Achondroplesia

Achondroplasia is a form of short-limbed dwarfism. The word achondroplasia literally means “without cartilage formation.” Cartilage is a tough but flexible tissue that makes up much of the skeleton during early development.
Table of Contents
Causes:
Achondroplasia is caused by a gene alteration (mutation) in the FGFR3 gene. The FGFR3 gene makes a protein called fibroblast growth factor receptor 3 that is involved in converting cartilage to bone. FGFR3 is the only gene known to be associated with achondroplasia.
During early fetal development, much of your skeleton is made up of cartilage. Normally, most cartilage eventually converts to bone. However, if you have achondroplasia, a lot of the cartilage doesn’t convert to bone. This is caused by mutations in the FGFR3 gene. The FGFR3 gene instructs your body to make a protein necessary for bone growth and maintenance. Mutations in the FGFR3 gene cause the protein to be overactive. This interferes with normal skeletal development.
Symptoms-

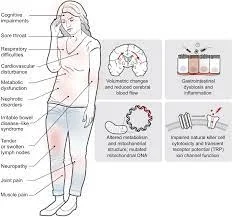
Due to poor bone development, the bones are shortened, particularly in the thigh and upper arms, a condition known as rhizomelia. The thigh and upper arms are more affected because they have longer bones and larger growth plates (regions of the bones where growth occurs).
The lower legs and forearms are affected to a lesser degree because their growth plates are smaller. The hands and feet are also short with unusual separation between the third and fourth digits. Affected individuals reach a maximum height of 120 cm (four feet). The torso usually develops to its proper size but the head may be larger than normal with a prominent forehead and flat nose.
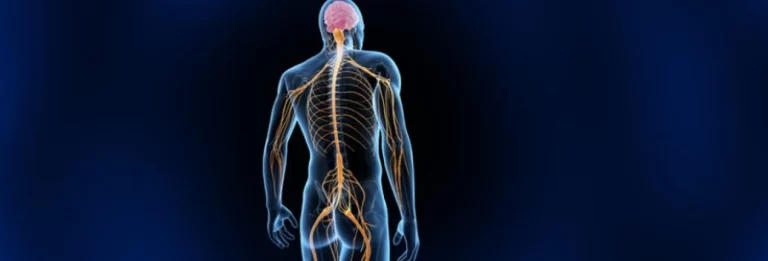
Affected children have delayed development and often take longer to learn to sit, crawl and walk than their unaffected peers. They may also develop a curved spine and bowed legs. Adults can suffer from back and leg pain. Abnormal development of the head may result in hearing loss and infections. In the worst cases, the abnormal structure of the skull and vertebrae can cause compression of the spinal cord, resulting in paralysis and breathing difficulties.
Diagnosis:
Achondroplasia is generally diagnosed by bone measurement during physical examination or after X-ray. Prenatal diagnosis is recommended if one or both of the parents are already affected. In the majority of cases, achondroplasia occurs spontaneously through mutations in the sperm or egg

There are diagnostic tests which may be performed both before and after birth of the individual suspected to suffer from achondroplasia. A prenatal ultrasound of an infant may show signs of excessive amniotic fluid in the womb in cases of achondroplasia. After the infant is born, the front-to-back head size of the newborn is increased when compared to non-affected newborns. The child may also show signs of hydrocephalus. X-rays of the infant may also be used to diagnose achondroplasia as the long bones show changes from those x-rays of non-affected infants.
Medical management:
There are no direct medical treatments for achondroplasia. However, there are many medical treatments for other disorders that may develop as a direct or indirect result of achondroplasia. Because otitis media is a commonly associated condition, medical management will likely be taken to treat it. Screening for hearing loss should also be routinely performed for the same reason. Upper respiratory illnesses are also typical among individuals with achondroplasia and thus medications and other treatments may be given for the management of these issues. The same abnormal development of the skull that predisposes the individual to upper respiratory issues may also lead to dental issues. Therefore, persons with achondroplasia may require the care of an orthodontist to correct malocclusions and crowding.[
Individuals should be routinely screened for other commonly associated conditions so that the appropriate treatment may be provided. Such conditions include but are not limited to spinal stenosis, degenerative joint disease, neurological changes at the spinal root level, and osteoarthritis. Many of these conditions may need to be treated with surgical interventions if left untreated with conservative methods for long periods of time or if conservative treatment does not improve the patient’s symptoms.
Treatment-
There is no cure for achondroplasia. Growth hormones? can help people with achondroplasia to achieve moderate growth in some children.
Surgery is a treatment option in some cases to increase leg length by up to 30 cm, prevent spinal compression, or correct bowed legs.In some people with achondroplasia it may be necessary to drain fluid from the head to:
relieve pressure on the braintest for hydrocephalus, a condition where spinal fluid? builds up inside the skull.
Although there have been no studies which support its use long term, growth hormone has been used in some individuals to promote growth and therefore increase the person’s height. The theory behind this hormone therapy is that growth hormone “stimulates growth of linear bone, skeletal muscle, and organs
Achondroplasia Physiotherapy:
As with the medical management of achondroplasia, there is no physical therapy management directly for the condition. However, due to the extensive list of possible co-morbidities, physical therapy will most likely be indicated for an individual with achondroplasia at some point within their lifespan. Perhaps the most likely indication for physical therapy is for the management of symptoms developed from spinal stenosis from either the cervical or lumbar spine. Because the incidence of this complication is quite large within the population of people with achondroplasia, screening of neurological signs and symptoms should be included in all examinations for this group.

The dysplastic nature of this population’s skeletal system makes them predisposed to a number of degenerative disorders for which physical therapy management can be of use. Individuals with achondroplasia may be referred to physical therapy with osteoarthritis and degenerative joint disease. As a result of these progressive conditions, individuals may have undergone a surgical procedure such as spinal fusion or joint replacement. Physical therapy may be involved before surgery as a conservative treatment to help reduce pain, strengthen the patient’s musculature, and maybe eliminate the need for surgery all together. Post-operatively physical therapy can be used to rehabilitate patients back to their pre-morbid status.
Another important role that physical therapy can play in the role of the lives of persons with achondroplasia is in prevention. Physical therapy can help to prevent the “wear and tear” on individuals with achondroplasia by teaching them compensatory motions, energy-saving methods, and more efficient ways of performing their daily tasks. Physical therapy can also help these individuals and their families to make modifications around the home to make their daily tasks easier and perhaps decrease their risk of some of the degenerative changes so commonly found in this population.