Prolapsed intervertebral disc Disease (PIVD) : Physiotherapy Treatment, Exercise
Table of Contents
Introduction :
Prolapsed intervertebral disc disease is a condition where the soft, central portion of an intervertebral disc herniates out of the disc space to the outer part of the vertebral body. This may lead to compression of the spinal cord or of the nerve roots of the spinal cord. Partial or complete blockage of nerve signals may occur, which may lead to pain, loss of sensation, leg weakness, back pain, and bowel and bladder problems.
- PIVD is a discrete clinical entity wherein the posterior longitudinal ligament gives way and the disc material herniates into the spinal canal.
- Incompetence of the posterior longitudinal ligament can be a result of vertical spinal instability or can be a result of an acute stretch related to sudden exertion or bending.
Relevant anatomy :
- The intervertibral disc consists of three distict components-the cartilage end-plates, nucleus pulposus and annulus fibrosus.
- The cartilage plates are thin layers of hyline carilage between adjacent vertebral bodies and disc proper.
- The disc receives its nutrition from the vertebral bodies via these end-plates,by diffusion.
- The nucleus pulposus is a gelatious material which liea a little posterior to the central axis of the vertebrae.
- It is enclosed in annulus fibrosus, a structure composed of concentric rings of fibro-cartilaginous tissue.
- The nucleus pulposus is normally under considerable pressure,and is restrained by the crucible-like annulus.
- The posterior longitudinal ligament is a strap-like ligament at the back of the vertebral bodies and disc .
Pathology:

- The term prolapsed disc means the protrusion or extrusion of the nucleus pulposus through a rent in the annulus fibrosis.
- It is not a one time phenomenon rather it is a sequence of changes in the disc, which ultimately lead to its prolapse.
a)Nucleus degeneration :
- Degenerative changes occur in the before the displacement of the nuclear material.
- These changes are :
- i) Softning of the nucleus and its fragmentation
- ii) Weakening and disintegration of the posterior part of the annulus.
b) Nucleus displacement :
- The nucleus is under positive pressure at all times.
- When the annulus becomes weak, either because a small area of its entire thickness has disintegrated spontaneously or because of injury, the nucleus tends to bulge through the defect .
- This is called disc protrusion.
- This tendency is greatly increased if the nucleus is degenerated and fragmented.
- Finally,the nucleus comes out of the annulus, and lies under the posterior longitudinal ligament though it has not lost contact with the parent disc.
- This is called disc extrusion .
- Once extruded, the disc does not go back.
- The posterior longitudinal ligament is not strong enough to prevent the nucleus protruding further.
- The extruded disc may loose its contact with the parent disc , when it is called sequestrated disc.
- The sequestrated disc may come to lie behind the posterior longitudinal ligament or may become free fragment in the canal.
c) Stage of fibrosis:
- This is the stage of repair .
- This begins alongside of degeneration .
- The residual pulposus becomes flattened, fibrosed, and finally undergoes calcification .
- At the same time, new bone formation occurs at the points where the posterior longitudinal ligament has been stripped from the vertebral body and spur formation occurs.
- The site of exit of the nucleus is usually postero-lateral on one or the other side.
- occasionally, it can be central disc prolapse.
- The type of nuclear protrusion may be : a protrusion, an extrusion or a sequestration.
- A dissectiong extrusion, may occur.
- The commonest level of disc prolapse is between L4-L5 in the lumber spine and C5-C6 in the cervical spine.
- In the lumber spine, it is uncommon above L3-L4 level.
Secondary changes associated with disc prolapse :
As a consequence of disc prolapse, change occure in the structures occupying the spinal canal, and in the intervertebral joints.
these are as follows:
a) Changes in structures occupying spinal canal :
- Commonly, unilateral protrusion is in contact with the spinal theca and compresses one or more roots in their extra-thecal course.
- Usually, a single root is affected.
- Sometimes, two roots on the same or opposite sides are affected.
- The nerve root affected is usually the one which leaves the spinal canal below the next vertebra.
- This is because the root at the level of prolapsed disc leaves the canal in the upper-half of the foramen .
- Thus, the nerve root affected in a disc prolapse between L4-L5 vertebrae is L5, although it is the L4 root which exits the canal at this level.
- Pressure effects on the intra-thecal roots of the cauda equina may occur by a sudden large disc protrusion in the spinal canal ,and may present as cauda equina syndrome .
- This is uncommon.
b) Changes in the intervertebral joints :
- With the loss of a part of the nucleus pulposus and its subsequent fibosis, the height of the disc posterior facet joints.
- The incongruity of the facet articulation leads to degenerative arthritis.
Clinical features :
- The patient is usually an adult between 20-40 years of age, with a sedentary lifestyle.
- The commonest presenting symptom is low back pain with or without the pain radiating down the back of the leg.
- A preceding history of trauma is present in some cases.
- In a few cases, there is a history of exertion such as having lifted something heavy or pushed something immediately precending a sudden-onset backache .
The following symptoms are common :
- The onset of backache may be acute or chronic.
- An acute backache is severe with the spine held rigid by muscle spasms, and any movement at the spine pain.
- The patient may be able to get about with difficulty, in extreme cases, he has completely incapacitated any attempted movement producing severe pain and spasm.
- In chronic backache, the pain is dull and diffuse, usually made worse by exertion, forward bending, sitting, or standingin one position for a long time.
- It is relieved by rest.
Sciatica Pain :
- This is usually associated with low back pain, but maybe the sole presenting symptom.
- The pain radiates to the gluteal region, the back of the thigh, and the leg.
- The pattern of radiation depends upon the root compressed.
- In S1 root compression, the pain radiates to the postero-lateral calf and heel.
- In L5 root compression, the pain radiates to the anterolateral aspect of the leg and ankle.
- In a disc prolapse at a higher level(L2-L3 etc.), the pain may radiate to the front of the thigh.
- Often the radiation may begin on walking and is relieved on rest (neurological claudication).
Neurological symptoms :
- Sometimes, the patient complains of paraesthesias, most often described as pins and needles corresponding to the dermatome of the affected nerve root.
- The maybe numbness in the leg or foot and weakness of the muscles.
- In cases with large disc material compressing the theca and roots, a cauda equina syndrome results, where the patient has irregular LMN type paralysis in the lower limbs, bilateral absent ankle jerks, with hypoaesthesia in the region of L5 to S4 dermatomes, and urinary and bowel incontinence.
Diagnosis :
The diagnosis is mainly clinical.
Investigations like C.T. Scan and M.R.I. scans may be done to confirm the diagnosis, especially if surgery is being considered.
Physical Examination :
- The back and limbs are examined with the patient undressed.
The following observation is made :
Posture :
- The patient stands with a rigid, flattened lumbar spine.
- The whole trunk is shifted forwards on the hips.
- The trunk is tilted to one side ( sciatic tilt or scoliosis ).
- The sideways tilt tends to exaggerate on attempted bending forwards.
Movements :
- The patient is unable to bend forward, any such attempt initiates severe muscle spasm in the paraspinal muscles.
Tenderness :
- There is diffuse tenderness in the lumbosacral region.
- Localized tenderness in the midline or lateral to the spinous process is found in some cases.
Straight leg raising test (SLRT) :
- This test indicates nerve root compression.
- A positive SLRT at 40 degrees or less is suggestive of root compression.
- More important is a positive contralateral SLRT.
Lasegue test :
- This is a modification of SLRT where first the hip is lifted to 90 degrees with the knee bent.
- The knee is then gradually extended by the examiner.
- If nerve stretch is present , it will experience pain in the back of the thigh or leg.
Neurological examination :
- A careful neurological examination would reveal a motor weakness, sensory loss, or loss of reflex corresponding to the affected nerve root of special importance is the examination of the muscles of the foot supplied by L4, L5, and S1 roots, as these are the roots affected more commonly.
- The extensor hallucis longus muscle is exclusively supplied by L5 root and its weakness is easily detected by asking the patient to dorshiflex the big toe against resistance .
- Sensory loss may be merely the blunting of sensation or hypoaesthesia in the dermatome of the affected root.
- I gives the neurological findings as a result of compression of different roots.
Investigations:
Plain X-ray :
- Plain X-ray does not show any positive signs in a case of acute disc prolapse.
- X-rays are done basically to rule out bony pathology such as infection.
- In cases of chronic disc prolapse, the affected disc space may be narrowed, and there may be lipping of the vertebral margins posteriorly.
Myelography :
- With the availability of non-invasive imaging techniques like the C.T.scan, the usefulness of myelography has become limited.
- It is performed in cases where precise localisation of the neurological signs in not possible.
- It is also used in cases if facilities for a C.T. scan are not available.
The following myelographic features suggest disc prolapse :
- Complete or incomplete block to the flow of dye at the level of dye at the level of a disc.
- An indentation of the dye-column.
- Root cut-off sign: Normally, the dye fill-up the nerve root sheath.
- In cases where a lateral disc prolapse is presenting on the nerve root, the sheath may not be filled.
- It appears on the X-ray as an abrupt blunting of the dye-columm filling the root sheath.
C.T. scan :
- Normally, in an axial cut section, the posterior border of a disc appears concave.
- In a case where there is disc prolapse, it will appear flat or convex.
- There will be loss of pre-thecal fat shadow normally seen between the posterior margin of the disc and theca.
- The herniated disc material can be seen within the spinal canal,pressing on the nerve-roots or theca.
M.R.I Scan :
- This is the investigasion of choice .
- It shows the prolapsed disc,theca ,nerve roots.
- Very clearly.
Electromyography (EMG) :
- Findings of denervation, localized to the distribution of a prticular nerve root, helps in localizing the offending disc in cases with multiple disc prolapses.
- This test is rarely required.
Differential diagnosis :
- A prolapsed disc is a common cause of low backache especially the backache associated with sciatic pain.
- One must be extremely cautious and avoid misdiagnosis of other diseases that may mimic a disc prolapse.
- These include ankylosing spondylitis, vascular insufficiency, extra-dural tumour, spinal tuberculosis.
Treatment of Prolapsed intervertebral disc Disease :
PIVD Treatment mainly are symptomatic pain relieving Medicine like NSAIDs and Physiotherapy treatment and exercise, if this treatment are not improving your condition then surgery is last treatment of choice mostly suggested by Doctor’s.
Principles of treatment :
- The aim of treatment is to relieve of the symptoms, mostly possible by remission of the symptoms, with conservative treatment like pain relieving medicine with rest, traction and Physiotherapy exercise and Electrotherapy modalities.
- Cases that do not respond to conservative treatment for 3-6 weeks and those presenting with cauda equina syndrome may require operative intervention.
Conservative treatment :
Rest :
- It is most important in the treatment of a prolapsed disc .
- Rest on a hard bed is necessary for 2-3 weeks.
Drugs :
- These consist of mainly analgesics and muscle-relaxants.
Operative treatment :
Indications for operative treatment are :
- Failare of conservative treatment
- Cauda equina syndrome
- Severe sciatic tilt.
The disc is removed by the following techniques :
Fenestration :
- The ligamentum flavum bridging the two adjacent laminae is excised and the spinal canal at the level exposed.
Laminotomy :
- In addition to fenestration,a hole is made in the lamina for wider exposure.
Hemilaminectomy :
- The whole of the lamina on one side is removed.
Laminectomy :
- The laminae on both side with the spinous process, are removed.
- Such a wide exposure is required for a big, central disc producing cauda-equina syndrome.
Chemonucleolysis :
- In this technique, an enzyme with the property of dissolving fibrous and cartilaginous tissue is injected into the disc, under X-ray control.
- This leads to the dissolution and fibrosis of the disc and thus relief of symptoms.
- It can through a few puncture wounds.
Percutaneous discectomy :
- This is a more recent technique where the disc is removed by using an endoscope and fine endoscopic instruments or laser probes inserted percutaneously through small stab wounds.
- Through a minimally invasive technique, its indications are limited, and one requires adequate instrumentation and training.
Physiotherapy treatment in PIVD :
Before planning the treatment, determine the position of comfort or symptom reduction i.e FUNCTIONAL POSITION. The patient may have.
a) Extension bias: Patient’s symptoms are lessened in the position of extension (bending back) and provoked in flexion (bending forwards) e.g PIVD.
b) Flexion bias: Patient’s symptoms are lessened in the position of spinal flexion (bending forwards) and provoked in spinal extension (bending backward) e.g spinal stenosis, spondylolisthesis.
Spinal Extension (bending back) is contraindicated if:
i) when no position or movement decreases or centralizes the pain.
ii) when saddle anesthesia and/or urinary incontinence is present (could indicate spinal cord or cauda equina lesion due to large central disc herniation).
iii) when the patient is in such extreme pain that he rigidly holds the body immobile.
Spinal flexion (bending forward) is contraindicated if:
i) when extension relieves the symptoms.
ii) when flexion increases or peripheralizes the symptoms.
Acute Phase of Prolapsed intervertebral disc Treatment :
Aims:
a) To relieve pain.
b) To promote muscle relaxation.
c) To relieve inflammation and pressure against the pain-sensitive or neurologic structures.
d) patient education.
e) prevention.
Physiotherapy Treatment in Acute Phase of PIVD:
a) CONTROLLED REST– is recommended i.e rest in the form of-
Posture and activity modification- Avoid flexed postures, sitting for a long duration, bending or lifting activities, asymmetric postures ( flexion and rotation).
All these activity increase the disc pressure.
Local support in the form of a corset (lumbosacral belt), abdominal binder, use of taping technique, etc.
These measures will enhance healing and prevent re-injury to the healing disc.
Within 10 days fibrin is laid down.
If the spine is maintained in lordosis, the annulus will heal in shortened position and the nucleus will be retained centrally.
If symptoms are severe, bed rest (maximum for 2 days) on a hard bed is indicated with short periods of walking at regular intervals ( with corset).
Walking promotes lumbar extension and stimulates fluid mechanics to help reduce swelling in the disc/connective tissues.
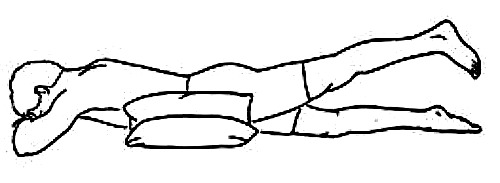
If a patient presents with an inability to straighten up, make the patient lie prone with 2-3 pillows under the abdomen.
As the pain subsides, remove the pillows and prop up the trunk by placing pillows under the thorax.
By this nucleus pulposus is shifted forwards and relieves pain and gains a lordosis.
b) MODALITIES TO REDUCE PAIN AND SPASM-
Hot Pack / Cold Pack : reduces muscle spasms and inflammation in the acute phase.
TENS: relieves pain in both acute and chronic phases.
Ultrasound Therapy (US) : as phonophoresis increases the extensibility of connective tissues
Moist heat: used as an adjunct before applying specialized techniques to decrease muscle spasms.
Short Wave Diathermy (SWD)– pulsed SWD in acute conditions and continuous SWD in chronic cases.
Interferential Therapy (IFT) is used to reduce radiating pain, muscle spasm.
Soft tissue manipulation– to reduce local muscle spasms and induce relaxation.
Lumbar /Cervical Traction- may be beneficial to relieve nerve root compression and radiculopathy or paraesthesias in the acute phase of PIVD. Reduces nuclear protrusion by decreasing the pressure on the disc or by placing tension on the posterior longitudinal ligament. Time of traction should be short in the acute phase else there could be an increase in disc pressure leading to increased pain due to fluid imbibition ( less than 15 minutes of intermittent traction and less than 10 minutes of sustained traction).
Manual mobilization for PIVD: Manual mobilization is very effective in the treatment of PIVD ( prolapsed intervertebral disc), with the help of some hand manual technique we can adjust the lumbar disc alignment, which helps in decreasing radiate pain and other symptoms.
(D) EXERCISES FOR HERNIATED DISC:
Herniated disc exercises play a vital role in the treatment of pain and inflammation.
Extension exercises are useful in the early treatment of disc-related signs and symptoms.
Techniques to mechanically reduce a nuclear disc protrusion- These are used if the test movements show that these movements and postures improve the symptoms:
(a) Posterior or posterolateral protrusion:
(i) Passive Back Extension exercise :
The patient is lying prone (i.e on the belly).

If the patient is in such extreme pain, place pillows under the abdomen for support, gradually increase the amount of extension by removing pillows.
Progress by having the patient prop himself up on the elbows, allowing the pelvis to sag.
Wait for 5-10 minutes between each increment of extension to allow for reduction of water content and size of the bulge. Progress by having patient prop on the hands.
If sustained postures are not well tolerated, have the patient perform passive lumber extension intermittently by repeating the prone press-ups.
(ii) Lateral shift correction:
If the patient has a lateral shift, first correct lateral shift then start with extension exercises.
The therapist stands on the side to which the thorax is shifted and places his shoulder against the patient’s elbow which is flexed against the rib cage.
The therapist wraps the arms around the patient’s pelvis and pulls the pelvis towards him while pushing the patient’s thorax away.
Self-correction:
The patient places the hand on the side of the shifted rib cage on the lateral aspect of the rib cage and place the other hand over the crest of the opposite ilium.
Then gradually push these regions towards the midline and hold.
(b) Anterior protrusion:
(i) Correction of lateral shift: The patient stands in front of a chair and places the leg opposite to the shift on a chair so the hip is in about 90 degrees of flexion. The leg on the side of the lateral shift is kept extended. The patient then flexes the trunk onto the raised thigh and applies pressure by pulling on the ankle.
(ii) Passive flexion: Bring both knees to the chest and hold this position with an arm around the thighs.
(c)Active range of motion exercises within pain-free range to the lower limb can be done e.g ankle toe movements, heel drag, hip abduction/adduction.
(d) Mobilization of thoracic spine Mobilization of segments above and below the affected segmental level.
(e) Piriformis muscle stretching
(f) Maintain/ improve mobility of neural tissues- These exercises should be performed with caution in the acute stage, usually in a recumbent position. These will prevent chronic complications from increased neural tension e.g passive SLR with foot dorsiflexion.
(g) Hydrotherapy exercises
(h) Patient education-
These are some movements you should try to avoid:
- bending over to lift very heavy items
- performing squats with too much weight
- low back extensions, as they put high-stress levels on discs
- running, since it can place strains on the discs
- any form of resistance training
Sub-acute Phase of Prolapsed intervertebral disc:
Usually, the acute symptoms decrease in 4-6 days.
(a) Continue with the exercises done in the acute phase e.g prone press-ups, nerve mobility exercises, modalities.
(b) Simple spinal movements in pain-free ranges using gentle pelvic tilts. Pelvic rocking can be done in supine, sitting, prone lying, side-lying, standing, quadruped (cat and camel exercise). Emphasize on anterior pelvic tilt so that the spine is in extension. Pelvic rolling can be added.
(c) Isometrics of extensors but caution against holding breath and causing Valsalva.
(d) Encourage aerobic activities, walking, swimming with the patient’s tolerance.
Chronic Phase: When the disc symptoms have stabilized.
Aims:
(a) Restore range of motion.
(b) Restore muscle strength, endurance and function.
(c) Retrain kinesthetic awareness and control of normal alignment.
(d) Patient involvement and education to manage posture to prevent recurrences.
PIVD Exercises In Chronic Stage:
(a) Gentle active pain free range of motion exercises:
After 3 weeks from the onset of PIVD symptoms, start side flexion and extension in standing.
Progress to adding flexion only when the disc has healed.
(b) Stretching and flexibility exercises:
Stretching of the lumbar erector spine and soft tissues posterior to the spine ( knee to chest position).
Following any flexion exercises, conclude with extension exercises such as prone press-ups/ standing back extension.
Hamstring stretch on wall.
Quadriceps stretch.
Hip adductor stretch.
Gluteal stretch.
Isometric hip adduction.
(c) Core stability exercises:
Whenever there is a slight imbalance in the core muscles, you suffer from back pain.
Core strengthening exercises help in relieving back pain and form the base of the core stability training program.
The aim of these exercises is to provide more support to your back by strengthening the muscles of your spine.

The Bridging exercise:
Strengthens several core muscle groups – e.g buttocks, back, abs for PIVD patients.
Lie flat on back; bend knees at 90-degree angle, feet flat on the floor.
Tighten abs.
Raise buttocks off the floor, keeping abs tight.
Tighten buttocks. Shoulder to knees should be in a straight line.
Hold for a count of five. Slowly lower buttocks to the floor.
Repeat five to fifteen times.
The plank exercise:
Strengthening exercise for back, abs, and neck (also strengthens arms and legs)for PIVD patients. Lie on the stomach, place elbows and forearms on the floor. In a push-up position, balance on your toes and elbows. Keep your back straight and legs straight. (Like a plank) Tighten abs. Hold the position for 10 seconds. Relax. Repeat five to ten times. If this exercise is too difficult (as it often is for beginners), balance on your knees instead of your toes.
The Side Plank: Strengthens the obliques (side abdominal muscles)for PIVD patients. Lie on the right side. Place right elbow and forearm on the floor.
Tighten abs. Push up until the shoulder is over the elbow. Keep your body in a straight line – feet, knees, hips, shoulders, head aligned. Only the forearm and side of the right foot are on the floor (feet are stacked).
Hold the position for 10 seconds. Relax. Repeat five times. Repeat on the left side. If this exercise is too difficult, balance on stacked knees (bend knees and keep feet off the floor) instead of feet.
The Wall Squat: Strengthening exercise for back, hips, and quads in PIVD patients. Stand with your back against a wall, heels about 18 inches from the wall, feet shoulder-width apart. Tighten abs.
Slide slowly down the wall into a crouch with knees bent to about 90 degrees. If this is too difficult, bend knees to 45 degrees and gradually build up from there. Count to five and slide back up the wall. Repeat 5 -10 times.
Leg and arm raise Strengthening exercise for back and hip muscles in PIVD patients.
Lie on your stomach, arms reaching out past your head with palms and forehead on the floor.
Tighten abs. Lift one arm (as you raise your head and shoulders) and the opposite leg at the same time, stretching them away from each other.
Hold for 5 seconds and then switch sides. Repeat 5 – 10 times.
Leg lifts:
Quad Strengthening Exercise for PIVD patients.
Lie flat on your back.
Bend left knee at a 90-degree angle, keeping the foot flat on the floor.
Tighten abs.
Keep the right leg straight and slowly lift the right foot to the height of the left knee.
Hold for a count of 3. Do 10 repetitions.
Switch sides and repeat.
Basic Crunches:
upper abdominal exercise for PIVD patients.
Lie on back, knees bent, feet flat on the floor.
Do not anchor feet.
The Head and back should be in a neutral position.
A rolled-up towel may be placed under the natural curve of the lower back to provide extra support – the small of the back should be about an inch above the floor.
Place hands behind head with elbows pointing outward.
Your hands are used to support your head but do not pull your head forward.
Tighten abs.
Raise your head and shoulders off the floor – three to six inches is enough.
Look at the ceiling to help prevent tilting your head.
Keep elbows back.
Exhale when raising your torso off the floor and inhale when lowering.
Do ten-fifteen repetitions.
(d)Strengthening exercises:
Opposite Arm and Leg Extension: balancing/stabilization exercise for PIVD patients:
Strengthens muscles running downsides of the spine, back of the shoulders, hips, and buttocks.
Begin on all fours, hands directly under your shoulders and knees directly under your hips.
Keep the head aligned with the spine.
Keep buttocks and abdomen tight.
Do not arch the back. Lift one arm up and forward until it is level with the torso; simultaneously lift the opposite leg in the same manner.
Keep arm, spine, and opposite leg aligned as if they are forming a tabletop.
Balance yourself for 10 seconds then slowly return to starting position.
Switch sides and repeat.
Remember to breathe.
Do five repetitions.
Leg Lifts:
lower abdominal exercise for PIVD patients.
Lie flat on your back.
Bend left knee at 90-degree angle, keeping the foot flat on the floor.
Tighten abs.
Keep the right leg straight and slowly lift it until the right foot is at the height of the left knee.
Hold for a count of 5.
Do 5 to 15 repetitions.
Switch sides and repeat.
Backward Leg Swing:
Gluteal exercise for PIVD patients.
Stand, holding onto the back of a chair for support.
Tighten abs.
Swing leg back at a diagonal until you feel your buttocks tighten.
Tense muscles as much as you can and swing leg back a couple more inches. Return leg to the floor.
Do 10 – 15 repetitions.
Switch sides and repeat.
Abdominal strengthening exercises: Isometric abs, knee to chest, bicycle exercises.
(e) Hydrotherapy exercises for back pain:
- Warm-up, mobilizing exercises
- Stretching exercises
- Strengthening exercises
- Relaxation exercises
- Swimming workouts
(f) Patient Education:
- Teach safe movement patterns and body mechanics.
- Teach patients preventive exercises and mechanics for relief of mechanical stress in daily activities.
- Teach relaxation exercises to cope with muscle tension.
- Instruct patient on how to modify environment e.g bed, chairs, car seats, work area etc.