Stiff person syndrome (SPS)
- Stiff person syndrome (SPS) is a rare chronic condition that causes muscle stiffness and painful muscle spasms. The seriousness of symptoms differs from person to person. There is no cure for stiff person syndrome (SPS), but treatment can help manage symptoms and slow the progression of the syndrome.
Table of Contents
What is stiff person syndrome?
- Stiff person syndrome (SPS) is an infrequent autoimmune neurological disorder.
- People with this condition commonly experience muscle stiffness in their trunk and abdomen (the middle part of their body). Over time, they develop stiffness (rigidity) and spasms in their legs and other muscles. Walking may become harmful, and people become more prone to falls and injury.
- Stiff person syndrome is utilized to be called “stiff man syndrome,” yet the name was updated to be more inclusive, as the disorder can affect people of any age and sex.
- An autoimmune disorder happens when your immune system incorrectly identifies healthy body tissues as harmful and attacks them.
- Stiff person syndrome (SPS) causes you to experience uncontrolled episodes of muscle spasms and stiffness. It is a progressive disorder that can ultimately impede walking and other basic daily functioning skill.
- Stiff person syndrome (SPS) can significantly interfere with your quality of life without proper treatment. However, it is a rare disorder affecting only about 1 to 2 people per million trusted Sources. It has been described as starting between the ages of 30 and 60 and appears to be more usual in females.
Types of stiff person syndrome (SPS)
There are several different subtypes or classifications for Stiff person syndrome (SPS), including:
- Classic Stiff person syndrome (SPS): This is the most common form. It is associated with GAD (glutamic acid decarboxylase) antibodies, though studies have reported another antibody association.
- Stiff person syndrome (SPS) variants: There are several variants of Stiff person syndrome (SPS) that can involve specific parts of your body or involve more prominent incoordination (ataxia).
- Progressive encephalomyelitis with rigidity and myoclonus (PERM): PERM is a more severe variant of Stiff person syndrome (SPS) causing decreased consciousness, eye movement issues, ataxia, and autonomic dysfunction. Progressive encephalomyelitis with rigidity and myoclonus (PERM) commonly requires management in a hospital due to autonomic dysfunction.
How does stiff person syndrome (SPS) affect?
- Women and people assigned female at birth (AFAB) are twice as likely to have Stiff person syndrome (SPS) as men and people assigned male at birth (AMAB).
- Stiff person syndrome (SPS) can develop at any age, but symptoms most often begin in your 30s and 40s.
Stiff person syndrome (SPS) is also associated with the presence of other autoimmune conditions, such as:
- Type 1 diabetes,
- Autoimmune thyroid disease
- Vitiligo
- Pernicious anemia
- Celiac disease.
How common is stiff person syndrome?
- Stiff person syndrome (SPS) is very rare. About one out of every 1 million people have the syndrome.
What are the symptoms of stiff person syndrome (SPS)?
- Stiff person syndrome (SPS) spasms can be very strong and may cause you to fall if standing. They can often be strong enough to break bones. The spasms may be worse when you are anxious or upset. Sudden movements, loud noise, or touching can trigger involuntary spasms.
- When you are living with Stiff person syndrome (SPS), you may also have depression or anxiety. This may be caused by other symptoms you might be experiencing or a reduction in neurotransmitters in the brain.
- The potential for emotional distress can increase as Stiff person syndrome (SPS) progresses. You may notice the spam worsen when you are out in public. This may conduct you to develop anxiety about going out in public.
- You may experience improved muscle stiffness and rigidity in the later stages of Stiff person syndrome (SPS). Muscle stiffness can affect other body parts, such as your face. This can involve muscles used for eating and talking. Muscles included in breathing may also be affected, causing life-threatening breathing problems.
The two important symptoms of stiff person syndrome (SPS) are:
- Muscle stiffness or rigidity.
- Painful muscle spasms.
- Stiff person syndrome (SPS) symptoms can spread to other areas of your body and/or get worse over time. Symptoms can take several months to a certain year to develop. Some people’s symptoms remain similar for years. Others experience slowly worsening symptoms, involving more severe spasticity/rigidity, which can limit their ability to perform activities of daily living.
Muscle stiffness
- In most cases of stiff person syndrome (SPS), your trunk (abdomen, chest, and back) muscles are the first to become stiff. The rigidity causes pain and an aching discomfort. These symptoms can fluctuate in seriousness without a clear reason or trigger. They can affect your arms and legs. As stiffness increases, certain people develop an abnormal posture that can make it difficult to walk or move.
Muscle spasms
- Painful muscle spasms are another symptom of Stiff person syndrome (SPS). They can include your entire body or only a specific area. These spasms can last a certain seconds, minutes, or, occasionally, a few hours.
Spasms can be triggered by:
- Unexpected or loud noises
- Physical touch or stimulation
- Changes in temperature, including cold environments
- Stressful events.
- Due to the unpredictable triggers of muscle spasms, some people with Stiff person syndrome (SPS) develop anxiety and agoraphobia — an extreme fear of entering open or crowded places or of leaving their homes. This is because it is more difficult to avoid the triggers of muscle spasms in public.
What causes stiff person syndrome?
- Researchers do not know the exact cause of stiff person syndrome. But they think it is an autoimmune condition, a condition in which your immune system attacks healthy cells for unknown reasons.
- Many people with Stiff person syndrome (SPS) make antibodies against glutamic acid decarboxylase (GAD). Glutamic acid decarboxylase (GAD) plays a role in making a neurotransmitter known as gamma-aminobutyric acid (GABA), which helps control muscle movement.
- Researchers do not yet understand the exact role that glutamic acid decarboxylase (GAD) plays in the development and worsening of SPS. It is important to note that the presence of glutamic acid decarboxylase (GAD) antibodies does not mean that someone has Stiff person syndrome (SPS). In fact, a small portion of the general population has glutamic acid decarboxylase (GAD) antibodies without any adverse effects.
- There are other antibodies associated with Stiff person syndrome (SPS), including glycine receptor, amphiphysin, and DPPX (dipeptidyl peptidase-like protein 6) antibodies. There are also some people with Stiff person syndrome (SPS) who have no detectable known antibodies. Research is ongoing to see if there are other potential antibodies that have not yet been discovered.
How is stiff person syndrome (SPS) diagnosed?
- Stiff person syndrome (SPS) can be difficult, as since it is rare and its symptoms are similar to other conditions such as ankylosing spondylitis, multiple sclerosis, or other autoimmune conditions. A healthcare provider (doctor) may use several tests to rule out these conditions and look for specific signs of stiff person syndrome (SPS).
- They will ask you questions about your symptoms and perform a physical exam and neurological exam.
- They will consider other causes of movement problems with muscle spasms, like multiple sclerosis (MS) and Parkinson’s disease, which have their own diagnostic criteria. Stiff person syndrome (SPS) might be considered when the signs and symptoms do not fit with more common neurological conditions.
- The doctor may also do electromyography (EMG) to calculate your muscular electrical activity.
- Your doctor may order a blood test to detect the GAD or other antibodies. Not everyone with Stiff person syndrome (SPS) has these antibodies. However, up to 80%Trusted Source of people living with Stiff person syndrome (SPS) do have elevated GAD antibodies.
If your provider suspects stiff person syndrome, tests to confirm the diagnosis may involve:
- Antibody blood test: A blood test can check for the presence of antibodies to glutamic acid decarboxylase (GAD) (or other relevant antibodies) and for other signs that might indicate or rule out other diseases.
- Electromyography (EMG): This test measures electrical activity in your muscles and can assist rule out other causes of your symptoms.
- Lumbar puncture (spinal tap): During a lumbar puncture, a healthcare provider uses a needle to draw fluid from your spinal canal to check for the presence of antibodies to glutamic acid decarboxylase (GAD). They will also look for other signs that might indicate or rule out other conditions.
What is the treatment for stiff person syndrome (SPS)?
- Treatment for stiff person syndrome (SPS) is based on your symptoms. The goal of treatment is to manage symptoms and increase your mobility and comfort.
The two main treatment strategies involve:
- Medications & therapies for symptom management
- Immunotherapy, or disease-modifying treatment.
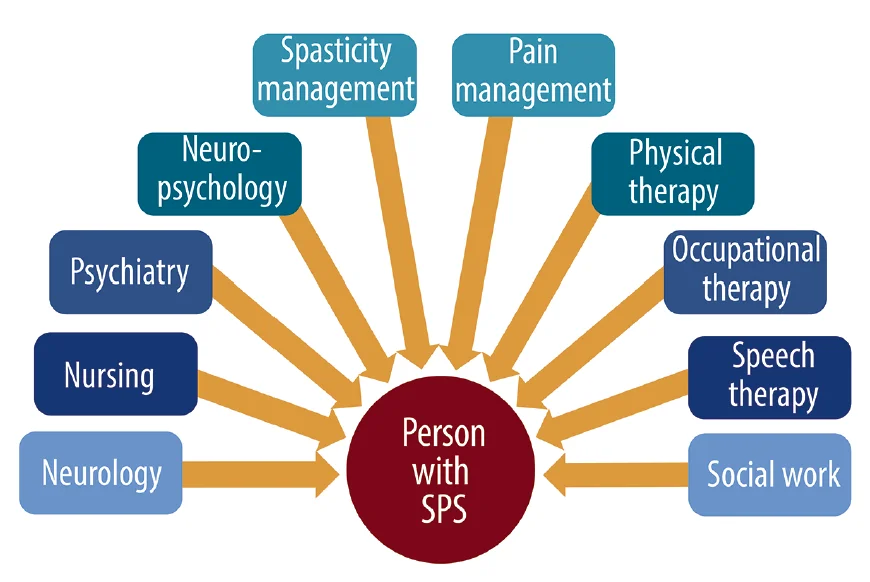
Your healthcare team may involve several specialists, such as:
- Neurologists, specifically, neuroimmunologists
- Occupational and physical therapists
- Physical medicine and rehabilitation specialists
- Speech therapists
- Mental health specialists, such as psychologists.
Medications and therapies for symptoms
Medications that can assist decrease stiffness, rigidity, and painful muscle spasms include:
- Benzodiazepines: Benzodiazepines are a class of drugs that treat a variety of conditions, like anxiety, seizures, and insomnia. They affect GABA signals. Healthcare providers often prescribe diazepam as a first-line treatment for stiff person syndrome (SPS).
- Muscle relaxants: Baclofen can assist treat muscle spasms. It works by relaxing your muscles, which decreases muscle stiffness.
- Neuropathic pain medications: Medications such as gabapentin and pregabalin also affect GABA signals and can help with stiff person syndrome (SPS) symptoms.
Therapies that may also help manage symptoms involve:
- Physical therapy
- Massage
- Hydrotherapy (water therapy)
- Heat therapy
- Acupuncture.
Immunotherapy
- There is some evidence to suggest that intravenous immunoglobulin (IVIg) treatment (a type of immunotherapy) can improve symptoms for some people with stiff person syndrome (SPS).
- Intravenous immunoglobulin (IVIg) contains immunoglobulins (natural antibodies your immune system produces) donated by thousands of people with healthy immune systems.
There is no cure for Stiff person syndrome (SPS). However, treatments are available to assist you to manage your symptoms. Some treatments may also stop the condition from getting worse. Muscle spasms and stiffness may be treated with 1 or more of the following medications:
- muscle relaxers like baclofen,
- benzodiazepines like diazepam(Valium) or clonazepam (Klonopin),
- anti-seizure medications such as gabapentin (Neurontin),
- anticonvulsants like pregabalin (Lyrica).
- You may also require to take medications for pain and discomfort. Antidepressants such as selective serotonin reuptake inhibitors (SSRIs) may also help trusted Sources with depression and anxiety.
- Additional treatments have been shown to help prevent the disease process of Stiff person syndrome (SPS).
These include:
- Autologous stem cell transplant: This is the process where your blood and bone marrow cells are collected and multiplied previous transferring back to your body. This promotes the creation of immune cells that do not causes the Stiff person syndrome (SPS) autoimmune process. This is an experimental treatment, yet it has shown Trusted Source some success.
- Intravenous immunoglobulin: This treatment can reduce the number of antibodies that attack healthy tissues.
- Plasmapheresis: This is a procedure in which your blood plasma is traded with new plasma to decrease the number of antibodies in the body.
- Immune-suppressing drugs: This involves rituximab (Rituxan) and tacrolimus.
In addition to medications, your doctor may refer you to a physical therapist. Physical therapy alone can not treat Stiff person syndrome (SPS).
However, the exercises may significantly assist Trusted Source with your:
- emotional well-being
- walking
- independence
- pain
- posture
- overall day-to-day function
- range of motion.
- Depending on your symptoms, your physical therapist will monitor you through mobility and relaxation exercises. With the assistance of your therapist, you may even be able to practice some movements at home.
Physical Therapy Management
- It is important to note that physical therapy could worsen symptoms of Stiff person syndrome (SPS) during certain phases of the disease; the efficacy of physical therapy is highly variable, and certain precautions should be taken the previous proceeding with treatments.
Scott Newsome, DO, Department of Neurology at Johns Hopkins Medical recommends that physical therapy include:
- Deep tissue myofascial techniques
- Ultrasound,
- Passive range of motion (ROM) (any type of contractile exercise can reproduce or worsen symptoms),
- Heat therapy or possibly hydrotherapy, like any type of cold therapy can exacerbate symptoms.
- Ultimately, physical therapy should be tailored to the individual with Stiff person syndrome (SPS), as patients may present in different ways. It is important to comply with patient goals, understand symptom triggers, and assist in the best way possible in order to reduce pain and increase the quality of life in those living with Stiff person syndrome (SPS).
- Although no formal measurement tools exist for stiff person syndrome (SPS), both the Functional Independence Measure (FIM) and the Timed up and Go (TUG) assessment tools have been used as objective measures in the assessment of Stiff person syndrome (SPS).
Differential Diagnoses
Stiff person syndrome (SPS) is often misdiagnosed as a more common neurological or psychological condition, including but not limited to the following:
- Multiple sclerosis
- Parkinson’s disease
- Fibromyalgia
- Generalized anxiety disorder
- Phobias
- Psychosomatic illness.
Can stiff person syndrome (SPS) be cured?
- There is currently no cure for stiff person syndrome (SPS). Treatment includes managing symptoms.
Can I prevent stiff person syndrome (SPS)?
- As stiff person syndrome (SPS) is an autoimmune-related condition, there is nothing you can do to prevent developing it.
What is the prognosis for stiff person syndrome?
Stiff person syndrome (SPS) is a chronic (lifelong) condition. The prognosis (outlook) differs from person to person based on a few factors, including:
- Symptom severity,
- How quickly the condition progresses,
- How well treatment helps.
- Starting treatment soon later symptoms begin is essential to cure or lessen the syndrome’s progression and avoid long-term complications. Most people with stiff person syndrome (SPS) improve with medications, but it can still be difficult to manage triggers that cause muscle spasms.
- Over time, walking can become more and more harmful. Your ability to perform daily, routine tasks may decline over time. The increased risk of falls also becomes a growing concern as stiff person syndrome (SPS) worsens. Some people may require to use a cane, walker, or wheelchair for assistance.
What questions should I ask my doctor?
If you have stiff person syndrome (SPS), it may help to ask your healthcare provider the following questions:
- What treatment do you suggest based on my symptoms?
- What can I do at home to assist my symptoms?
- What signs of complications should I see out for?
- What can I expect to occur to my health in the future?
- Are there any clinical inquiries for stiff person syndrome?
How do I take care of myself if I have stiff person syndrome (SPS)?
- If possible, try to find a healthcare provider who specializes in researching and treating stiff person syndrome (SPS). Because the syndrome is rare, this may be harmful. You may have to advocate for yourself to ensure you get the best medical care that can assist you to have the best quality of life.
- It is common for people with stiff person syndrome (SPS) to experience anxiety or depression related to the condition. If you are experiencing mental health symptoms, it is important to talk to your provider or a mental health specialist, such as a therapist or psychologist.
- You and your family may want to consider joining a support group to meet others who can relate to your experiences.
When should I see my healthcare provider?
- If you have stiff person syndrome (SPS), you will need to see your healthcare team regularly to check if your treatment is working and to monitor the progression of your symptoms.
- If you notice new symptoms or side effects of your medications, talk to your healthcare provider (doctor).
- If you are living with this condition, you are more prone to falls because of a lack of stability and reflexes. This can improve your risk for severe injuries and even permanent disability.
- Occasionally, stiff person syndrome (SPS) can progress and spread to other areas of your body.
- There is no prevention for stiff person syndrome (SPS). However, treatments are available to assist you to manage your symptoms. Your overall see depends on how well your treatment plan works.
- There are different treatments, and it is not possible to predict with certainty which treatments will be most effective for you.
- Discuss your symptoms with your doctor. It is especially important to discuss any new symptoms you are experiencing or if you are not seeing any improvements. This information can assist them to choose the best treatment plan for you.
NOTE
- Conception your stiff person syndrome (SPS) diagnosis can be overwhelming. Your healthcare (doctor) team will devise a management plan that is unique to you and your symptoms. It is important to make sure you are getting the support you need and to stay attentive to your health. Know that your healthcare (doctor) team will be there to support you and your family.
FAQs
The main symptoms of Stiff Person Syndrome (SPS) are muscle stiffening in the torso and limbs, along with episodes of violent muscle spasms. These can be triggered by environmental stimuli (like loud noises) or emotional stress. The muscle spasms can be so severe that they cause the person to fall down.
Stiff person syndrome (SPS) is a rare chronic condition that causes muscle stiffness and painful muscle spasms. The severity of symptoms varies from person to person. There’s no cure for Stiff Person Syndrome (SPS), but treatment can help manage symptoms and slow the progression of the syndrome.
From symptom onset to death, the course of Stiff Person Syndrome (SPS) can range from 6-28 years. Although the treatment for Stiff Person Syndrome (SPS) is available, it does not cure the syndrome. Many patients have a slow course of the disorder that is mostly without symptoms, punctuated by occasional episodes of stiffness.
The characteristic findings associated with Stiff Person Syndrome (SPS) are progressive, fluctuating muscular rigidity that occurs along with muscle spasms. The severity and progression of Stiff Person Syndrome (SPS) can vary from one person to another. The symptoms usually develop over a period of months and may remain stable for many years or slowly worsen.
A definitive diagnosis can be made with a blood test that measures the level of glutamic acid decarboxylase (GAD) antibodies. Most people with Stiff Person Syndrome (SPS) have elevated (higher) levels of GAD antibodies. Antibody titers are important for the diagnosis of Stiff Person Syndrome (SPS).
Stiff-person syndrome (SPS) is a rare neurological disorder, which is an autoimmune disorder frequently associated with the presence of serum anti-glutamic acid decarboxylase (GAD) antibody (anti-GAD Ab).
The differential diagnosis for Stiff-Person Syndrome (SPS) is diverse including neurological, autoimmune, and infectious disorders like Parkinsonism, axial dystonia, Ankylosing Spondylitis (AS), and tetanus (16).
Stiff person syndrome (SPS) is a rare terminal condition. There are many treatment options available, but none can cure it. The treatment options aim to ease your symptoms while also improving your comfort. Over time, Stiff Person Syndrome (SPS) can limit your ability to move or walk.
Stiff-person syndrome (SPS), formerly called stiff-man syndrome) is an uncommon disorder characterized by progressive muscle stiffness, rigidity, and spasm involving the axial muscles, resulting in severely impaired ambulation?





One Comment