of the breast tissue and ovaries (along with upper or lower limb edema) is not uncommon. In males, the genitalia can be severely affected. Unilateral or bilateral hydroceles in the scrotum (especially in the spermatic cord) can lead to disfigurement and loss of sexual function.
- Immune:- Other bacterial or fungal infections often develop as a secondary result of lymphatic filariasis, primarily due to excessive skin folds and skin tears.





I have no idea why you would write that it takes months or serveral bites to get infected? It takes ONE bite from a infected mosquito, thats it!