Spine mobilization
Table of Contents
What is Mobilization for the spine?
- Spine mobilization is a passive, skilled, manual therapy maneuver applied to joints and related to the soft tissue at various speeds and amplitudes taking physiological or accessory movement for therapeutic purposes
- small amplitude potency applies at a fast velocity, and a large amplitude force applies at to slow velocity
- it is a manual method that includes applying the target forces on a painful, stiff or otherwise neglected joint in addition to upgrading its overall function. Which is not appropriate in all situations, joint mobilizations/manipulation help improve the range of motion, reduce pain, and reduce stiffness.
- Joint mobilization is a hands-on treatment that is repeatedly executed by physical therapists and healthcare professionals who master rehabilitation for movement disorders and chiropractors, health professionals treating disorders of the musculoskeletal system that involve bones, muscles, soft tissue, ligaments, etc.
Introduction for spine
- A healthy spine has three natural curves that generate an S-shape. These curves absorb shocks to your body and defend your spine from injury. Many different parts create the spine:
- Vertebrae: The spine has 33 disfigured vertebrae (small bones) that form the spinal canal. The spinal canal is a tunnel that mansion the spinal cord and nerves, defending them from injury. Most vertebrae move to permit a range of motion.
- Facet joints: These spinal joints have cartilage (a slippery connective tissue) that permits vertebrae to slide in opposition to each other. Facet joints let you twist and turn, giving flexibility and stability. These joints can establish arthritis and cause back pain or neck pain.
- Intervertebral disks: These flat, round cushions lie between the vertebrae and act as the spine’s shock absorbers. Each disk has a soft, gel-like center (the nucleus pulposus) enclosed by a flexible outer ring (the annulus). Intervertebral disks are under constant pressure. A herniated disk can tear, permitting some of the nucleus’s gel substance to leak. Herniated disks also called bulging, slipped, or ruptured disks can be awful.
- Spinal cord and nerves: The spinal cord is a column of nerves that passes through the spinal canal. The line expands from the skull to the lower back. Thirty-one pairs of nerves branch out over vertebral openings in the neural foramen. These nerves take out messages between the brain and muscles.
- Soft tissues: Ligaments connect the vertebrae to grasp the spine in position. Muscles support the back and help you move in forward and backward. Tendons attach muscles to bones and aid movement.
What are the spine segments?
The 33 vertebrae compose five specific spine segments. Starting at the neck and going down toward the buttock’s rear end, these segments include
- cervical spine
- thoracic spine
- lumber spine
- sacrum
- coccyx
Cervical spine
- Cervical spine (neck): The top part of the spine has seven vertebrae C1 to C7. These neck/cervical vertebrae permit you to turn, tilt, and nod movement of your head. The cervical spine generates an inward C-shape termed a lordotic curve.
ligaments of the cervical spine
- The ligaments are strong fibrous bands that grasp the vertebrae together, stabilize the spine and shield the discs. The three major ligaments of the spine are the ligamentum flavum, anterior longitudinal ligament, and posterior longitudinal ligament The Anterior longitudinal ligament and posterior longitudinal ligament are continuous strap-like shapes that travel from the top of cervical vertebrae to the bottom of the spinal column along the vertebral bodies. They inhibit exaggerated movement of the vertebral bones. The ligamentum flavum connects the lamina of each vertebra.
anterior longitudinal ligament
- A strong band of variable thickness and width envelope the anterior aspects of the vertebral bodies and intervertebral discs all over the length of the vertebral column. From superficial to deep its ligamentous fibers run varying lengths:
- the nethermost fibers are short intersegmental fibers
- the intermediate fibers attach two to three vertebrae
- the superficial fibers attach three to four vertebrae
- It is thick, yet narrow, through the vertebral bodies where it is loosely bound to the periosteum. At the levels of the intervertebral disc, it broadens and the fibers strongly attach to the fibrocartilage disc, the hyaline cartilage vertebral end plates, and the edge of the vertebra
- A primary spine stabilizer about one inch wide, the Anterior longitudinal ligament travels the entire length of the spine from the base of the skull, via the cervical spine, thoracic spine, and lumbar spine to the sacrum. It attaches the front side anterior of the vertebral body to the front of the annulus fibrosis.
- It’s connected to the upper and lower edges of the particular vertebral body.
- restricts the extension of the vertebral column and emphasizes the intervertebral disc.
- the area on the anterior surface of the bodies of the vertebral column.
innervation
- The anterior longitudinal ligament is supplied by recurrent branches of rami communicantes.
posterior longitudinal ligament
- The posterior longitudinal ligament is one of the three most important ligaments that contribute to stability in the spine. It passes along the posterior aspect of the vertebral body inside the vertebral canal from the body of the axis to the sacrum. The ligament is serene of longitudinal fibers that are opaquer than the anterior longitudinal ligament. However, like the anterior longitudinal ligament, the opaquer fibers are deeper and attach to one vertebra while the superficial fibers attach to three to four vertebrae. The superficial layer is an extension of the tectorial membrane at the axis, and the deep layer is an extension of the cruciform ligament at the atlas.
- The fibers are thick at the intervertebral spaces and are more enthusiast to the annulus fibrosus of the intervertebral discs than at the vertebral body where fibers are thinner. This anomaly is more observable in the posterior ligament than in the anterior. Therefore, the posterior longitudinal ligament is much more delicate than the anterior longitudinal ligament, which is significant for the disc herniations occurring posterolateral.
- The Posterior longitudinal ligament contains superficial and deep connective tissue layers, The superficial layer is the more posterior side, with its extension from the dura mater often being difficult to determine. It contains a central band of fibers 8 to 10 mm wide expanding over several vertebral segments. Due to its vast connection to the intervertebral disc, it has been termed as being ‘‘fanlike’’, allowing it a craggy appearance over each vertebral body. This craggy appearance becomes more probable in the lower thoracic and lumbar regions, where the superficial layer is of more reliable width.
- morphological variation even within the lumbar region, where both the central fibers and the ‘‘fanlike’’ portion tend to decelerate in width between L1 and L5. The deep layer, which is adherent to the superficial layer in the midline, is of more reliable diameter all over its length, being 2 to 3 mm broad at its narrowest point. It also has a craggy appearance.
- In the cervical region, the Posterior longitudinal ligament is a broad band-like structure of similar width over both the intervertebral disc and vertebral body, however more inferiorly, it becomes increasingly craggy, with its broadest part being over the intervertebral disc The divide fibers of the superficial and deep layers were difficult to identify at the level of the intervertebral disc, but their connection to the edges of the vertebral bodies and intervening annulus fibrosus was clear.
- The fibers of each and every layer arose to consolidate, forming a common connection. Both superficial and deep layers are connected to a midline bony septum on the posterior surface of the vertebral body between the superior and inferior edges. This connection was not always extended because of deficiencies in the septum in the central third of the vertebral body. The orientation of fibers without the posterior longitudinal ligament was consistent at all levels, with the fiber in the central portion of the superficial layer being more vertical than those of the ‘‘fanlike’’ portion. even if the deep layer was visible through the superficial layer
- The posterior longitudinal ligament has a more defensive than supportive role. The observed pattern of movement of foreign materials like masses and bony fragments following a vertebral fracture into the vertebral canal confirms that the Posterior longitudinal ligament acts to defend the spinal cord and from displaced disc material.
- Fibers of the superficial layer will restrict forward flexion, while the oblique fibers of the deep layer will restrict lateral flexion and rotation. fibers from both layers are included in all movements, with an elevating number of fibers enlisted with elevating pressure. The craggy appearance of the Posterior longitudinal ligament in the lower thoracic and lumbar regions may be due to the elevated rotational and lateral flexion forces brought out in the lower region compared with the upper regions of the vertebral column of the spine. The presence of elastin protein in the Posterior longitudinal ligament supports that it has a role in the dynamic movement of the spine. Observed patterns of disc fragment migration following vertebral burst fractures suggest that the Posterior longitudinal ligament also defends the contents of the vertebral canal.
blood supply of posterior longitudinal ligament
- The primary supply of blood to the spinal cord is in distinction to a single anterior spinal artery and the two posterior spinal arteries. These two posterior arteries are the branches of the vertebral artery in the spine. Posterior arteries supply the blood to the posterior part of the spinal cord, and the anterior portion achieves blood supply from the anterior spinal artery. adjacent to the spinal arteries, there are other arteries also available at each spinal segment called radicular spinal arteries, which derive from the body wall arteries. The small penetrating arteries exude off by both anterior and posterior spinal arteries form interrelate in the spinal cord.
- The radicular spinal arteries supply the blood anterior and posterior parts of the spinal cord. The drainage of blood from the spinal cord catch place with the aid of anterior and posterior spinal veins. These veins duct into the internal and external venous plexus. Through these plexus, the blood duct into the main venous system with the help of azygous veins, lumbar veins, and hemizygous veins
nerve supply of posterior longitudinal ligament
- The primary source of the nerve supply of the posterior longitudinal ligament is the meningeal branch borrowed from the spinal nerve. It accords ascending and descending branches in the vertebral column of the spine. There are transverse branches hammered by the synthesis of ascending and descending branches. The synthesis of the transverse branches from the adverse side makes a network of nerve fibers superficially, which animates the posterior longitudinal ligament in the vertebral segment of the spine. The posterior part of the annulus fibrosus is crossed by the nerve fibers hammering a network deep in the intervertebral part of the posterior longitudinal ligament
- There is no animation of the deep layer of the nucleus pulposus or annulus fibrosus because of the shortcoming nerve fibers and nerve terminals. some nerve terminals are present in the middle part of the nucleus pulposus, but in the peripheral zone, there are abundant nerve fibers. The abundant nerve fibers in the peripheral zone play an essential part in the regulation of movement and posture in the vertebral column of the spine.
muscle attached to the posterior longitudinal ligament
- There are three groups of muscle in the back of the spine; superficial, intermediate, and deep muscle layers. The superficial layer contains two muscles the splenius cervicis and splenius capitis. They play an essential part in the extension of the neck and the movement of the shoulder.
- The intermediate muscle group consists of the longissimus, iliocostalis, and spinalis muscles. All three muscles of the intermediate group have an equal tendinous origin. The intermediate groups of muscles help in the flexion of the head and upper vertebral column and the movement of the thoracic cage. The deep layer contains semispinalis, rotatores, and multifidus. The major function superficial intermediate and deep muscle group is the stabilization of the vertebral column and maintaining an upright posture. They also help in balance and proprioception
variants of the ligament
- the posterior longitudinal ligament is smaller and sluggish. It has an oval shape that varies from 2 to 2.25 mm in thickness at the level of L5-S1. From L5 upwards, the ligament hammers a narrow band, which broadens symmetrically at the level of each disc. The fibers of the annulus fibrosus and the edge of the vertebral body are the sites of connection of the ligament, but in some cases, not all, it is attached to the posterior aspect of the vertebra. The thickness of the ligament at the different levels is as follows.
- The posterior longitudinal ligament seems to be most developed at the level of the L3 and L4 vertebra, where its average thickness is 1.4 mm. From L2 upwards, the ligament thins considerably. There is a thicker middle portion approximately about 2.5-4 mm thickness all over the whole length of the ligament. The ligament in the central portion of each vertebral body envelops the vascular foramina
interspinous ligament
- This ligament is poised of thin sheets attaching the spinous processes from roots to apexes from C1 to S1 one segment at a time. Anteriorly, Its fibers attach with ligamentum flavum, although posteriorly its fibers attach with the supraspinous ligament. The ligaments are small and elongated in the thoracic region, broader, thicker, and quadrilateral in a form in the lumbar region, and only slightly refined in the neck. In the neck, they are generally considered part of the nuchal ligament.
- The interspinous ligaments are thin and short structures attaching adjacent spinous processes. The Interspinous ligament are well vascularized and contains sensory nerves, particularly on their posterior and lateral surfaces. These ligaments originate somewhat from the ligament Flava, somewhat from the reciprocal vertebral laminae, and somewhat from the caudal aspect of the spinous process. The lumbar Interspinous ligament is thicker and tends to be more jewel and quadrilateral in nature and generally occurs in pairs. The lumbar Interspinous ligament is usually blocked out with a fiber direction passing obliquely or horizontally in an anterior-posterior direction from the superior margin of the caudal spinous process to the cranial spinous process.
- The Interspinous ligament is part of the posterior ligamental complex, and they act as stabilizers of the spine and help to limit spine flexion.
nerve supply
- The lumbar interspinous ligaments achieve a nerve supply from the medial branches of the lumbar dorsal rami and experimental stimulation of the interspinous ligament provides low back pain and referred pain in the lower limbs. This distributes the interspinous ligament as an attractive source of low back aches.
blood supply
- The interspinous ligament is well supplied by small blood vessels and sensory nerves, the latter particularly in its posterior part and on its lateral surfaces.
movement
- The role of the interspinous ligament is to limit flexion bending forwards by restricting the separation of the spinous processes of the vertebral column.
ligamentum flavum
- The ligamentum flavum is a short but thick ligament that attaches the laminae of adjacent vertebrae from C2 to S1 and is considered a medical ward continuation of a facet joint. It consists of 80% elastin fibers and 20% collagen fibers. This high percentage of elastin fibers provides the ligament with its yellow color and flexible nature.
- Despite the elastic and flexible essence of the ligament, at the neutral position, the ligament has a hypocrisy inhibiting it from buckling. At the lumbar vertebra, this pretension is provided by the traction and tension forces applied by muscles on the Thoracolumbar fascia by the supraspinous, interspinous ligaments to ligamentum flavum causing hypocrisy in the neutral position of the interspinous supraspinous thoracolumbar ligamentous complex
- At each intersegmental level, the ligamentum flavum is a paired structure represented symmetrically on both sides.
- In the neck region, the ligaments are thin but wide and long; they are broader in the thoracic region and broadest in the lumbar region.
Attachments of the ligamentum flavum
- The ligament flavum originates from the lower half of the anterior surface of the lamina beyond and connects to the posterior surface and upper margin of the lamina beneath, hammering a cup-like grasp on the upper border of the lamina beneath.
- On each side the ligament divides into two portions:
- The medial portion: canyon to the back of the next lower lamina and astride the gap between the contiguous vertebrae fusing with the interspinous ligament
- The lateral portion: canyon in front of the facet joint where it connects to the anterior aspect of the inferior and superior articular processes and hammers the anterior capsule. Most lateral fibers expand beyond the superior articular process to the pedicle beneath.
Function
- The marked elasticity provides to preserve the upright posture and assists the vertebral column in reopening its shape after flexion. It resists excessive separation of the contiguous vertebral lamina and inhibits buckling of the ligament into the spinal canal during extension, inhibiting canal compression. The lateral portion of the ligament inhibits the anterior capsule of the facet joint from being cached without the joint cavity during movement.
Alar ligament
- Two strong rounded cords attach the skull to C2 (Axis).
attachment of the alar ligament
- origin from either side of the odontoid process and connect to the medial aspect of the occipital condyle
Function
- firm in flexion, limit rotation, and side flexion to the opposite side.
- Play a role in stabilizing the C1 and C2 vertebrae of the cervical spine, especially in rotation
intertransverse ligament
- the intertransverse ligaments are ligaments that are placed in the middle of the transverse processes of the spine.
- In the cervical region, the intertransverse ligament consists of a few irregular, scattered fibers that are often recouped by muscles. In the thoracic region, they are rounded cords intimately attached to the deep muscles of the back. In the lumbar region, the intertransverse ligament is thin and membranous.
- The intertransverse ligaments generally combine with the intertransverse muscles.
- The function of the intertransverse ligaments is to restrict lateral flexion of the spine.
Apical ligament of dens
- spans in the middle of the second cervical vertebra in the neck and the skull. It lives as a fibrous cord in the triangular interval in the middle of the alar ligaments.
- The ligament was on average 7.5 mm long and 5.1 mm broad. Structurally, the ligament is a small gathering of elastic fibers encompassing a core of notochordal particles essentially it represents a rudimentary nucleus pulposus that is the particle of notochord seen at other vertebral levels.
attachments
- origins from the tip of the odontoid process on the Axis generally hammer a small coronal groove located there and inserts into the anterior rim of the foramen magnum at the base on the mid-point.
- The apical ligament is detached anteriorly from the anterior atlantooccipital membrane by a thin layer of fat and connective tissue. Posteriorly it is separated from the superior crus of a cruciform ligament by an intervening layer of connective tissue. The tectorial membrane is established further dorsally, posterior to the cruciform ligament. Laterally the alar ligaments expand from the odontoid to the medial aspect of the condyles of the occipital bone. There is no accordant contact in the middle of the alar ligament and the apical ligament.
function
- The apical ligament is a small ligament that connects the apex tip of the dens of the C2 vertebra to the anterior margin of the foramen magnum. It is the weak, fibrous particle of the notochord and does not devote significantly to stability.
Nuchal ligament
- the nuchal ligament is located on the back of the neck Continuous with the Supraspinous ligament. It hammers a two-layered fibroelastic septum that separates the dorsal muscles of the neck and spans from the spine of the C7 vertebra to the occiput bone.
attachments
- Extension from the external occipital protuberance on the skull and median nuchal line to the spinous process of C7 vertebrae. The deep fibers of the ligament connect to the external occipital crest, the posterior tubercle of the atlas, and to the medial surface of the bifid processes of the other cervical vertebrae.
Function
- Limits flexion
- gives a connection between Trapezius and Splenius capitis.
supraspinous ligament
- The supraspinous ligament or supraspinal ligament is a strong fibrous cord that attaches together with the apices of the spinous processes from the seventh cervical vertebra to 3rd or 4th lumbar vertebrae. From the C7 vertebra to the skull ligament turn in to structurally specific from more caudal parts of the ligament and is called the ligamentum nuchae
- Origin: It originates from the C7 vertebra.
- Insertion/Terminates: Sacrum
- The supraspinous ligament is fully grown only in the upper lumbar region and may terminate at L3 vertebrae, despite the most common termination site tending to be at L4 vertebrae. The supraspinous ligament is almost always absent at L5/S1 vertebrae.
- It is thicker and broader in the lumbar region than in the thoracic region, it combines with the thoracolumbar fascia.
- The most superficial fibers of the supraspinous ligament expand beyond three or four vertebræ; those more deeply seated ligament pass in the middle of two or three vertebræ while the deepest connect the spinous processes of relative vertebrae
- The deep layer of the supraspinous ligament is assisted by tendinous fibers of the multifidus muscle. in the middle of the spinous processes, it is extended with the interspinal ligaments. The supraspinous ligament’s middle fibers connect with the thoracolumbar fascia’s dorsal layer.
Function
- Limits flexion along with other ligaments of the vertebral column.
- The supraspinous ligament contributes as a midline connection for some important muscles.
- The supraspinous ligament aids in maintaining the upright position of the head.
- It’s stretched in flexion, its fibers resist separation of spinous processes during forward flexion, and during hyperflexion, the interspinous ligament and supraspinous ligament are the first to fail.
- At the lumbar region, through the attachment of the supraspinous ligament to the thoracolumbar fascia and interspinous ligament, they form together Interspinous_supraspinous thoracolumbar ligamentous complex which it`s function is to move tension that is located on Thoracolumbar fascia to ligamentum flavum causing pretension in the neutral position
Anterior atlantooccipital membrane
- The anterior atlantooccipital membrane also termed the anterior atlantooccipital ligament is wide and unruffled of dimly woven fibers, which pass in the middle of the anterior margin of the foramen magnum beyond, and the upper border of the anterior arch of the atlas beneath. It is an extension of the anterior longitudinal ligament.
- Laterally, it is an extension of the articular capsules. In front, it is strengthened in the middle line by a strong, rounded cord, which attaches the basilar part of the occipital bone to the tubercle on the anterior arch of the atlas.
- The anterior atlanto occipital membrane is in relation in front with the rectus capitis anterior muscles, back of the alar ligaments.
- Type: Synovial ellipsoid joint; biaxial
- Articular surfaces: Occipital condyles, superior articular facets of the atlas
- Ligaments: Posterior atlantooccipital ligament, anterior atlantooccipital ligament
- Innervation: C1 spinal nerve
- Blood supply: Anastomosis between deep cervical, occipital and vertebral arteries
- Movements Principal movement: Flexion – extension
- Limited lateral flexion
cruciate ligament of the atlas
- The cruciform ligament of atlas cruciate may another form of the cruciform ligament is a cruciate ligament in the neck hammering part of the atlantoaxial joint. The ligament is named cruciate as such because it is in the shape of an annoyed.
- It consists of two bands:
- Longitudinal band.
- Transverse band.
function
- It is an important ligament that grasps the posterior dens of the C2 vertebra in fabrication at the atlantoaxial joint. It lives back of a large synovial bursa encompassing a loose fibrous capsule and contains two bands:
- Longitudinal band: connect the body of the C2 axis to the foramen magnum
- Transverse band: connects to the inner margin of the C1 atlas lateral masses on both sides.
Transverse ligaments of the atlas
- It is concave in front, convex in back, wider and thicker in the middle than wider and thicker at the ends, and firmly connected on either side to a small tubercle on the medial surface of a lateral mass of an atlas.
- As it annoyed the odontoid process, a small fasciculus termed crus superius is prolonged upward, and another is crus inferius downward, from the superficial or posterior fibers of the ligament.
- The former is connected to the basilar part of the occipital bone, in close relation with the membrana tectoria; the recent is fixed to the posterior surface of the body of the axis; thus, the full ligament is named the cruciate ligament of the atlas.
- The transverse ligament partition the ring of the atlas into two unequal parts. the posterior and larger contributions to the transmission of the medulla spinalis and its membranes and the accessory nerves; the anterior and smaller contain the odontoid process.
- The neck of the odontoid process is cramped where it is accessible posteriorly by the transverse ligament so that the transverse ligament gets by to retain the odontoid process in position after entire the other ligaments have been separated
attachments
- It is connected on either side to a small tubercle on the medial exterior of the lateral mass of the Atlas.
- As it annoyed the odontoid process, a small fasciculus crus superius is prolonged upward and another crus inferius downward, from the superficial or posterior fibers of the ligament. The former is connected to the basilar area of the occipital bone, in close relation with the Tectorial membrane. The recent is fixed to the posterior surface of the body of the Axis; thus the whole ligament is named the cruciform ligament of the atlas.
Function
- It is a very strong, primary stabilizer for the upper cervical spine – the odontoid process will rhythmically fracture previously the ligament will tear.
- It partitions the ring of the Atlas into two unequal parts of the transverse ligament of the atlas, the posterior and larger contributions to the transmission of the spinal cord, its membranes, and the accessory nerves; the anterior and smaller contain the Odontoid process.
- It functions to inhibit anterior displacement of the C1 atlas over the C2 axis, the main stabilizer for the odontoid process inhibiting it from posterior migration.
Muscle of the cervical spine
Anterior Neck Muscles
- Superficial muscles – platysma, sternocleidomastoid
- Suprahyoids – Digastric, mylohyoid, geniohyoid, stylohyoid
- Infrahyoids – sternohyoid, sternothyroid, thyrohyoid, omohyoid
Vertebral Muscles
- Muscles form musculoskeletal columns around vertebrae. These are further divided into the anterior, lateral, and posterior vertebral muscle groups.
Anterior (Prevertebral) Vertebral Muscles
- These are also termed Deep cervical flexors:
- Rectus Capitis Anterior
- Rectus Capitis Lateralis
- Longus capitis
- Longus colli/ Longus cervicis
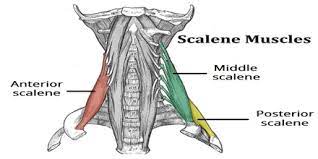
Lateral Vertebral Muscles (Paravertebral)
- Scalenes muscle – anterior, middle, posterior, and minimus scalene muscles
Posterior Vertebral Muscles
- These can be further divided into intrinsic muscles and extrinsic muscles.
Extrinsic muscle
- Trapezius and Levator scapulae
Intrinsic muscles
- Superficial muscles :
- splenius capitis,
- splenius cervicis
Deep muscles:
- Suboccipital group
- rectus capitis posterior major
- rectus capitis posterior minor
- obliquus capitis inferior
- obliquus capitis superior
- Transversospinalis muscles
- semispinalis capitis
- semispinalis cervicis
- rotatores cervicis
- multifidus muscle(these are also known as deep neck extensors)
- Interspinales and intertransversarii.
The Movements and muscles in the cervical spine
Flexion
- Longus Colli
- Sternocleidomastoid
- Scalene anterior
- Longus capitis
- Rectus capitis anterior (head only)
Extension
- Levator Scapulae
- Splenius cervicis
- Splenius capitis
- Trapezius
- Erector spinae
- The Rectus capitis posterior, major, and minor (head only)
Lateral flexion
- Scalene anterior, medius, and posterior
- Sternocleidomastoid
- Splenius capitis
- Trapezius
- Erector spinae
- The Rectus capitis lateralis (head only)
Rotation
- Semispinalis cervicis
- Multifidus
- Scalene anterior
- Splenius cervicis and capitis
- Sternocleidomastoid
- Inferior oblique (head only)
- Rectus captitis posterior major (head only)
range of the movement
- Flexion 50 degrees
- Extension 15 degrees
- Right lateral flexion 20 degrees
- Left lateral flexion 20 degrees
- Right rotation 5 degrees
- Left rotation 5 degrees
Thoracic spine
- Thoracic spine (middle back): The chest or thoracic part of the spine has 12 vertebrae from T1 to T12. Your ribs attach to the thoracic spine. The thoracic spine turns out slightly to make a backward C-shape called the kyphotic curve.
ligaments of the thoracic spine
costotransverse ligament
- The costotransverse ligament is a fibrous band between the transverse process and the neck of the rib, it’s divided into two parts: the superior and the lateral costotransverse ligaments.
- there are three types of costotransverse ligaments in the human body: costotransverse ligament connects the posterior surface of the neck of the rib with the transverse process of the corresponding vertebrae. a lateral costotransverse ligament connects the non-articular part of the rib with the tip of the transverse process and a superior costotransverse ligament connects the upper border of the neck of the rib to the inferior border of the transverse process of the vertebrae beyond. In addition, the inferior costotransverse ligament and the posterior costotransverse ligament are in this grouping.
Functions
- Support and inhibit dislocation of ribs and restrict the costotransverse joint to perform a gliding movement.
- Their posterior surfaces provide connection points for the extensor muscles’ deep group of the back.
Anterior atlanto axial ligament
- The anterior atlantoaxial ligament is a strong membrane, fixed, above, the lower border of the anterior arch of the atlas; beneath the front of the body of the axis.
- It is strengthened in the middle line by a rounded cord, which attaches the tubercle on the anterior arch of the atlas to the body of the axis, and is an extension upward of the Anterior longitudinal ligament.
- The ligament is in relation, in front, with the long capitis.
- anterior longitudinal ligament, posterior longitudinal ligament, nuchal ligament, ligamentum flavum, interspinous ligament, and supraspinous ligaments already mentioned above
Muscle of the thoracic spine
- Superficial back muscles are found just beneath the skin. Involve latissimus dorsi, the trapezius, levator scapulae and the rhomboids. Ability moves the upper limb as they arise at the vertebral column and insertion onto either the clavicle, scapula, or/and humerus.
- Intermediate back muscles – work to elevate and depress the rib cage of the spine. There are two major muscles without elevating and depressing the spine. the serratus posterior superior and/or the serratus posterior inferior.
- Back muscles – Involve Erector Spinae and Transversospinalis Group intrinsic back muscles. These muscles generally work to aid movements of the vertebral column of the spine and to also control posture.
Major Muscles of the thoracic spine
Superficial Layer
- Trapezius large back muscle connects to the vertebral column from the base of the skull to the ligamentum nuchae of the neck, again connecting to the spinous processes of the C7 vertebrae and the thoracic spine down to the T12 vertebrae. It attaches the shoulder blade to the vertebral column and acts to help the arm and assist in upper limb movement by controlling shoulder blade movements.
- Latissimus Dorsi broad back muscle travels from the spinous processes of the lower thoracic vertebrae and lumbar spine, the connective tissue fascia of the thoracolumbar region, along with the pelvis and lower ribs, to embed into the upper arm bone humerus. Its primary action is to expand, adduct, and internally rotate the upper arm bring the upper arm backward, to the side of the body, and rotate the upper arm towards the body performing a chin-up. It also consequences the movements of the shoulder blade and trunk.
- Rhomboids these muscle rhombus-shaped muscles arise from the spinous processes of cervical and thoracic vertebrae C7 to T5 vertebrae and connect to the shoulder blade. The rhomboid’s main action is to drag the shoulder blades back through scapular retraction
Intermediate Layer
- Serratus Posterior Superior is a thin, quadrilateral-shaped muscle, addressed at the upper and back part of the thoracic spine. It lives deep in the rhomboids and aids inspiration by elevating rib cages 2 to 5 where it connects.
- Serratus Posterior Inferior is addressed at the junction of the thoracic and lumbar regions. It arises from vertebrae T12 down to L3 and embeds into the 9th through to the 12th ribs. It acts to draw the lower ribs backward and downwards and helps in trunk rotation and extension. It also helps with forced expiration.
back muscle
- Thoracic Erector Spinae groups are Iliocostalis; Longissimus; Spinalis the main extensor backward-bending muscle of the thoracic spine, located on either side of the vertebral column.
- Transversospinalis Group muscles are shorter, deep muscles that help stabilize the spinal segments.
- They are situated deep to the erector spinae, run obliquely, and make up the mass of musculature that fills the laminar groove of the spine between the transverse and spinous processes.
- The transversospinalis muscle group can be separated into three subgroups: from superficial to deep, the semispinalis, the rotatores, and the multifidus:
- The Semispinalis connects superiorly to vertebrae on five or more levels beyond the inferior connection
- The Rotatores connect superiorly to the vertebrae on one to two levels beyond the inferior connection
- The Multifidus connects superiorly to vertebrae three to four levels beyond the inferior connection.
Lumber spine
- Lumbar spine (lower back): Five vertebrae L1 to L5 make up the lower part of the spine. the lumbar spine helps the upper parts of the spine. It attaches to the pelvis and lifts most of your body’s weight, along with the stress of lifting and carrying items. Many back problems happen in the lumbar spine. The lumbar spine turns inward to create a C-shaped lordotic curve.
ligaments of the lumber spine
iliolumbar ligament
- The iliolumbar ligament is a strong bond of connective tissue. and one of the three vertebropelvic ligaments. The others are the sacrotuberous and the sacrospinous ligaments. They help stabilize the lumbosacral spine on the pelvis.
- The iliolumbar ligaments are decisive in helping the lower lumbar spine; they connect the 4th and 5th lumbar vertebrae L4 and L5 to the iliac bone crest at the back of the pelvis. Injury to the iliolumbar ligament, fairly common among certain athletes due to the amount of agitated spinal motion included in many sports, can develop into sacroiliac joint pain and related problems. The sacroiliac joint is addressed in the pelvis and helps to conduct the spine’s stable
Attachments
- Origin: the transverse process of L5
- Insertion: deep into the ventral area of the iliac crest 6-7cm from the midline
- The main part of the iliolumbar ligament arises from the L5 vertebral transverse processes. insertion is protected by the crest dorsally, making it unattainable to palpation
Function
- It plays an essential role in restraining movement in the lumbosacral and sacroiliac joints. The iliolumbar ligament strengthens the lumbosacral joint helped by the lateral lumbosacral ligament, and, like all other vertebral joints, via the posterior and anterior longitudinal ligaments, the ligamentum flava, and the interspinous and supraspinous ligaments.
Sacrospinous ligament
- The Sacrospinous ligament small and anterior sacrosciatic ligament of the sacroiliac joint is a pelvic ligament. It is a thin triangular band and its length is about 3.8-4.6cm.
- The sacrospinous ligament’s fibers are interweave with the sacrotuberous ligament. Posteriorly, the sacrotuberous ligament encompasses the back of the sacrospinous ligament. Anteriorly, The sacrospinous ligament envelopes the coccygeus muscle. It is connected by the spine of the ischium and the outer margin of the sacrum and coccyx.
Attachments
- The sacrospinous ligament performs as a wider for the greater and lesser sciatic foramen. The greater sciatic foramen lives beyond the ligament and gives a path for superior gluteal nerves and vessels to combine from the pelvis while acting as a passage for the inferior gluteal vessels and nerve, sciatic and posterior femoral cutaneous nerves to encompass through and exit the pelvis.
- The lesser sciatic foramen is beneath the ligament, passing the tendon of the obturator internus, its nerve, and the internal pudendal vessels and nerve
Function
- The sacrospinous and sacrotuberous ligaments help in pelvic stability. The ligament works with the sacrotuberous ligament to inhibit rotation of the illum past the sacrum thus inhibiting excessive twisting of the pelvis, low back pain, and sacroiliac junction strain.
Sacrotuberous ligament
- The sacrotuberous ligament is a stabilizer of the sacroiliac joint and attaches the bony pelvis to the vertebral column.
- the sacrotuberous ligament Is in the shape of a fan addressed in the posterior pelvis, on both sides, and attaches the sacrum to the iliac tuberosities.
- It consists mainly of collagen fibers, it is strong enough to support the sacrum and inhibit adverse changes beneath body weight
- The Sacrotuberous ligament helps in pelvic stability, and the obliquity arrangement of the sacrotuberous ligament on both sides inhibits the anterior tapping of the sacrum by performing to control sacral nutation.
- The Sacrotuberous ligament inhibits the sacrum from tapping forward when downward pressure is applied to the spine. It is stressed with sports that generate a lot of arching in the lower back like high jumping, golfing, gymnastics, pitching, and volleyball spiking.
- attaching the lower limb with the trunk, biceps femoris, and perineum to the thoracolumbar fascia, and erector spinae.
- sacrotuberous and sacrospinous ligaments stabilize the sacrum in opposition to twisting with the pelvis, and excessive side bending. thus, an imbalance in the middle of the sacrotuberous ligament on both sides causes pelvic rotation, Sacroiliac junction strain, or LBP
- anterior longitudinal ligament, posterior longitudinal ligament,ligamentum flavum, supraspinous, interspinous, intertransverse, nuchal, apical ligament of dens, cruciate ligament of the atlas
movements of the ligament in the lumber spine
- Alar skull Head: rotation & lateral flexion
- Anterior Atlantoaxial – Extension
- Posterior Atlantoaxial – Flexion
- Ligamentum Nuchae Cervical Flexion
- Anterior Longitudinal Axis – Sacrum Extension & reinforces the front of the annulus fibrosis
- Posterior Longitudinal – Sacrum Flexion & reinforces back of annulus fibrosis
- Ligamentum Flavum – Sacrum Flexion
- Supraspinous ligament – Thoracic & Lumbar Flexion
- Interspinous ligament – Lumbar Flexion
- Intertransverse ligament – Lumbar Lateral flexion
- Iliolumbar ligament – Sacroiliac joints Stability & some motion
- Sacroiliac – Sacroiliac joints Stability & some motion
- Sacrospinous ligament- Sacroiliac joints Stability & some motion
- Sacrotuberous ligament- Sacroiliac joints Stability & some motion
muscle of the lumber spine
- multifidus
- quadratus lumborum
- psoas major
- longissimus
- spinalis
- iliocostalis
- musculus iliocostalis lumborum
- inter spinalis
- levator scapulae
- serratus posterior inferior
- intertransversarii
- transversospinales
- rhomboid major
- longissimus cervisis
- semispinalis thoracis
- semispinalis cervicis
- longus capitis
Range of movement
- Flexion 50 degrees
- Extension 15 degrees
- Right lateral flexion 20 degrees
- Left lateral flexion 20 degrees
- Right rotation 5 degrees
- Left rotation 5 degrees
- Sacrum: This triangle-shaped bone attaches to the hips. The five sacral vertebrae S1 to S5 blend as a baby develops in the uterus, which means sacral vertebrae don’t move. The sacrum and hip bones hammer a ring called the pelvic girdle.
- Coccyx (tailbone): Four fused vertebrae make up this small piece of bone found at the bottom of the spine termed the coccyx. Pelvic floor muscles and ligaments connect to the coccyx.
What conditions and disorders affect the spine?
- Vertebrae and disks can wear downward with age, causing pain. Other conditions that affect spine health involve:
- Arthritic conditions, such as ankylosing spondylitis
- cervical spondylosis
- lumber spondylolisthesis
- intervertebral disc prolapse
- Back strains and sprains.
- Birth defects such as spina bifida.
- Bone spurs jagged ends of the vertebrae that put pressure on the spinal cord and nerves.
- spinal curvatures like scoliosis, lordosis, and kyphosis.
- Neuromuscular diseases, such as amyotrophic lateral sclerosis, pseudo bulbar palsy
- Nerve injuries involve spinal stenosis, sciatica, and pinched nerves.
- Osteoporosis weak bone.
- Spinal cord injuries, including spinal fractures, herniated disks, bulging disks, and paralysis.
- Spine tumors and cancer.
- Spine infections like meningitis and osteomyelitis.
Goals for spine mobilization
pain, muscle guarding, and spasm
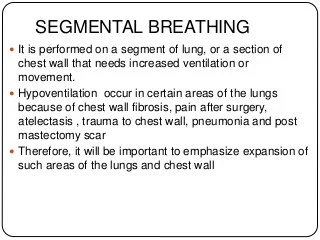
- painful joint, reflex, muscle guarding, and muscle spasm can be examined with slight joint play methods to stimulate neurophysiological and mechanical effect
Neurophysiological effect
- small amplitude oscillatory and/or distraction movement are used to encourage mechano receptors that may inhibit the transmission of nociceptive stimuli at the spinal cord or brain stem level
Mechanical effect
- minor amplitude distraction or gliding for movement of the joint is used to create synovial fluid movement, which is an agent for carrying nutrients to avascular portions of the articular cartilage
- rhythmic joint play techniques help to maintain nutrient exchange and inhibit the painful and degenerating effects of statis when the joint is swollen or/and painful, and can not go through a range of motion
- when adjusted to treat pain, muscle spasms and muscle guarding small amplitude methods should not apply stretch on the reactive tissue
Reversible joint hypomobility
- reversible joint hypomobility can be examined with a progressively vigorous joint stretching method to elongate hypermobile capsular and ligamentous connective tissue
- uninterrupted or/and distracted stretch forces helped to distend a shortened tissue mechanically
Positional faults/subluxations
- A faulty or/and incorrect position of one bony companion in addition to its opposing surface may affect the outcome in limited motion or/and pain
- positional faults can transpire with traumatic injury, after periods of immobility, muscle imbalance
- the faulty position may be conserve
- by maladapted neuromuscular control across a joint
- during examining an active range of motion, faulty tracking of the joint surface outcome in pain or/and lessened motions
Progressive limitations
- diseases that progressively restrict movement can be examined with joint play techniques to maintain available motion or/and lessen the progressive automated deduction
- the patient’s response is necessary for the dosage of distraction or/and glide to treatment and the state of the disease
Functional immobility
when the patient can’t functionally gesture the joint for a longer period
the joint can be examined with nonstretch gliding or/and distraction procedure to maintain available joint play and inhibit the degenerating and reduce the effect of immobility
Grades for spine mobilization
- grade 1 small amplitude oscillations are used for pain, modulation, typically during the acute stage of injury
- grade 2 large amplitude oscillations are used for pain modulation, dosage, and indication same for grade 1
- grade 3 large amplitude oscillation that goes up to the restrictive joint barrier,
- this grade is designed to improve joint ROM and is used only during the subacute, chronic stage of healing
- grade 4 small amplitude oscillation that goes up to the restrictive joint barrier,
- this grade is designed to improve joint ROM and is used only during the chronic stage of healing
- grade 5 (HVT) high velocity and low amplitude thrust applied at the physiologic limit of joint motion
- this grade is performed only one time and solely improves rom
Spine mobilization exercises
Mobilization for cervical flexion

- Patient position: prone with arm resting comfortably at patient’s side
- put a pillow under the clavicular region for patient comfort and to promote a neutral cervical thoracic curve
Therapist position and hand placement
- stand on one side of the patient with your body facing toward his/her head
- adopt a two-thumb contact on the spinous process of the superior restricted segment of the three-joint complex
mobilizing force
- adopting the force through the thumbs, slide the superior vertebra in a cephalad anterior direction
- this glide is used to increase flexion of the cervical spine
Mobilization for cervical extension

- Patient position: prone with arm resting comfortably at patient’s side
- adopt a pillow for patient comfort and to promote a neutral thoracic curve
Therapist position and hand placement
- stand at the head of the patient with the body facing toward his/her feet
- adopt two thumb contact on the spinous process of the superior restricted segment of the restricted three-joint complex
mobilizing force
- adopting the force through the thumbs, slide the superior vertebra in a caudal posterior direction
- this glide is used to increase the extension of the cervical spine
Mobilization for cervical rotation

- Patient position: prone with arm resting comfortably at patient’s side
- adopt a pillow for patient comfort and to promote a neutral cervical thoracic curve
Therapist position and hand placement
- stand on one side of the patient with your body facing toward the patient’s head
- apply a two-thumb contact on the transverse process on the superior restricted vertebrae of the three-joint complex to create rotation toward the direction of restriction
mobilizing force
- adopting force through the thumbs, slide the superior vertebra in a cephalad anteromedial direction
- this glide is used to increase the rotation of the spine
Mobilization for cervical side bending
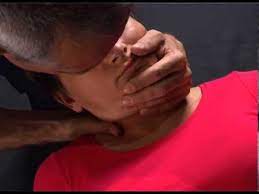
- patient position: supine
Therapist position and hand placement
- stand at the head of the patient with one hand supporting the head and the hand opposite side of the restriction
- the other hand in contact with the lateral aspect of the vertebra to be mobilized
- the medial side of the second MCP joint should be in contact with the edge of the facet and pillar to be mobilized
- rest of your hand relaxed position on the posterolateral portion of the patient’s neck
- passively place the patient’s head and neck into the flexion, contralateral rotation, and side bending to take up the slack until the segment is treated
mobilizing force
- adopting force through the metacarpal joint of the 2nd digits, slide or upglide the cervical facet in an anterior superior medial direction at a 45 degree
- this glide is used to increase the side bending of the cervical spine
- side bending increases the diameter of the ipsilateral foramen
Alternate technique
- patient position: supine
Therapist position and hand placement
- stand at the head of the patient with one hand supporting the head and the hand opposite side of the restriction
- the other hand in contact with the lateral aspect of the vertebra to be mobilized
- the medial side of the second MCP joint should be in contact with the edge of the facet and pillar to be mobilized
- rest of your hand relaxed position on the posterolateral portion of the patient’s neck
- passively place the patient’s head and neck into the extension, ipsilateral rotation, and side bending to take up the slack until the segment is treated
mobilizing force
- adopting force through the metacarpal joint of the 2nd digits, slide or downward glide the cervical facet in an anterior superior medial direction at a 45 degree
Craniocervicle flexion

- patient position: supine with hand placed comfortably on the affected side
Therapist position and hand placement and patient effort
- stand at the edge of the treatment table, support the occiput with one hand,
- place another hand across the forehead
- ask the patient to look upward gently
- apply resistance against the patient’s occiput
- creating a slight isometric contraction in the suboccipital muscles
- when the patient relaxes, take up the feeble by passively nodding the head through any new range
Alternate technique
- sit on a stool at the head of the patient with your forearm resting on the treatment table
- one hand stabilizes the c2 vertebra by grasping the transverse process between the proximal portion of the thumb and index finger
- the other hand supports the occiput bone,
- passively nod the patient’s head with the hand beneath the occiput to take up the feeble of the suboccipital muscles
- then told the patient to roll their eyes upward
- the patient conduct looking upward for 3 to 5 seconds and then relax
- after the patient relaxes, take up the feeble by passively nodding the head through any new range
- repeat the techniques 3 to 5 times or until desired the outcome is achieved
- only the motion in the middle of the occiput and c2 should occur
- the contraction is gentle and the technique is to hold and relax the rectus capitis posterior minor muscle
Craniocervical rotation

- patient position: supine with the hand placed comfortably at the side
Therapist position and hand placement
- stand at the head of the patient
- wrap hands around the side of the patient’s head with a finger under the occiput
- place the patient’s head in end-range of cervical flexion
- next, rotate his/her head in the direction of the restriction
- if restricted rotation to the left, place the head in end range left rotation
- once the patient is at the end range instruct the patient to look in the opposite direction
- while you resist the rotation movement with gentle pressure in opposition to the side of the hand after a 3 to 5-second hold
- the patient has to relax and move the head into greater rotation
- this causes gentle isometric contraction of the suboccipital muscles
Thoracic spine mobilization
Thoracic spine extension

- patient position: prone with arm resting comfortably on patient’s side
- put a pillow beneath the thoracic region for increased patient comfort and to promote a neutral cervical thoracic curve
Therapist position and hand placement
- stand on one side of the patient with your body facing toward the head of a patient
- place the distal phalanx of your 2nd and 3rd finger on the transverse process of the superior vertebral segment to be mobilized
- this technique also termed as V spread technique
- place the hypothenar eminence of your other hand on the top of the two-finger contact
mobilizing force
- apply an anterior glide, the contact points on the transverse process serve as a point of reference
- the other hand exerts a force through the hypothenar eminence pisiform in an anterior direction
Thoracic spine flexion

- patient position: prone with arm resting comfortably on patient’s side
- place a pillow beneath the thoracic region for increased patient comfort and to promote a neutral cervical thoracic curve
Therapist position and hand placement
- stand on one side of the patient with your body facing toward the head of a patient
- place the distal phalanx of your 2nd and 3rd finger on the transverse process of the inferior vertebral segment to be mobilized
- this technique also termed as V spread technique
- place the hypothenar eminence of your other hand on the top of the two-finger contact
mobilizing force
- apply an anterior glide, the contact points on the transverse process serve as a point of reference
- the other hand exerts a force through the hypothenar eminence pisiform in an anterior direction
- modify your force for pain modulation or to improve from
Thoracic spine rotation

- patient position: prone with arm resting comfortably on patient’s side
- place a pillow beneath the thoracic region for increased patient comfort and to promote a neutral cervical thoracic curve
Therapist position and hand placement
- use v spread contact
- place one finger on the superior transverse process and the second/other fingers on the contralateral inferior transverse process to be mobilized
- the finger placement accompanies the rule of the lower finger
Rule of the lower finger
- when applying v-spread contact on the contralateral transverse process for thoracic rotation mobilization, rotation of a segment occurs in the direction of the finger on the inferior transverse process
mobilizing force
- apply an anteriorly directed force against the transverse process with the contralateral hand pressing through the contact finger
pistol thrust

- patient position: supine with arm crossed
Therapist position and hand placement
- stand at the patient’s side facing toward his/her head
- roll the patient toward you and reach beyond the patient’s body
- contact the inferior vertebra of the 3 joint complexes to be mobilized by ” using pistol grip “
- one contact is achieved passively return the patient to the supine position
- to improve the rotation, use the rule of the lower finger
mobilizing force
- place your trunk directly over the segment to be mobilized
- A cephalad distraction force is initiated with the patient’s body weight at the segment to be mobilized
- apply high-velocity posterior force against the patient’s crossed arm toward the treatment table
Cross arm thrust

- patient position: prone with arm resting comfortably on patient’s side
- place a pillow beneath the thoracic region for increased patient comfort and to promote a neutral cervical thoracic curve
Therapist position and hand placement
- stand beside the patient
- cross your arm and place the pisiform bone hypothenar eminence of one hand on the left and one hand on the right transverse process of the segment to be mobilized
- modify transverse process contact to flexion, extension, or rotation by placing the pisiform bone on the superior and inferior or using a rule of the lower finger
mobilizing force
- An anterior force is applied simultaneously by the hypothenar eminence
Fall thrust

- patient position: standing with arms crossed
Therapist position and hand placement
- stand behind the patient
- wrap your arms around the patient
- place a mobilization folded towel at the desired spinal level to direct the force to a specific thoracic segment
- grasp the patient’s elbow alternatively
- if unable to grasp the elbow, interlock your fingers in front of the patient
mobilizing force
- bend backward on your heels while applying an extension force on the patient’s spine then quickly drop down so your feet are flat on the floor
Lumbar spine mobilization
lumbar spine extension

- patient position: prone lying, place a pillow beneath the abdominal region for patient comfort and to provide a neutral lumbo sacral curve
Therapist position and hand placement
- place your pisiform bone hypothenar eminence beyond the spinous process
- relax your hand on the patient’s back
Mobilizing force
- thrust with your hypothenar eminence in an anterior direction
- align your trunk directly above the segment, so the force is directed downward and not an angle
Lumbar spine rotation

- patient position: prone, place a pillow beneath the abdominal region for patient comfort and to provide a neutral lumbo sacral curve
Therapist position and hand placement
- place your pisiform hypothenar eminence beyond the transverse process on the side opposite of the direction of motion you wish to promote
- if wanting to encourage left rotation, place your hypothenar eminence on the right transverse process
- relax leisurely with your hand on the patient’s back
mobilizing force
- give thrust with your hypothenar eminence in an anterior and medial direction
lumbar spine side bending

- patient position: side-lying with the restricted side downwards
- position the patient nearer to the margin of the bed as possible
- flexes the hip and knees to 90 degree
Therapist position and hand placement
- stand facing the patient
- place the tip of your caudal hand on the superior spinous process to monitor the motion
- passively rotate the patient’s trunk backward to “take up the feeble” until just before feeling the vertebral segment move
- now place the tip of the finger of your cephalad hand on the superior spinous process to observe the motion
- flex both hips of the patient until just before you feel the vertebral segment move
- the patient’s leg can be supported either on the plinth or with your thigh
mobilizing force
- lift the patient’s leg into the hip rotation, causing the lumbar spine to side bend
HVT lumbar roll

- patient position: side lying with restricted side upward,
- position the patient nearer to the margin of the bed as possible
- flex the hip and knee 90 degrees
- provide a pillow for the patient to hold the position and act as a physical barrier
Therapist position and hand placement
- stand facing the patient
- place the fingertip of your cephalad hand on the inferior spinous process to monitor the motion
- move the patient’s top side of the leg into hip flexion until just before you feel the inferior vertebral segment move
- maintain the hip flexion by stabilizing the leg between the therapist’s body or/and the treatment table
- move the cephalad hand to the superior spinous process to observe the motion
- passively rotate the patient’s trunk backward to “take up the feeble” until just before feeling the superior vertebral segment move
- rest the forearm on the patient’s body part
- the therapist’s hand should be directly over the segment to be mobilized
Mobilizing force
- therapist applying the downward rotational thrust toward the treatment table with the cephalad forearm and hand while applying a rotational force through the caudal forearm by pulling the patient’s lower trunk toward your body
Precaution for spine mobilization
- if a mobilization procedure causes a change in sensation or an increased pain to radiate down an extremity or/and if a patient reports a feeling of dizziness or lightheadedness or does not perform additional mobilizations
- use extreme precaution if the patient reports either a current history of corticosteroid use or excessive pain
Joint effusion
- the joint effusion occurs due to trauma or disease
- rapid swelling of the spine generally designate
- bleeding in the spine and may happen with diseases aspiration of the blood to lessen the necrotizing effect on an articular cartilage
- slow swelling for more than 4 hours generally designates serious spine effusion or edema on the spine due to mild trauma irritation or disease
- do not stretch the inflamed or injured spine with mobilization because the joint capsule is already stretched by being expanded to accommodate the extra fluid
- the limitation of motion is, in addition, to add extra fluid and muscle response to pain, not from shortened fibers
- gentle oscillating motion that does not stress the joint capsule may help to block the transmission of a pain stimulus so it is not perceived and may help to initiate fluid flow while maintaining available cooperative movement
- if a patient’s response to a slight method is increased pain or joint irritability
- the method was exercised too strenuously or should not be done with the current state of pathology
Inflamation
- whenever inflamation is present, stretching raises pain and muscle guarding conclusion in greater tissue damage
- gentle distraction movements may temporarily decelerate the pain response
hypermobility
- the joint of the patient with probable necrosis of ligaments or/and joint capsules should not be mobilized with stretching methods
FAQS
- When do we use joint mobilization for the spine?
The main goal of spine mobilization is to regain the normal joint play movement that might have been compromised by damage or injury. Normal movement of the affected spine will be recouped faster if it is compromised early in the treatment program. Also, mobilization is advantageous in cases when the range of motion is not present in the spine
- Why is early mobilization necessary after an injury?
In patients with acute spine injuries, early mobilization decelerates pain and swelling and upgrades functional outcomes correlated with cast immobilization
- How long do you do joint mobilization for the spine?
Typical treatment of a spine joint may add a series of 3 to 6 mobilizations kept on up to 30 seconds, with one to three oscillations or/and glide per second
- How does joint mobilization reduce pain?
grade 2:large amplitude rhythmic oscillation initiate within range, not achieve the limit of movement, apply the glide for 2 or 3 seconds for 1 to 2 minutes
that goes center way into the joint range of movement, attending any part of the range and still not reaching the end range. This method can be given to treat stiffness by accelerating the range of motion and pain - is mobilization suitable for a laminectomy?
During the acute phase of recovery, physiotherapy will target early mobilization getting up and walking, and slight exercise. Early mobility will diminish the risk of secondary complications such as blood clots, increased pain, and infection.