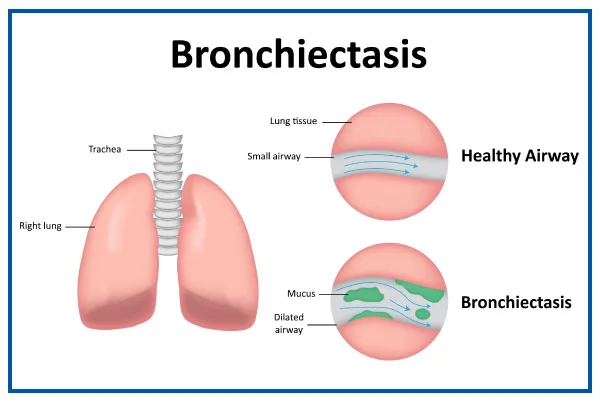
Bronchiectasis
- Bronchiectasis is a condition where damage causes the tubes in your lungs (airways) to widen or grow pouches. It creates it hard to clear mucus out of your lungs & can cause frequent infections. Coughing a lot with pus and mucus is an important symptom of bronchiectasis. Bronchiectasis can not be cured but can be managed with treatment.
- Bronchiectasis is a condition where the bronchial tubes of your lungs are permanently injured, widened, and thickened. These injured air passages allow bacteria and mucus to build up and pool in your lungs. This results in some infections and blockages of the airways.
- There is no cure for bronchiectasis, but it is manageable. With treatment, you can commonly live a typical life.
- However, flare-ups must be treated fastly to maintain oxygen flow to the rest of your body and cure further lung damage.
Table of Contents
What is bronchiectasis?
- Bronchiectasis (“bronk-ee-EK-tuh-sis”) is a lung condition where your airways (tubes going into your lungs) get injured and widen. Damaged airways can not clear mucus like they are supposed to. Bacteria then grow in the mucus, causing more inflammation & damage to your lungs. This makes you cough a lot as your body tries to discard the infected mucus.
What is the difference between bronchiectasis and bronchitis?
- Bronchiectasis and bronchitis have similar symptoms, involving mucus in your lungs and coughing. But bronchiectasis causes permanent widening of your airways & bronchitis is a temporary infection that does not cause lasting damage.
What are the types of bronchiectasis?
- Healthcare providers categorize bronchiectasis based on what the damage to your airways seems like — cylindrical (or tubular), varicose or cystic.
- Cylindrical bronchiectasis is the most usual and least serious form of bronchiectasis.
- Cystic bronchiectasis is the most serious form.
- Providers also classified bronchiectasis as focal (in one area) or diffuse (in many areas throughout your lungs). Traction bronchiectasis occurs when scarring in your lungs pulls your airways out of shape.
Whom does bronchiectasis affect?
- You are at higher risk of bronchiectasis if you are living with an underlying condition that affects your lungs or immune system. Without an underlying condition, your risk improves as you get older.
How common is bronchiectasis?
- About 350,000 to 500,000 people in the U.S. (America) have bronchiectasis. This involves one person out of 150 people who is 75 and older. The usual number might be higher since you can have bronchiectasis without having any symptoms.
How does bronchiectasis affect my body?
- The tubes (airways or bronchi) going into your lungs have defenses to cure you of disease. Annoying as it can often be, mucus is one of these defenses. When mucus can not be coughed out, it causes lasting damage to your airways.
How mucus protects your body
- When you breathe air in, any injurious particles get trapped in mucus in your airways. Then, millions of small, hairlike structures (cilia) use a coordinated motion to move the mucus out of your lungs, such as waves bringing debris to the shore. This is known as mucociliary clearance. You cough out the mucus or swallow it, where the trapped particles are demolished by your stomach acid.
- When any part of this system is not working — if your cilia are damaged or your airways have pockets that trap mucus — you build up mucus in your lungs. The mucus has bacteria caught in it, which can multiply and cause infections. The damage the infections cause can create bronchiectasis worse.
Epidemiology
- Bronchiectasis predominance is not clearly understood. The incidence of bronchiectasis has risen over the past some years. It can exist in any age group, but it commonly occurred in childhood during the pre-antibiotic period. New evidence looks that bronchiectasis disproportionately affects women and older individuals.
Clinically Relevant Anatomy
- Bronchiectasis includes inflammation of the airway walls, specifically the bronchial walls. The main area that is harmed in bronchiectasis is the bronchi.
- The cilia are also harmed in bronchiectasis and the mucociliary clearance of mucus is adversely affected. Cilia line the airway and are connected to the epithelium. They are hair-like with tiny hooks on the tip to grab the mucous and assist move the mucus up to the throat.
Pathophysiology
- The three most significant mechanisms that contribute to the pathogenesis of bronchiectasis are accordance infections, airway obstruction, and peribronchial fibrosis.
- The process starts with inflammatory damage to the bronchial walls, which then stimulates the formation of excess thick mucus.
- The warm and moist environment of the lungs combines with the mucus to cause further inflammation and obstruction, making an excellent environment for infection.
- The thick mucus crushes the cilia and causes further harm. When toxic inflammatory chemicals reacts with the immunity system (i.e. neutrophils), as well as conduct to fibrosis and bronchospasm if persistent.
Medical History
- History of the childhood infection or childhood respiratory symptoms,
- Family history of bronchiectasis, especially cystic fibrosis (CF),
- Smoking history,
- Presence of symptoms to purpose a systemic inflammatory disorder (joint problems, skin rash, muscle pain),
- Duration and seriousness of symptoms,
- Frequency of infective exacerbations.
Objective Examination
- Peripheral examination for signs of chronic lung disease e.g nail changes (clubbing) happens in some forms of bronchiectasis.
- Cough quality, strength, and sputum or mucus production.
- Auscultation: Bronchiectasis is characterized by focal or generalized noises (crepitations, crackles, wheezes,) hear with the stethoscope.
- Dyspnoea on exertion looks to be a major clinical manifestation as it is experienced by three out of four patients.
- Stress incontinence can also be a result of excess (increased) coughing.
- Exacerbations can happen several times a year and are identified by four or more of the following signs and/or symptoms: change in sputum, increased dyspnoea, increased cough, fever of greater than 38°, increased wheeze, decreased exercise tolerance, fatigue, lethargy, and radiographic signs of a new infection.
Is bronchiectasis a serious lung condition?
- Bronchiectasis can be mild or serious depending on how much damage you have in your lungs. Few patient have it and even don’t know about it. Others have had it for a long time and repeated infections have seriously damaged their lungs. Most people with bronchiectasis live a normal life span by managing their symptoms with a provider’s (doctor’s) advice & medication.
What are the symptoms of bronchiectasis?
Symptoms of bronchiectasis involve:
- Cough with lots of mucus & pus
- Repeated colds
- Bad-smelling mucus
- Shortness of breathing (dyspnea)
- Wheezing
- Coughing up blood (hemoptysis),
- Swollen fingertips with curved nails (nail clubbing).
- You might have stretches of time where your symptoms are not as bad and then have a flare-up (exacerbation) where your symptoms get worse.
Exacerbation symptoms involve:
- Extreme tiredness (fatigue)
- Fever, chills
- Increased shortness of breathing
- Night sweats.
What causes bronchiectasis?
- Bronchiectasis is caused by 2 phases of airway damage. In the 1st phase, the initial damage (or “insult”) is caused by an infection, inflammatory disorder, or another condition that affects your lungs. Healthcare providers do not know the initial cause in up to 40% of people with bronchiectasis.
- The 1st insult makes you more likely to get inflammation and repeated infections that cause further damage to your lungs. This is the second phase of the “vicious cycle.”
- Cystic fibrosis (CF) bronchiectasis: This type is related to having CF (Cystic fibrosis) and is a genetic condition that causes atypical production of mucus. CF (Cystic fibrosis) affects your lungs and other organs, like your pancreas and liver. These outcomes in repeated infections in your lungs and may cause bronchiectasis.
- Non-CF (non-cystic fibrosis) bronchiectasis. This type is not related to CF (Cystic fibrosis). The most common known conditions that can lead trusted Source to non-CF (non-cystic fibrosis) bronchiectasis include:
- previous severe respiratory infections, like pneumonia or tuberculosis,
- allergic bronchopulmonary aspergillosis (ABPA),
- primary ciliary dyskinesia,
- primary or secondary immunodeficiency,
- chronic obstructive pulmonary disease (COPD),
- severe asthma.
- The cause of bronchiectasis is not always known or unknown. Certain conditions are known to cause bronchiectasis that harm or damage airways are:
- Conditions that harm the airways, raise the risk of lung infections. For example Allergic bronchopulmonary aspergillosis; pneumonia; measles; inherited disorders eg Primary Ciliary Dyskinesia, Cystic Fibrosis (CF),
- Immunodeficiency: make liable the person for lung infections,
- Pulmonary Diseases ex. asthma, Chronic Obstructive Pulmonary Disease (COPD)
- Lung infections: may cause damage to the walls of the airways, ex. tuberculosis (TB), whooping cough, measles, pneumonia, or fungal infections, especially in childhood
- Conditions that cause an airway blockage, like a growth or a noncancerous tumor, regurgitated stomach acid, or inhaled objects that become stuck and block an airway.
What diseases cause bronchiectasis?
Some of the specific causes of the initial damage (“insult”) which begins the cycle of bronchiectasis include:
- Cystic fibrosis
- Mycobacterial infections, such as MAC infections or tuberculosis (TB)
- Autoimmune or inflammatory disorders, such as rheumatoid arthritis (RA), inflammatory bowel disease (IBD), lupus (SLE), and Sjögren’s syndrome,
- Foreign bodies, tumors, or lymph nodes that block airways and cure mucus clearance,
- Conditions that decrease immunity and increase the risk of infections (like HIV and hypogammaglobulinemia),
- Primary ciliary dyskinesia,
- Organ transplant. Transplant medications decrease immunity and can increase the risk of infection and bronchiectasis.
- Allergic bronchopulmonary aspergillosis (ABPA), an allergy to a type of fungus,
- Fibrosis (scarring) from radiation,
- Alpha-1 antitrypsin deficiency.
Does COVID-19 cause bronchiectasis?
- Research suggests that COVID-19 is not a very common cause of bronchiectasis. But if you have had acute respiratory distress syndrome (ARDS) with COVID-19, you may have pseudobronchiectasis. Pseudobronchiectasis seems like bronchiectasis, but it resolves over time rather than causing the cycle of repeated infections and lung damage.
What is the most common cause of bronchiectasis?
- The most usual cause of bronchiectasis depends on where you live. In the U.S. (America) and other western countries, the most common cause of bronchiectasis is cystic fibrosis. Worldwide, it is tuberculosis. In many cases, healthcare providers can not determine the cause of bronchiectasis.
What are the risk factors for developing bronchiectasis?
- The risk of developing bronchiectasis improves with age, though younger people can have it. Women are more likely to have risks than men.
Other health & medical conditions that can put you at risk of having bronchiectasis involve:
- an unusually functioning immune system,
- repeated aspiration (breathing in) of things such as food or drink,
- inflammatory bowel disease,
- autoimmune diseases such as HIV,
- COPD,
- allergic aspergillosis, which is a hypersensitivity lung reaction to fungus,
- and lung infections, like whooping cough, pneumonia, or tuberculosis.
How is bronchiectasis diagnosed?
- A chest computed tomography (CT) scan is the most usual test for diagnosing bronchiectasis because a chest X-ray does not provide enough detail.
- This painless test makes precise pictures of your airways and other structures in your chest. A chest CT scan can look at the extent and location of lung damage.
- Later bronchiectasis is confirmed with the chest CT scan, your doctor will try to establish the cause of the bronchiectasis based on your history and physical exam findings.
- It is important to find out the exact cause so the clinician can treat the underlying disorder to prevent the bronchiectasis from getting worse. There are many causes that can induce or contribute to bronchiectasis.
- The evaluation for the underlying cause importantly consists of laboratory and microbiologic testing and pulmonary function testing. Your initial evaluation will likely involve a complete blood count with differential (various),
- immunoglobulin levels (IgG, IgM, and IgA),
- sputum culture collection to check for bacteria, mycobacteria, and fungi,
- If your doctor suspects CF, they will order a sweat chloride test or genetic test.
- A healthcare provider (doctor) will diagnose bronchiectasis by examining you and asking you about your health history. They will listen to your lungs and test how well they are working. If they think you have bronchiectasis or another lung condition, they will order imaging tests to look at the structure of your lungs.
What tests will be done to diagnose bronchiectasis?
A healthcare provider may perform a number of tests to diagnose bronchiectasis or rule out other conditions, involving:
- Chest CT scan or X-ray: A provider (doctor) uses a machine to take pictures of your lungs to look if your airways are damaged.
- Blood tests and sputum cultures: A provider (doctor) takes samples of your blood or mucus (sputum) to find out if you have an infection.
- Lung function tests: A provider (doctor) uses lung function tests to determine how well your lungs are working. You will breathe into a machine that measures your lung function.
- Genetic testing: A provider (doctor) may take samples of your blood or other body fluid to test for diseases.
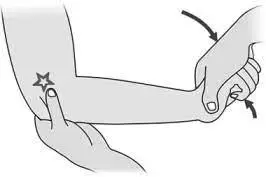
- Sweat chloride test: If a provider (doctor) thinks you could have cystic fibrosis, they’ll perform a sweat test. They will make your arm or leg sweat, collect a sample and test it for signs of cystic fibrosis.
- Bronchoscopy: In some cases, a provider (doctor) may use a procedure to look more closely at your airways (bronchoscopy). They will use a bronchoscope (a long flexible tube with a light and camera at the end) to find and remove anything blocking your airways & acquire samples of mucus or pus from your lungs for testing.
How is bronchiectasis treated?
- Bronchiectasis can not be fully cured, but you can treat the symptoms. Healthcare providers (doctors) treat bronchiectasis by clearing mucus and managing infections. Depending on the severity of your condition, your provider (doctor) might prescribe medication or physical therapy. You may also use medical devices that assist get rid of mucus.
- If bronchiectasis is caused by an underlying condition, treating that condition may assist your symptoms. If you have a tiny area of bronchiectasis, your provider might recommend surgery, though this is rare.
What treatments are used for bronchiectasis?
- Bronchiectasis treatments assist get rid of infected mucus, killing bacteria and decreasing inflammation.
They involve:
- Antibiotics: Antibiotics can treat contagious caused by bacteria. You can take antibiotics in pill form, yet if you have a severe infection, a provider (doctor) will use an IV to give you antibiotics directly into your bloodstream. Providers (doctors) also often prescribe inhaled antibiotics for bronchiectasis. You may use a nebulizer for inhaled medications, which creates the medicine into a mist that you breathe in.
- Macrolides: Macrolides are drugs that treat contagious and inflammation at the same time.
- Expectorants and mucolytics: These are medications that thin mucus and assist you to cough it out. These are available over the counter or by prescription.
- Physical therapy: Postural draining and chest percussion therapy can assist loosen and remove mucus. Breathing exercises can assist open up your airways.
- Medical devices: Oscillating positive expiratory pressure (PEP) devices and percussive vests break up and pull phlegm out from your lungs.
Physiotherapy treatment
- Physiotherapy has a very important role in aiding with symptoms of bronchiectasis. Since mucociliary clearance is decreased to about 15% of normal, patients tend to cough more. Physiotherapy treatments are aimed at aiding secretion clearance, and managing fatigue induced by the effort of ineffective clearance and increased coughing.
- See Chest Physiotherapy for a comprehensive see of the most effective techniques.
The most usual treatments are:
- Active Cycle of Breathing Technique (ACBT)
- Forced expiration technique, often referred to as a huff. It is part of the Active Cycle of Breathing Technique (ACBT) but can be used alone. A huff is very effective at clearing secretions, especially when combined with another airway clearance technique.
- Manual Therapy is a popular treatment technique and is sometimes used when the patient is fatigued or experiencing an exacerbation of symptoms. It describes techniques that include external forces to the chest wall to loosen mucus and involves any combination of percussion, shaking, rib springing, vibrations, and over-pressure. Because of the nature of the technique, it is contraindicated in patients that are holding anticoagulants or that have osteoporosis.
- Postural Drainage (PD) is an effective treatment that incorporates gravity-assisted techniques to help clear secretions from specific segments of the lungs, and sometimes requires tilting the head down to clear secretions from the middle and lower lobes.
- Autogenic Drainage is a technique that utilizes breathing control (BC) to clear secretions from the airways. The aim is to differ the depth, rate, and location of lung volumes during respiration to move secretions from the tiner airways to the larger airways for easier expectoration.
- Positive Expiratory Pressure (PEP) is a technique that describes breathing against resistance and can be executed either through a device or against pursed lips.
- High-Frequency Chest Wall Oscillation is achieved by wearing a vest that reproduces chest physiotherapy. The vest applies positive pressure air pulses to the chest which causes vibrations that loosen and narrow mucus, along with an intermittent cough or huff helps with the clearance of secretions. Allows people to carry out therapy in their own time.
- Intrapulmonary Percussive Ventilation: Intrapulmonary percussive ventilator (IPV) is a machine that brings short bursts of air through a mouthpiece that vibrates the airway walls. It is indicated for short-term use when another technique is contraindicated or has proved ineffective.
- Intermittent Positive Pressure Breathing (IPPB). A technique used to provide short-term or intermittent mechanical ventilation via mouthpiece or mask for the motive of augmenting lung expansion and delivering aerosol medication. Intermittent Positive Pressure Breathing (IPPB) may be applied to intubated as well as non-intubated patients
- Physical Exercise is recommended for respiratory conditions, involving bronchiectasis with the aim of improving aerobic capacity, fitness, and endurance. A study by Lee et al concluded that exercise resulted in short-term improvements and had an impact on dyspnoea and fatigue, and resulted in not many exacerbations over a 12-month period.
Outcome Measures
The following could be used, for many life:
- Dyspnoea Management Questionnaire,
- Incentive Spirometry,
- Borg Rating Of Perceived Exertion,
- Leicester Cough Questionnaire,
- 2-Minute Walk Test.
What foods should you avoid if you have bronchiectasis?
- What you eat does not seem to directly impact bronchiectasis. For instance, you may have heard that avoiding things like milk can assist lower the amount of mucus in your lungs, but research has not shown this to be true.
- What is most important is to maintain good nutrition. You might find yourself losing an unhealthy amount of weight or have another concern about your diet. Tell a dietician if you have concerns about healthy eating with bronchiectasis.
How can I reduce my risk of bronchiectasis?
You can decrease your risk of developing bronchiectasis by managing your lung health:
- Make sure you & your family are up-to-date on recommended vaccinations. Pertussis, the flu, pneumococcal disease, measles & staph infections can all cause or worsen bronchiectasis.
- Work with your healthcare provider (doctor) to treat any ongoing health conditions, especially ones that affect your lungs. Retain your appointments and stick to your treatment plan. Talk to your provider (doctor) if you feel like medications or therapies are not working.
- Avoid breathing in things that can injure your lungs, like cigarette smoke, vaping, fumes, and gases.
What can I expect if I have bronchiectasis?
- Bronchiectasis can not be cured — the harm it causes is irreversible. Yet most people can manage the symptoms of bronchiectasis with strategies recommended by their healthcare provider (doctor).
- Your outlook will depend on how serious your condition is, how well you respond to treatment and what other medical & health conditions you have. You may require to practice physical therapies or take medications daily. More serious cases may impact your quality of life.
Can bronchiectasis be prevented?
- The exact cause of bronchiectasis is unknown in about 50 percent of trusted Sources of cases of non-CF bronchiectasis.
- For others, it is related to atypical genetic characteristics and other medical conditions that affect the lungs. Ways to prevent bronchiectasis involve:
- not smoking tobacco products like cigarettes or quitting smoking,
- avoiding polluted air,
- taking your vaccination against the flu, whooping cough, pneumonia, measles, and COVID-19,
- taking antibiotics to cure and treat infections if you have conditions that put you at risk (studies are currently being done on new formulations of inhaled antibiotics),
- When the cause is unknown, the cure may be challenging. Early recognition of bronchiectasis is important so that you can get treatment before significant lung damage happens.
Complications of bronchiectasis
Damage caused by severe bronchiectasis can conduct to life-threatening complications, involving:
- Respiratory failure: If your lungs are not working properly, you might not be able to get enough oxygen to your blood and tissues, causing respiratory failure.
- Severe bleeding: Blood vessels in your airways may get so harmed that they bleed heavily. You may cough up blood if this occurs.
- Antibiotic resistance: You may use antibiotics so much that you begin getting infections that can no longer be treated with medication.
What is the life expectancy for bronchiectasis?
- With actual treatment, most people with bronchiectasis can expect to live as long as someone without it. A history of smoking & low lung function can decrease your life expectancy.
How do I look after myself with bronchiectasis?
- Managing ongoing conditions and your overall health can assist you to take care of yourself with bronchiectasis.
- Do not smoke: Smoking injures your lungs and can put you at higher risk of dying from bronchiectasis. Ask your healthcare provider if you need to assist in quitting.
- Follow the daily maintenance therapy that your provider (doctor) recommends. Treat exacerbations fastly.
- Eating a healthy diet.
- Drink plenty of water to remain hydrated. These assists keep mucus loose so you can clear it from your lungs.
- Follow a regular exercise routine to retain your lungs healthy.
- Get a flu shot every year and the pneumonia vaccine as recommended by your doctor (provider).
- Practice good hand-washing habits and take another step to avoid getting infectious diseases.
When should I see my healthcare provider (doctor) about bronchiectasis?
- Talk to your healthcare provider (doctor) if you have been coughing with a lot of mucus for several weeks or if you feel short of breath.
If you have been diagnosed with bronchiectasis, you should contact your healthcare provider (doctor) if you:
- Have signs of infection, such as a fever or chills,
- Have more trouble breathing than common,
- Are much more tired than common,
- Are losing weight unintentionally,
- Are coughing up more mucus, phlegm with blood in it, or phlegm that is yellow or green,
- You do not have an appetite.
When should I go to ER?
Go to the ER if you are:
- Coughing up a lot of blood.
- Having chest pains.
- Are struggling to breathe?
- What questions should I ask my healthcare provider?
- Do you know what caused my bronchiectasis?
- How can I prevent further damage?
- How can I manage exacerbations?
- When should I follow up with you?
- What symptoms should cause me to go to the ER?
What is the outlook for people with bronchiectasis?
- The outlook for people with bronchiectasis depends on the seriousness of the condition and what is causing it.
- Bronchiectasis harms 350,000 to 500,000 people in the U.S. While serious bronchiectasis can be fatal, individuals with the non-CF type generally have a good outlook with treatment.
- Early diagnosis is main so that treatment can begin and additional lung damage can be prevented.
Note
- In most cases, bronchiectasis should not keep you from living a full life. Talk to your provider (doctor) about bothering certain symptoms and how to deal with exacerbations. They may not be able to take care of every symptom, yet sometimes small changes can greatly improve your quality of life.
Tips for living with bronchiectasis
- Follow your bronchiectasis treatment plan.
- Take your medications as prescribed.
- Eat a healthy, well-balanced diet.
- Drink lots of water and other nonalcoholic beverages.
- Follow a gentle exercise routine.
- Practice good sleep hygiene.
- Get your annual flu shot.
- Get your COVID-19 vaccination and booster.
- Wash your hands.
- Perform breathing exercises and techniques.
- Maintain good posture.
- Save your energy.
- Relax and incorporate rest periods throughout your day.
- Do your more difficult tasks when your energy levels are highest.
- Ask for help when you need it.
FAQs
Bronchiectasis is caused by the airways of the lungs becoming damaged and widened. This can be the result of an infection or another condition, but sometimes the cause is not known.
What are the types of bronchiectasis? Healthcare providers categorize bronchiectasis based on what the damage to your airways looks like — cylindrical (or tubular), varicose or cystic. Cylindrical bronchiectasis is the most common and least serious form of bronchiectasis. Cystic bronchiectasis is the most severe form.
Most people diagnosed with bronchiectasis have a normal life expectancy with treatment tailored to their needs.
The most common symptom of bronchiectasis is a persistent cough that brings up a large amount of phlegm on a daily basis.
shortness of breath.
wheezing.
coughing up blood or bloodstained phlegm.
chest pain.
joint pain.
Where possible, avoid being in environments with secondhand smoke, pollution, chemical fumes, dust particles, and other substances which may be harmful to the lungs.



2 Comments