MEDIAL COLLATERAL LIGAMENT
The medial collateral ligament (MCL) is one of the four major ligaments in the knee, and it’s located on the inside of the knee. It is a thick band of connective tissue that runs from the medial epicondyle (the bony structure where the femur and tibia meet) to the medial condyle (the bony structure where the femur and fibula meet). The MCL’s main function is to prevent excessive lateral movement of the knee.
The MCL can be torn or stretched as a result of a direct blow or a force pushing against the outside of the knee, such as during an awkward landing.
Table of Contents
MEDIAL COLLATERAL LIGAMENT INJURY
An MCL injury is a sprain or tear to the medial collateral ligament. The MCL is a band of tissue on the inside of your knee. It connects your thighbone to the bone of your lower leg. Ligaments hold bones together and add stability and strength to a joint. The MCL keeps the knee from bending inward.
ANATOMY OF MCL
It is a broad, flat, membranous band, situated slightly posterior on the medial side of the knee joint. It is attached proximally to the medial epicondyle of the femur immediately below the adductor tubercle; below to the medial condyle of the tibia and the medial surface of its body. It resists forces that would push the knee medially, which would otherwise produce valgus deformity.

The fibers of the posterior part of the ligament are short and incline backward as they descend; they are inserted into the tibia above the groove for the semimembranosus muscle.
The anterior part of the ligament is a flattened band, about 10 centimeters long, which inclines forward as it descends.
It is inserted into the medial surface of the body of the tibia about 2.5 centimeters below the level of the condyle.
Crossing on top of the lower part of the MCL is the pes anserinus, the joined tendons of the sartorius, gracilis, and semitendinosus muscles; a bursa is interposed between the two.
MECHANISM :
Injury to the MCL often occurs after an impact to the outside of the knee when the knee is slightly bent. The ligament on the inside of the knee becomes stretched and if the force is great enough, some or even all of the fibres will tear. A grade one tear consists of fewer than 10% of the fibres being torn. A grade 2 sprain is upwards of 10% but not a complete tear of the ligament as in a grade 3.
The deep part of the ligament is prone to becoming damaged first which may lead to a medial cartilage meniscus injury. Twisting the knee can also cause a medial ligament sprain as well as the possibility of an ACL tear. If the foot is planted and the player tries to turn quickly this can also lead to stressing the joint causing the inside of the joint to open and tear the ligament.
CAUSES OF MCL INJURY
The MCL is injured when the (valgus) force is too great for the ligament to resist and the ligament is overstretched. This can occur through a sharp change in direction, twisting the knee whilst the foot is fixed, landing wrong from a jump, or the most common a blunt force hit to the knee, such as in football tackle. The incident usually needs to happen at speed. Muscle weakness or incoordination predispose you to a ligament sprain or tear.
SIGN & SYMPTOMS
- Tenderness on the inner part of the knee
- Bruising around the knee
- a popping sound upon injury
- Knee pain and tenderness along the inner part of your knee
- swelling of the knee joint
- a feeling that your knee is going to give out when you put weight on it
- locking or catching in the knee joint
- Knee joint Stiffness
CLASSIFICATION
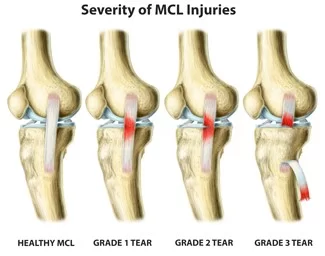
- Grade 1 — Some tenderness and minor pain.
- Grade 2 — Noticeable looseness in the knee when moved by hand; major pain and tenderness at the inside of the knee; swelling, in some cases.
- Grade 3 — Considerable pain and tenderness at the inside of the knee; some swelling and marked joint instability. The knee opens up about 1 centimeter (slightly less than half an inch) when the doctor moves your leg around. A grade 3 MCL tear often occurs along with a tear of the anterior cruciate ligament.
DIAGNOSIS
X-ray of the knee: Although MCL Injuries do not show up on x-rays, they can help rule out other causes of knee injuries and help confirm the diagnosis
Magnetic resonance imaging (MRI) of the knee: An MRI is a more detailed scan that uses a magnetic field to produce images, which allows a physician to view any damage to the bones and soft tissue to confirm the diagnosis
Ultrasound imaging of the knee: High-frequency sound waves are used to generate a more detailed image of the knee. This can help determine if any loose cartilage is caught in the knee

SPECIAL TEST:
The valgus stress test allows the therapist to examine the medial aspect of the joint for any laxity. An increase in laxity and joint space usually distinguishes damage to the medial collateral ligament. The patient should be positioned supine. By performing the test with the knee in approximately 30 degrees flexion rather than extension, this is due to the fact that flexion helps to relax surrounding structures including the posterior capsule.
This ensures there is isolated testing of the MCL. Therapists position one hand on the lateral aspect of the joint line of the knee with the other hand on the medial aspect of the ankle. A valgus force is then applied, a positive result of the knee in this position would be an increase in joint space medially.
MEDICAL TREATMENT
- Resting, icing, and elevating the knee (Use RICE Principle)
- Taking pain relievers, such as aspirin and ibuprofen, to ease pain and swelling
- Wearing a lightweight cast or brace that allows your knee to move backward and forward while restricting side-to-side movement. It usually is recommended to keep the knee immobilized like this for 72 hours, depending on the severity of the injury.
SURGERY
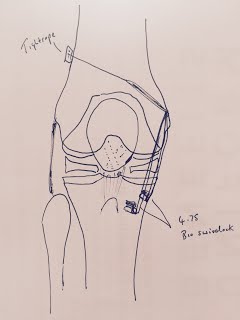
Knee arthroscopy:
Knee Arthroscopic surgery is a minimally-invasive surgical procedure that is used to visualize, diagnose, and repair the medial collateral ligament using small instruments. During this procedure, a surgeon inserts a thin tube attached to a camera (a fibro-optic camera) into the joint via a small incision on the skin of the joint. Visualizing the joint via a camera helps the physician view the inside of the knee and to determine the treatment
Knee ligament repair:
Knee ligament repair is a procedure to repair or replace the medial collateral ligament with surgery
PHYSIOTHERAPY TREATMENT
cryotherapy, laser, phonophoresis, hot packs: To reduce pain and to promote healing
Ultrasound- Ultrasound is often used in the conservative management of MCL sprains and is thought to increase blood flow to the area to promote healing and reduce pain.
Neuromuscular electrical stimulation to the quadriceps muscle may be used in order to reduce muscle atrophy.
EXERCISE THERAPY
STATIC QUADRICEPS EXERCISE

- Lie on your back with the leg you want to exercise straight.
- Place a small rolled towel underneath the knee. Slowly tighten the muscle on top of the thigh (quadriceps) and push the back of the knee down into the rolled towel.
- Hold the contraction for 5 seconds and then slowly release, resting 5 seconds between each contraction.
- Perform 3 sets of 10 repetitions, 1 time daily.
Sitting Quadriceps exercise
Seated with your knees bent, slowly extend your leg until it is straight, lined up with your thigh. Pause at the peak of the contraction for a few seconds. Control the movement as you slowly return the leg to the beginning position. An average set consists of 10 repetitions.
Straight leg raises
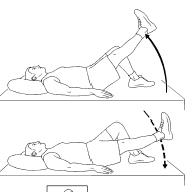
Lie on your back with your legs straight out in front of you. Bend the knee on your uninjured side and place the foot flat on the floor. Tighten the thigh muscle on your injured side and lift your leg about 8 inches off the floor. Keep your leg straight and your thigh muscle tight. Slowly lower your leg back down to the floor. Do 2 sets of 15.
SIDE ABDUCTION
Lie on your uninjured side. Tighten the front thigh muscles on your injured leg and lift that leg 8 to 10 inches (20 to 25 centimeters) away from the
other leg. Keep the leg straight and lower it slowly. Do 2 sets of 15.
PRONE SLR
Lie on your stomach with your legs straight out behind you. Fold your arms under your head and rest your head on your arms.
Draw your belly button in towards your spine and tighten your abdominal muscles. Tighten the buttocks and thigh muscles of the leg on your injured side and lift the leg off the floor about 8 inches. Keep your leg straight. Hold for 5 seconds. Then lower your leg and relax. Do 2 sets of 15.
HAMSTRING CURLS

Position yourself on your stomach, on a bench or bed, with your legs straight, knees extended and feet flexed.
Keeping your pelvis pressed down, slowly bend your knees, bringing your heels toward your buttocks. Pause at the top of the contraction for a few breaths. Slowly return your legs to fully extended, controlling the movement all the way down. A set of 10 repetitions should be easy to complete.
HEEL RAISES
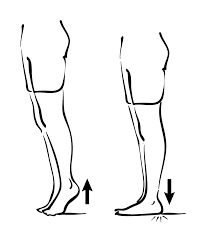
feet shoulder-width apart and facing forwards, the patient slowly moves up onto his toes – raising his heels as far as possible and comfortably without pain. Performed 3 sets of 10 repetitions on each occasion.
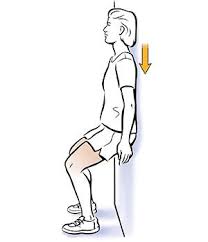
WALL SQUAT
Stand with your back, shoulders, and head against a wall and look straight ahead. Keep your shoulders relaxed and your feet about 3 feet (90 centimeters) away from the wall and a shoulder’s width apart. Keeping your head against the wall, slide down the wall. Lower your buttocks toward the floor until your thighs are almost parallel to the floor. Hold this position for 10 seconds. Make sure to tighten your thigh muscles as you slowly slide back up to the starting position. Do 2 sets of 8 to 12.
DO’S & DON’TS
Get plenty of rest – Your body will need as much energy as it can get to repair the damaged tissues in your knee. Stay off your feet when possible and take it easy for the first few weeks after surgery, when healing is happening the fastest.
Use cryotherapy – Cold therapy is proven to help reduce the pain and swelling that comes after knee surgery. Reducing swelling will help contribute to a faster recovery, so ice your knee regularly. If possible, use an active cold therapy system to get the most from cryotherapy.
Use compression therapy – Compression bandages and modern active compression therapy systems help remove excess fluid from the area surrounding the knee joint to help accelerate healing.
Do physical therapy – Work with a physical therapist to learn the strengthening and stretching exercises that will help you heal faster and prevent future injuries.
Don’t skip doctor visits – Keep the appointment schedule your doctor provides. It is important to stay on track throughout your recovery and only your doctor can confirm that the repairs they performed are healing correctly.
Don’t end physical therapy early – Because the pain subsides and you can get a comfortable range of motion back relatively quickly, many people are tempted to stop going to physical therapy sessions before they have fully recovered. Follow the entire course of care to ensure that the healing process is allowed to complete fully.




One Comment