Monoarthritis
Table of Contents
What is monoarthritis?
Monoarthritis is inflammation of one joint identified by joint swelling, pain, warmth, & sometimes fever and periarticular erythema. Arthritis is frequently associated with joint stiffness and total loss or decreased range of motion. Often, monoarthritis can occur suddenly and cause joint discomfort that ranges from moderate to severe. The condition has several potential underlying causes, involving infection, gout, and certain autoimmune diseases.
Arthritis is a nonspecific term referring to joint pain or disease connected with physical signs of articular inflammation or degenerative change. Arthralgia is related to joint pain that is not associated with abnormal findings on physical examination. Both arthritis & arthralgia can occur in one or more joints. When a patient appears with joint pain, identifying the presence or absence of physical findings & symptom distribution is key because the differential diagnosis differs substantially based on these criteria.
Acute monoarthritis is arthritis that occurs in a single joint for less than 2 to 4 weeks and is a common presenting symptom for patients in primary care and emergency settings. Diagnosis of acute monoarthritis can be challenging & outcomes range from benign and self-limiting to chronically disabling & deadly. Clinicians in primary & emergency care must be familiar with the clinical presentation & initial diagnostic workup for this condition so that they can give appropriate initial treatment, provide timely referrals for patients more likely to have emergency conditions such as septic arthritis & identify patients at more risk for chronic disability or significant complications.
What are the causes of monoarthritis?
The causes of monoarticular arthritis could be acute or chronic. Acute causes involve infection, trauma, crystal-induced arthritis, avascular necrosis, & mechanical derangement. Chronic conditions generally cause polyarthritides (i.e., involving more than one joint) such as systemic rheumatic diseases, which include seronegative spondyloarthritis, osteoarthritis, & rheumatoid arthritis; nevertheless, polyarthritis can initially manifest as monoarthritis.
Virtually every bacterium can potentially cause septic arthritis, but depending on host risk factors, it can be distributed into gonococcal and non-gonococcal septic arthritis. Gonococcal arthritis consequence of the sexually transmitted bacteria Neisseria gonorrhea; a gram-negative diplococcus, when spread in blood, can lead to disseminated gonococcal infection. It can present as a triad of features like vesiculopustular skin lesions, tenosynovitis, & arthritis (arthritis-dermatitis syndrome). Nevertheless, disseminated gonococcal infection without skin lesions has also appeared in the literature. The risk factor for disseminated gonococcal infection includes young individuals with multiple sexual partners, complement deficiencies, HIV, menstruation disorders, intrauterine device, pregnancy, and a history of pelvic disease/surgery. The diagnosis is possible with a detailed history & physical, blood cultures, culture of synovial fluid of the affected joint, and skin lesions like the pharynx, urethra, cervix, or rectum.
Staphylococcal aureus (S. aureus) is the most usual cause of nongonococcal septic arthritis; followed by Streptococcus species and gram-negative bacteria. Septic arthritis generally affects larger joints of the body like the knee & hip, but the wrist and ankle can also be affected. Septic arthritis can develop either from hematogenous seeding because of bacteria in the blood (bacteremia), direct inoculation of the joint secondary to trauma or penetrating wounds (animal or human bite), or contiguous spread of infection from the bone into the joint cavity. The risk factors involve intravenous drug use, prosthetic joints, indwelling catheters, chronic kidney disease, diabetes, malignancy, rheumatoid arthritis, & immunocompromised patients. Septic arthritis is a medical emergency, and synovial fluid analysis with gram stain & culture are the most important steps in the diagnosis. Clinically, the collection of arthrocentesis & blood cultures should take place beforehand the administration of antibiotics. Mycobacterium & fungi are rare causes of monoarticular septic arthritis. In these cases, predisposing factors like an immunocompromised state or travel to endemic areas are generally present in the history of the patient.
Late stages of Lyme disease can also present as monoarticular arthritis and often involves the knee joint. Lyme serology is needed for the diagnosis because synovial or tissue culture is always negative. Certain viruses like hepatitis B, hepatitis C, parvovirus, Epstein Barr virus (EBV), human immunodeficiency virus (HIV), alphavirus (e.g., chikungunya virus) & Zika virus can manifest with monoarticular arthritis/ arthralgia. Most viral illnesses are self-limited; nevertheless, travel history, vaccination status, & targeted serology might be indispensable to rule out serious medical conditions like HIV and hepatitis.
Crystal-induced arthritis characteristically presents with deposition of chemical compounds, monosodium urate (MSU) in gout, calcium pyrophosphate dehydrates (CPPD) in pseudo-gout, & calcium hydroxyapatite in calcific periarthritis (calcium crystal disease). A classic gout attack includes the single joint of the lower limb usually the first metatarsophalangeal joint (podagra), or in the midfoot, ankle, or knee. Gout is an inflammatory procedure related to the formation & reversible deposition of uric acid (MSU crystals) in the joints, and extra-articular tissues of the body. Classic presenting symptoms include severe pain, swelling, erythema, & disability but rarely cause joint destruction. Risk factors comprised excessive alcohol use, male gender, dehydration, trauma, surgery, metabolic disorders, hypertension, chronic kidney disease, & drugs (hydrochlorothiazide, loop diuretics) that can predispose the patient to a gout flare. Diagnostic confirmation is with the evaluation of synovial fluid aspirate of the affected joint & visualization of intracellular MSU crystals under the polarized light. The crystals are negatively birefringent beneath polarized light.
Pseudogout is an acute attack of synovitis through the deposition of CPPD crystals in the joint. The crystals are positively birefringent under the polarized light, as shown in the joint aspirate & connective tissues of the body. Pseudogout often involves the knee joint but can also present in the ankle, shoulder, & wrist joints. Clinically, it may be associated with metabolic & endocrine disorders like hemochromatosis. Seronegative spondyloarthritis (e.g., psoriatic arthritis, reactive arthritis) can manifest as monoarthritis & likely affect joints of the lower extremity. Certain chronic conditions such as osteoarthritis, rheumatoid arthritis, & bone neoplasms might arise as monoarthritis & later involve other joints of the body.
Gonococcal arthritis is arthritis that occurs due to a gonorrhea infection and is the most common cause of monoarthritis in young, sexually active people.
If you have had a joint replacement, infection of the site around the replacement can also potentially cause monoarthritis. Contact your surgeon right away if the patient had a joint replacement and is experiencing troubling pain or signs of infection. You may need treatment with antibiotics.
Psoriatic arthritis
Occurs in 5-10% of patients who have psoriasis. The classic presentation involves the DIP(distal interphalangeal joints). Morning stiffness is present. Deformity of involved joints, dactylitis, and nail involvement is common. Well-demarcated red plaques with silvery scaling – the typical lesions of psoriasis are seen on the dorsum of the hand.
common causes:
Avascular necrosis of bone
Crystals:
- Monosodium urate
- Calcium pyrophosphate dihydrate
- Apatite Loose body
- Calcium oxalate
Hemarthrosis
Infectious arthritis:
- Bacteria
- Fungi
- Mycobacteria
- Viruses
- Lyme disease
Internal derangement
Osteoarthritis
Osteomyelitis
Overuse
Trauma
But a lot of the time, these conditions affect more than one joint. Depending on the cause, it’s possible for monoarthritis to progress to inflammation in other joints over time.
Other causes
In addition to gout & septic arthritis, there are other medical conditions that can lead to monoarthritis. These include:
- ankylosing spondylitis
- Lyme disease, which generally affects the knee joint
- osteoarthritis
- psoriatic arthritis
- rheumatoid arthritis (RA), which generally occurs in smaller joints (not the knees or hips)
- trauma due to injury
- Monoarthritis can occur in 5 to 20 % of patients whom a doctor will later diagnose with rheumatoid arthritis.
What are the symptoms of monoarthritis?
Monoarthritis tends to cause acute pain. This means the pain appears to come on suddenly, usually within hours to days.
Some monoarthritis symptoms might include:
- pain that usually worsens with movement
- swelling
- warm feeling in the joint
- weakness
- periarticular erythema,
- total loss or decreased range of motion
A wide range of symptoms depends upon the underlying cause. For example, if rheumatoid arthritis is causing monoarthritis, the patient will usually experience joint stiffness in the morning that improves in an hour or less.
Conditions like gout might not cause joint stiffness specifically in the morning. Infections causing monoarthritis may be accompanied by fever, chills, & aches.
Trauma, fracture, or a loose body is suspected when monoarthritis occurs suddenly. Monoarthritis that develops more gradually, over one or two days, is generally associated with inflammation, infection, or crystal deposition. Pain that, at first, is unrecognized but worsens gradually over days to weeks, maybe because of an indolent or asymptomatic infection, osteoarthritis, or tumor. Typically, if there is morning stiffness, as well as joint pain & restricted movement, an inflammatory type of arthritis is suspected. Pain that occurs in a periarticular area is usually related to a soft tissue disorder. If monoarthritis is chronic, usually it is related to a pre-existing joint disease. But, before monoarthritis is classified as chronic, the causes of acute monoarthritis must be considered & ruled out.
What is the classification system of monoarthritis?
Classification of acute arthritis is convenient to narrow the differential diagnosis during the diagnostic process. Common classification systems classify presentations according to the acuity location of symptoms, the presence of inflammatory symptoms & signs, and the number of joints affected.
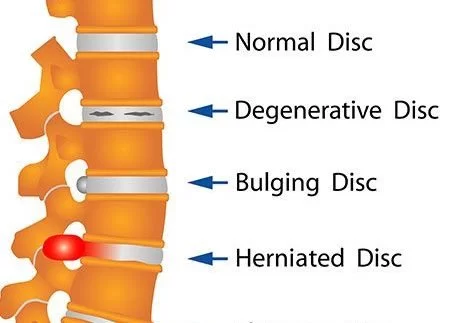
Acuity
Extremely acute onset of joint symptoms, which can happen within seconds, suggests a process that disrupted the internal structure of the joint, such as traumatic injury to the bone or soft-tissue structures. Acute onset over hours to days is the most usual time frame for acute inflammatory processes, such as septic or crystal-induced arthritis. Slow onset over days to weeks usually represents osteoarthritis, tumors, infiltrative disease, or more indolent infections. Longstanding symptoms might occur because of a monoarticular process or a monoarticular exacerbation of the polyarticular disease.
Inflammatory symptoms and signs
Inflammatory joint symptoms might be infectious, crystal-induced, immune-related, or reactive. The presence of synovitis is significant in inflammatory arthritis. Characteristic findings of synovitis involve warmth over the joint, joint effusion, & pain with movement. Inflammatory processes, especially systemic rheumatic diseases, commonly are related to joint pain with inactivity & morning stiffness lasting more than 30 to 60 minutes. The noninflammatory procedure can be because of trauma, repetitive use, degeneration or ineffective repair, neoplasm, & pain amplification. Noninflammatory processes are related to joint pain that increases with prolonged use and usually is not associated with morning stiffness.
Location of symptoms
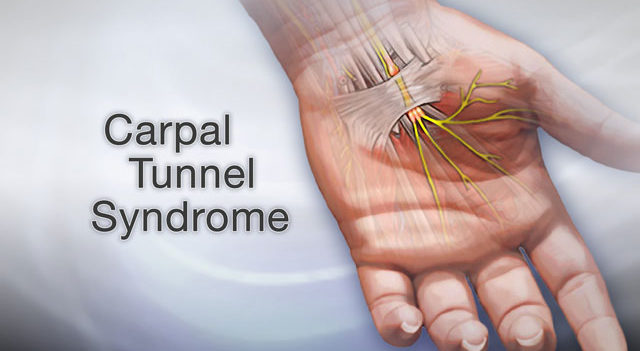
Patients who present with joint pain might have pathology in intra-articular and periarticular structures. Intra-articular pathologic procedures originate in the synovium, synovial fluid, articular cartilage, intra-articular ligaments, and joint capsule. Pathologic processes including these structures involve septic arthritis, crystal-induced arthritis, & systemic rheumatic diseases. Periarticular structures involve supporting structures such as bursae, tendons, ligaments, muscles, fascia, bone, nerves, & overlying skin. Pathologic processes involving these structures involve bursitis, tendonitis, sprains, strains, and others. Pain that arises from intra-articular structures significantly is deep, worsens with movement of the joint & weight bearing, improves with joint rest, and is maximal at extremes of joint motion. Associated swelling is common with intra-articular pathology. Pain that happens with joint movement is more likely caused by pathology in periarticular structures. Vaguely localized pain in the proximity of the joint might be due to referred pain from a distant source, such as shoulder pain related to angina, or a lesion in the surrounding bone. Another difference between intra-articular & periarticular processes is that intra-articular processes are usually related to reductions in both active and passive range of motion; periarticular processes are associated with reductions in active range of motion only.
The area of the joint also can give diagnostic clues. Crystal-induced arthropathies significantly affect the first metatarsophalangeal joint & the knee. Septic arthritis usually involves the knee or hip. Rheumatoid arthritis significantly occurs in smaller, peripheral joints.
Number of joints involved
Monoarthritis, by definition, includes only one joint. Nevertheless, monoarthritis might be the starting presenting symptom for oligoarthritis which involves two to four joints, or polyarthritis, which affects five or more joints. This most commonly occurs with rheumatoid arthritis & seronegative spondyloarthropathies. Monoarticular or oligoarticular presentations occur in 5% – 20% of patients ultimately diagnosed with rheumatoid arthritis. Additionally, a patient with an established polyarticular process might develop acute monoarthritis, defined as pain in one joint that is out of proportion to pain in other joints.
Associated symptoms
The presence or absence of certain features can narrow the differential diagnosis of monoarticular arthritis. For example, a sensation of “giving way” or “locking” of a joint in addition to joint pain & swelling suggests ligament or cartilage disruption or a loose body in the joint. Weakness in relation to joint pain & swelling advocates a neuromuscular cause for the symptoms. If the weakness is related to altered sensation, pathology is likely to present in an associated nerve root or peripheral nerve. Fever can be an accompanying symptom of acute monoarthritis; nevertheless, it is not specific to a particular diagnosis. However, the presence of constitutional symptoms, such as fever & weight loss, in combination with systemic symptoms, such as dermatologic, ocular, & vascular manifestations, recommends the presence of systemic rheumatic disease. The combination of arthritis, urethritis, diarrhea, conjunctivitis, & dermatitis suggests reactive arthritis, a subtype of seronegative spondyloarthropathies. The presence of psoriatic nail changes or plaques recommends psoriatic arthritis, another subtype of seronegative spondyloarthropathy. Symptoms of ocular inflammation & back pain in addition to peripheral joint pain and swelling suggest ankylosing spondylitis, a form of seronegative spondyloarthropathy.
What are the complications of monoarthritis?
Septic arthritis without treatment might rapidly lead to severe complications such as:
- osteomyelitis
- necrosis
- bony erosions
- fibrous ankylosis
- sepsis
- death
Gout can lead to:
- joint damage/deformity
- tophi
- kidney stones
- renal failure
What is the differential diagnosis of monoarthritis?
The most important feature of the diagnosis of monoarticular arthritis is to differentiate joint pain from soft tissue conditions like bursitis or tendinitis that tend to mimic similar symptomology. The timing of symptoms is particularly crucial in this regard. For example, the rapid onset of monoarticular pain in seconds or minutes can be signs of trauma, fracture, dislocation/derangement, or the presence of a loose body in the joint.
Pain that has onset over several hours to days generally indicates infection or crystal-induced arthritis, whereas pain over days to weeks might be an early sign of chronic conditions like osteoarthritis or rheumatoid arthritis. Certain factors like intravenous drug usage or patient on immunosuppression medications can potentially increase the risk of septic arthritis. A Triad of symptoms, including urethritis, conjunctivitis, & arthritis after infection is a telltale sign of reactive arthritis.
What is the diagnostic procedure for monoarthritis?
Physical Examination
When a patient complains of joint pain, the first step is to determine whether the cause of the pain is the joint or a periarticular soft tissue structure such as a bursa or tendon. It is not uncommon to find that “hip pain” actually is the outcome of trochanteric bursitis. Asking the patient to point to the exact area might be helpful. Unlike true joint inflammation, redness or swelling usually is not present with periarticular pain. Nevertheless, a patient with inflammation of certain bursae i.e., prepatellar bursitis, and olecranon bursitis might present with redness or swelling that mimics joint inflammation.
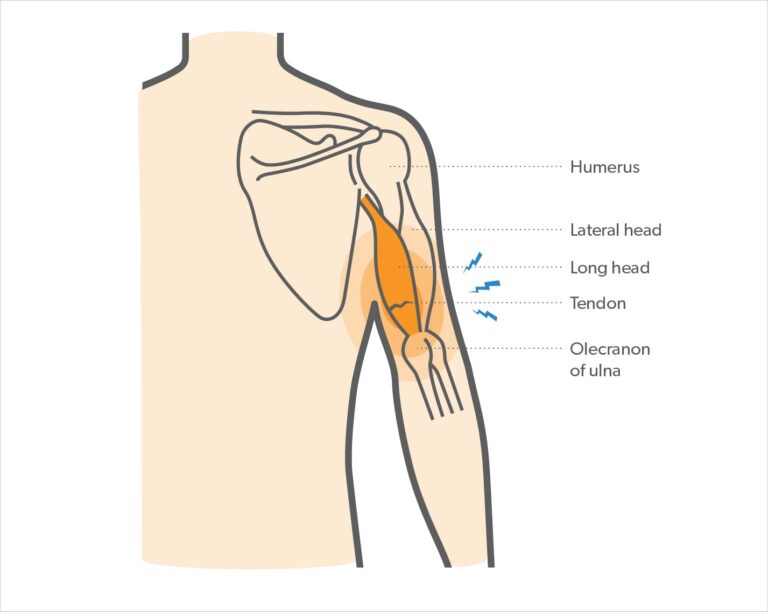
True intraarticular problems cause restriction of active & passive range of motion, whereas periarticular problems resist the active range of motion more than the passive range of motion. Maximum pain at the limit of joint motion is a feature of true arthritis. In tendonitis or bursitis, joint movements against resistance obtain pain. For example, elbow pain resulting from septic arthritis occurs with active & passive motion in any direction. In contrast, elbow pain coming from lateral epicondylitis i.e., “tennis elbow” worsens with resisted active extension or supination of the wrist. Specific maneuvers can be diagnostic for other conditions, such as medial epicondylitis; bicipital & rotator cuff tendonitis; trochanteric bursitis; & patellar, prepatellar, and anserine bursitis.
Perform a thorough examination of the symptomatic joint & surrounding area, the contralateral joint, and a general screening examination to identify additionally affected joints & systemic manifestations. Involve inspection, palpation, range-of-motion testing, assessment of stability, & strength, & sensory testing in the examination. On joint inspection & palpation, the patient might have soft-tissue swelling secondary to edema in periarticular structures, synovial thickening, & joint effusion. The joint effusion might be difficult to appreciate on examination but is important to detect because it signals intra-articular pathology. Special techniques can be used to detect effusion in various joints.
The physical examination should localize the origin of pain to periarticular or intra-articular structures. Point tenderness and tenderness over periarticular structures can occur with pathology in tendons or bursae, such as tendinitis or bursitis. Tenderness situated over the entire joint can indicate inflammatory arthritic processes such as gout or rheumatic disorders. Noninflammatory joint disorders, such as osteoarthritis, tend to be non-tender to palpation. Reduced active & passive range of motion suggests synovitis, structural joint abnormality, or soft-tissue contracture. Reduced active range of motion & preserved passive range of motion suggests a periarticular soft-tissue disorder such as bursitis or tendinitis.10 Tenderness to palpation along the course of a tendon and pain produced when the tendon is stretched or stressed during the range of motion and strength testing suggests pathology in the tendon. The presence of instability suggests ligamentous injury or tear. The feeling of crepitus with joint motion in relation to joint pain can signify articular surface abnormalities or synovitis; however, crepitus without associated joint pain often is a benign finding.
The joint effusion may not be readily visible. In the knee joint, the “bulge sign” can show a small effusion. The medial or lateral compartment is stroked, & the fluid moves through the suprapatellar site into the opposite compartment, resulting in a visible bulge. To detect effusion in the elbow joint, the triangular recess is the area between the lateral epicondyle, olecranon process, and radial head in the lateral aspect should be palpated. To search for effusion in the ankle, the joint should be palpated anteriorly. Maneuvers for examining other joints are reviewed somewhere else.
Joint pain might be referred from internal organs, i.e. shoulder pain in a patient with angina. Referred pain should be imagined in patients with a normal joint assessment.
The general physical examination might provide other diagnostic clues or reveal the involvement of other joints. Fever & tachycardia might signal infection, but they are not reliable indicators, especially in immunocompromised patients & patients who are taking corticosteroids or antibiotics. Patients with gonococcal infection might own a rash, pustules, or hemorrhagic bullae. Patients with longstanding gout might have tophi i.e., firm subcutaneous deposits of urate over the olecranon prominence, first metatarsal joints, or pinnae. Patients with reactive arthritis might have inflamed eyes. A new cardiac murmur & splinter hemorrhages in the nail folds advocate endocarditis.
Diagnostic evaluation
Diagnostic testing should refine & confirm suspected diagnoses based on information obtained during the health history & physical evaluation. Synovial fluid analysis is the key diagnostic test to assess acute monoarthritis and is needed if septic arthritis is a diagnostic possibility. Arthrocentesis, the process performed to remove synovial fluid for analysis, can be both diagnostic and therapeutic in some patients because removing excess fluid can relieve symptoms and control infection.
Synovial fluid analysis should involve gross analysis of fluid appearance, white blood cell (WBC) count with differential, Gram stain, culture, & polarized light microscopy to evaluate for septic & crystal-induced arthritis. Normal synovial fluid is clear. Inflammatory changes lead to the synovial fluid becoming cloudy and opaque; noninflammatory pathologic processes in synovial fluid can result in a clear or cloudy appearance. WBC counts in inflammatory synovial fluid are significantly elevated, with associated increased percentages of polymorphonuclear cells. Isolation of infectious agents is more likely to happen in patients with nongonococcal septic arthritis compared with those with gonococcal septic arthritis. If clinical suspicion of infection stays high and initial cultures fail to isolate a pathogen, repeat & confirm the cultures.
Recognizing crystals is important for the diagnosis of crystal-induced arthritis. Nevertheless, crystals can be difficult to identify depending on the skill of the observer. Polarized light microscopy might not be available in certain clinical settings & tentative diagnosis can be made if crystals are identified using an ordinary light microscope. The needle-shaped monosodium urate crystals related to arthritis caused by gout are more easily identified with an ordinary light microscope than are the calcium pyrophosphate dihydrate crystals related to pseudogout. Remember that crystal-induced arthritis can exist in relation to other arthritic processes, including septic arthritis, so the identification of crystals does not rule out concurrent infection.
Additional laboratory testing might aid the diagnostic approach. For example, increased serum uric acid levels suggest a possible diagnosis of gouty arthritis; nevertheless, gouty arthritis can develop with normal or elevated serum uric acid levels.
Routine blood & urine tests, such as metabolic panels, complete blood cell count, & urinalysis, should be performed when the systemic disease is suspected based on the patient’s clinical symptoms. Leukocytosis might be found in patients with septic arthritis but is a nonspecific finding.
Acquire blood cultures in patients with suspected septic arthritis. Additional cultures of the pharynx, urethra, cervix, or rectum might be indicated for suspected cases of gonococcal arthritis.
Rheumatic laboratory tests, such as erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), rheumatoid factor, anticitrullinated peptide antibody (anti-CCP), & antinuclear antibody (ANA), should only be ordered after other acute inflammatory & noninflammatory processes have been excluded based on patient history, physical examination, and synovial fluid analysis. ESR and CRP are nonspecific and can be increased in patients with infection, inflammation, or malignancy. Inflammatory markers, such as ESR and CRP, can be useful to distinguish between inflammatory & noninflammatory causes for acute monoarthritis when this distinction cannot be determined clinically.
Rheumatoid factor & anti-CCP antibodies should only be ordered when there is at least a moderate doubt for the diagnosis of rheumatoid arthritis. Rheumatoid factor is nonspecific & can be identified in low levels in up to 15% of healthy patients. Additionally, the presence of the rheumatoid factor can be related to other diseases, including Sjögren syndrome, systemic lupus erythematosus, pulmonary diseases, & infectious diseases. Anti-CCP is much more specific but less sensitive than rheumatoid factor.
Avoid ANA testing in patients who present with localized joint pain that is not related to systemic symptoms; up to 30% of healthy patients might have positive ANA at very low titers. The presence of high ANA titers can decrease the risk of false positives; nevertheless, these antibodies also are seen in patients with other systemic & organ-specific autoimmune disorders, infectious diseases, & malignancies. The American College of Rheumatology suggests that clinicians avoid ordering bundled arthritis laboratory panels because of the high frequency of false-positive test results.
Diagnostic imaging:
Plain radiographs, bone scintigraphy, CT, ultrasound, & MRI are common imaging tools to assess acute musculoskeletal complaints.
Plain radiography frequently is the initial imaging study of choice & is indicated after significant trauma, when pain is not relieved following conservative therapy, and when the patient has a history of malignancy. Acquire radiographs of the affected and contralateral joints. Despite the frequency with which plain radiographs are utilized in the clinical setting, they are nondiagnostic in most cases. Identification of erosive disease on early radiographs is a poor prognostic factor & indicative of future disability. Chondrocalcinosis might be seen on plain radiographs & is suggestive, but not diagnostic, of pseudogout.
Radiographs should be done as a baseline study for patients with confirmed and suspected septic arthritis; nevertheless, they have low sensitivity and abnormal radiographic findings are nonspecific for septic arthritis. Arthrocentesis is the only way to definitively diagnose septic arthritis; nevertheless, radiographs give supplemental information about disease severity & complications. Initial changes that might be seen on radiographs in patients with septic arthritis are soft-tissue swelling, followed by joint space narrowing. Chronic infection frequently leads to more destructive changes. CT & MRI scanning is more sensitive and specific imaging modalities for this condition and might be required.
CT, ultrasound, & MRI improve visualization of intra-articular and periarticular soft-tissue structures. Bone scintigraphy is optimal for evaluating bone turnover. These advanced imaging studies can help refine the diagnosis of monoarthritis in patients who are difficult to diagnose, and often are utilized in follow-up evaluation of patients with acute monoarthritis but are rarely indicated at initial workup.
What is the treatment plan for monoarthritis?
Most patients who present with acute monoarthritis can be treated conservatively with activity modification, local care, & appropriate analgesia. Recognizing patients who need emergency care is critical: septic arthritis, fracture, compartment syndrome, osteomyelitis, necrotizing fasciitis, tumors, & systemic vasculidities can cause acute joint symptomatology.
Patients who might have any of these conditions should be referred immediately to an appropriate specialist. Urgently refer patients with internal derangement related to severe pain, poor function, or instability, & patients with suspected acute tendon or muscle rupture.
The American College of Rheumatology advocates timely referral for patients with
undiagnosed multisystem or systemic rheumatic disease
undiagnosed synovitis, in patients who repeat arthrocentesis or synovial biopsy, might be needed
musculoskeletal pain that did not diagnose after 6 weeks
unexplained immunochemical test abnormalities advocative of underlying rheumatic disease
musculoskeletal pain not appropriately controlled with therapy
musculoskeletal pain related to severe or progressive loss of function or work productivity
conditions for which treatment with corticosteroids or immunosuppressive drugs is being contemplated
dysfunction out of proportion to objective findings.
Monoarthritis treatments depend upon the underlying cause. There are some times when monoarthritis can be a crisis. This involves if septic arthritis or another acute infection is suspected.
Other times, healthcare professionals will usually treat you with conservative measures.
Medical treatment for monoarthritis:
Treatment will depend on the cause of monoarticular arthritis. Empiric antibiotics are required for septic arthritis based on likely cause, which will later be tailored based on synovial fluid cultures. Give analgesia for gout & pseudogout within 24 hours of symptom onset for the best outcome. Corticosteroids, (NSAIDs) non-steroidal anti-inflammatory drugs & colchicine are equally effective in managing acute flares of gout & pseudogout with NSAIDs being the first-line treatment. NSAIDs are the first-line treatment with indomethacin, historically being the first-line choice, but no proof exists for its superiority to other NSAIDs.
Colchicine is another treatment choice but does not provide analgesia & is less effective if given beyond 72 to 96 hours after symptoms start. It should be utilized with caution in patients with hepatic or renal impairment, & side effects involve nausea, vomiting, & diarrhea. Another second-line treatment for those who cannot tolerate NSAIDs is corticosteroids. Caution is necessary when using corticosteroids with patients with diabetes mellitus as it can alter their blood glucose levels.
When to seek care
Definite causes of monoarthritis are medical emergencies, especially if accompanied by symptoms other than joint pain. Seek immediate medical management for monoarthritis if :
the patient has recently had surgery and experienced sudden pain, swelling, warmth, or redness in the joint, which can be a sign of infection
Patients have a high fever along with arthritis symptoms, which can also indicate possible infection
you have joint pain & swelling after an injury — you might have a fracture or sprain that requires attending
Even if you don’t think your pain is an emergency, consider making an appointment with the doctor if your symptoms interfere with your quality of life. Pain, swelling, or redness in a joint should always be assessed by a professional.
Physiotherapy treatment for monoarthritis:
Patients with monoarthritis are usually treated initially in the inpatient hospital setting & require an interprofessional team of caregivers including the primary care provider, physical & occupational therapist, nurses, & wound care team. At the time of discharge, some patients can return home while others with increased debility might need ongoing physical therapy at either an acute or subacute rehabilitation facility. The social workers in the hospital help to make sure a smooth transition from inpatient to outpatient care.
The initial treatment of infectious arthritis is outside of the role of physical therapy. It is important, first, for the physical therapist to acknowledge the signs & symptoms of the infection and refer out for other medical treatment. Subjective history, in sequence with the physical therapist’s objective findings, is important in order to recognize the risk factors that make septic arthritis the likely diagnosis. It is important to immobilize the joint in this stage to best treat the patient’s pain & to decrease the likelihood of doing further damage to the joint until proper treatment can occur.
Once the patient receives a round of antibiotic treatment in combination with either joint aspiration, debridement, or arthroscopy, the patient might then be referred back to physical therapy including
educate the patient on how to properly protect the affected joint.
Gentle mobilization of the infected joint can start if the patient is responding well following 5 days of medical treatment.
Once the infection is well-treated, current evidence states the patient will usually respond well to aggressive physical therapy to allow maximum post-infection functioning.
Physical therapy needs to consist of allowing the joint to be in its functional position & positioning the joint to allow a passive range of motion activities.
Cryotherapy or a cold pack helps to reduce swelling. For cold therapy, application equipment is cold packs, ice, nitrogen spray, and cryotherapy.
Electrical Stimulation–Transcutaneous electrical nerve stimulation (TENS) therapy is the most usual form of electrotherapy used to treat arthritis. Studies have reported that patients feel less pain after receiving TENS therapy once a week for approximately a month.
All patients require follow-up to ensure that the condition is not worsening. Some patients might benefit from temporary offloading of the extremity, & others might require an ambulatory device. Physical therapy is recommended for all patients to regain muscle strength & joint function.
Monoarticular arthritis needs an interprofessional team approach, involving physicians, specialists, therapists, specialty-trained nurses, and pharmacists, all collaborating across disciplines to achieve optimal patient results
What is the prognosis of monoarthritis?
The prognosis of monoarticular arthritis depends on factors such as time to diagnosis, & initiation of treatment. If treatment is delayed, septic arthritis can lead to joint degeneration & permanent damage. If septic arthritis affects an artificial joint, complications might include joint loosening or dislocation.
Conclusion
Acute monoarthritis is a common condition for patients & has a wide range of causes, from benign to life-threatening. Clinicians in primary & acute settings require to be comfortable obtaining a complete patient history & physical examination in order to select appropriate diagnostic tests to narrow the differential diagnosis to a single, working diagnosis.
Clinicians also require to recognize which patients can be treated conservatively & which require emergency or timely referral to specialists to minimize adverse consequences & future disability.
Hence, it can be winded up that patients suffering from arthritis can get immense relief upon consulting a physiotherapist. Advancements are continually being made on the part of PT to improve the quality of life in patients affected with arthritis.
In acute monoarthritis, Septic arthritis is the worst case with the worst outcomes
Therefore, the patient should assume it is until you they reached a thresh hold to rule it out
3 good rules for Acute Monoarthritis.
Rule out specific joints!
FAQ (Frequently asked questions)
What is the difference between polyarthritis and monoarthritis?
The involvement of only one joint is referred to as monoarthritis. Oligoarthritis is the inclusion of 2 to 4 joints. Polyarthritis is the inclusion of five or more joints.
Is osteoarthritis monoarthritis?
Osteoarthritis is a degenerative condition commonly involving the knees and hips. It results from erosion of the cartilage protecting the bones from rubbing each other. Osteoarthritis is, in fact, polyarthritis, but it starts initially in one joint before the inclusion of other joints, hence, mimicking monoarthritis.
What is the prognosis of septic arthritis?
If treatment is delayed, septic arthritis can lead to joint degeneration & permanent damage. If septic arthritis affects an artificial joint, complications might include joint loosening or dislocation.