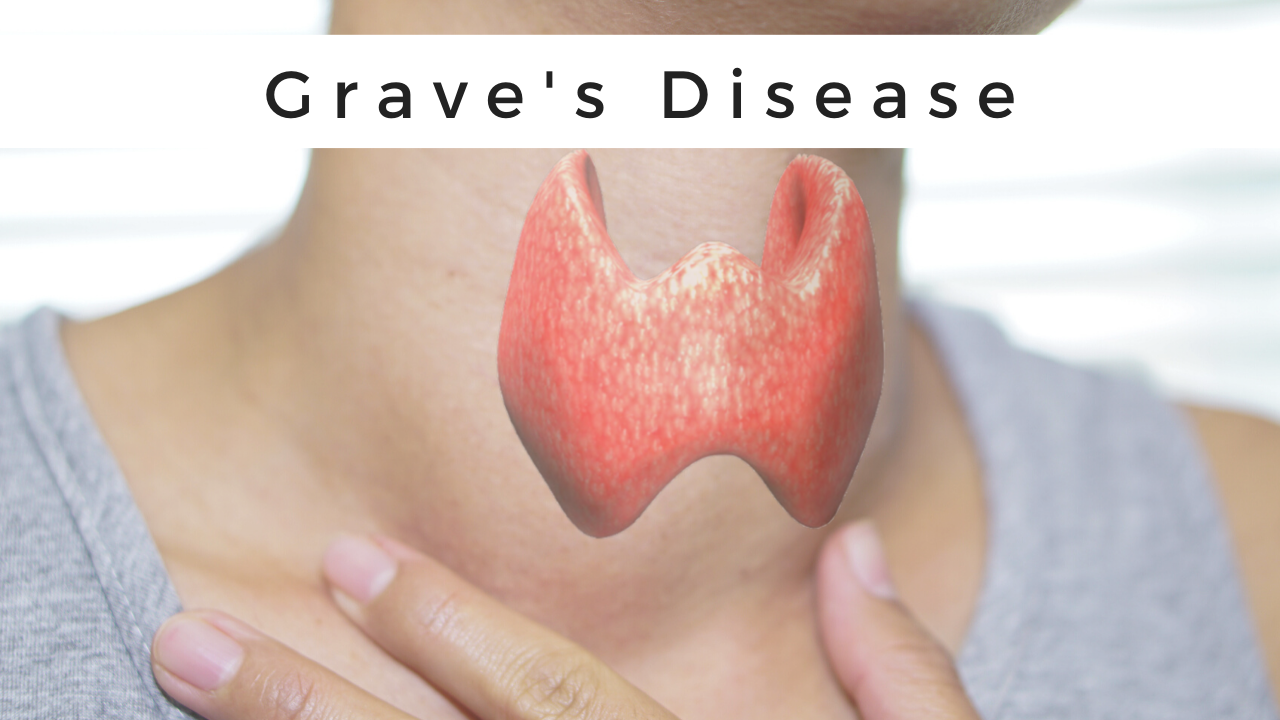
Grave’s Disease
Table of Contents
What is Grave’s Disease?
Grave’s disease is an immune system disorder(autoimmune disorder). In Grave’s disease, there is an overproduction of thyroid hormones that leads to hyperthyroidism. The thyroid present in the body is a small, butterfly-shaped gland in the front of the neck. Thyroid hormones regulate the way the body uses energy, so they affect nearly every organ in the body, even the way the heart beats. Although multiple disorders may result in hyperthyroidism, Graves’ disease is a common cause of hyperthyroidism.
In a person with Grave’s disease, the immune system makes antibodies that provoke the thyroid to make more thyroid hormone than the body needs.
The thyroid’s main job is to regulate the speed of metabolism (metabolic rate), which is how your body transforms the food you consume into energy by releasing certain hormones.
Grave’s disease affects everyone, more common among women and people younger than 40.
Causes of Grave’s Disease:
It is unknown what causes autoimmune diseases like Grave’s disease. There is something that triggers the immune system to overproduce an antibody called thyroid-stimulating immunoglobulin (TSI). TSI attaches to healthy thyroid cells, causing your thyroid to overproduce thyroid hormones.TSI acts like a thyroid-stimulating hormone (TSH), a hormone made in your pituitary gland that tells your thyroid how much thyroid hormone to make. TSI provokes the thyroid to make too much thyroid hormone.
The stimulus of the attack may be a combination of having a genetic predisposition and environmental factors, such as:
- Stress.
- Virus/infection.
- Pregnancy.
Signs and Symptoms of Grave’s Disease:
The signs and symptoms of Graves’ disease all result from the direct and indirect effects of hyperthyroidism. It often causes symptoms of hyperthyroidism. Graves’ disease may also affect the eyes and skin. Symptoms can occur and go over time.
Symptoms of hyperthyroidism can alter from person to person and may include:
- Weight loss, despite an increased appetite
- Rapid or irregular heartbeat(Palpitation)
- Nervousness, irritability, trouble sleeping, fatigue
- Shaky hands, Due to muscle weakness
- Sweating or trouble to tolerate heat
- Frequent bowel movements
- An enlarged thyroid gland called a goiter
- Diarrhea and/or more frequent bowel movements.
- Thin, warm, and moist skin.
- Intolerance to heat and excessive sweating.
- Difficulty sleeping, such as insomnia.
- Enlarged thyroid gland (goiter).
- Loss of hair and change in hair texture (brittle).
- Menstrual changes.
- Muscle weakness.
- If a person is experiencing any of these symptoms, see to doctor
Graves’ disease can also induce eye disease symptoms, including:
- Gritty, irritated eyes.
- Swelling of the tissues around the person’s eyes (puffy eyes).
- Bulging eyes.
- Light sensitivity.
- Pressure or pain in your eyes.
- Blurred or double vision
This problem in the eye is named Graves’ ophthalmopathy or orbitopathy or thyroid eye disease. Few people with Graves’ disease develop this condition.
Infrequently, people with Graves’ disease may produce a lumpy, reddish thickening of the skin on their shin known as pretibial myxedema (called Graves’ dermopathy)
It is generally painless and mild, but it can be painful for some people.
Risk Factors:
Although any person can develop Graves’ disease, there are many factors that can increase the risk of the disease, including:
- Family history: Because a family history of Graves’ disease is a known risk factor, there is probably a gene or genes that can make a person more susceptible to the disorder.
- Sex: Women are much more susceptible to developing Graves’ disease than men.
- Age: Grave’s disease usually develops in people before age 40 in younger age.
- Other autoimmune disorders: People with other immune disorders, such as type 1 diabetes or rheumatoid arthritis, have an increased risk.
- Emotional or physical stress: Stressful work or life events or illness may act as a trigger for the onset of Graves’ disease among people who have genes that increase their risk.
- Pregnancy: Pregnancy or recent childbirth may increase the risk of the disease, particularly among women who have genes that increase their risk.
- Smoking: Cigarette smoking is unhealthy, which can affect the immune system, and increases the risk of Graves’ disease. Smokers who have Graves’ disease may also be at increased risk of developing Graves’ ophthalmopathy.
Complications of Grave’s Disease:
If it is untreated, Graves’ disease can cause serious health problems, including:
- A rapid and irregular heartbeat can lead to blood clots, stroke, heart failure, and other heart-related problems
- Thinning bones
- Osteoporosis NIH external link
- Muscle problems
- Difficulty in the menstrual cycle, pregnancy, and fertility
- Eye discomfort and changes in vision
Pregnancy issues: Possible complications of Graves’ disease during pregnancy includes are given below:
- Miscarriage
- Preterm birth
- Fetal thyroid dysfunction
- Poor fetal growth
- Maternal heart failure
Preeclampsia: Preeclampsia is a maternal condition in which there is high blood pressure and other serious signs and symptoms.
Heart disorders: If it is left untreated, Graves’ disease can lead to heart rhythm disorders, changes in the structure and function of the muscles of the heart, and the heart’s not able to pump sufficient blood to the body termed heart failure.
Thyroid storm. A rare but life-threatening complication of Graves’ disease is a thyroid storm, also comprehended as accelerated hyperthyroidism or thyrotoxic crisis. It is more occur when severe hyperthyroidism is untreated or treated inadequately.
The sudden and intense raise in thyroid hormones can produce many effects on the body, including fever, sweating, vomiting, diarrhea, delirium, severe weakness, seizures, irregular heartbeat, yellow skin and eyes (jaundice), severe low blood pressure, and coma. Thyroid storm requires immediate emergency care.
Brittle bones: If hyperthyroidism is not treated, also can lead to weak, brittle bones (osteoporosis). The strength of the bones depends on the amount of calcium and other minerals the bone contains. Too much thyroid hormone interferes with your body’s ability to incorporate calcium into the bones.
Eye complications: A small percentage of all patients with the grave disease will develop a condition called thyroid eye disease in which the eye muscles and tissues become swollen. This can lead to exophthalmos in which the eyeballs protrude from their sockets, which is considered a hallmark of Graves’ disease, even though it’s rare. But having this eye complication doesn’t have anything to do with how severe Graves’ disease is. In fact, it is not clear whether such eye complications stem from Graves’ disease itself or from a totally other cause, but it is a closely linked disorder. If a person has developed thyroid eye disease, the eyes may ache and feel dry and irritated. Protruding eyeballs are prone to excessive tearing or water and redness, partly because the eyelids can’t protect them as well.
In severe cases of exophthalmos, which are rare, swollen eye muscles can put enormous pressure on the optic nerve, possibly leading to partial blindness. Eye muscles weakened by long periods of inflammation can lose their ability to control the movement of the eye, resulting in double vision.
Skin complications: Some with Graves may develop a rare skin condition known as pretibial myxedema or Graves dermopathy, which is a lumpy reddish thickening of the skin on the shins.
Diagnosis:
The doctor may advise laboratory tests if they might have Graves’ disease. If anyone in the family has had Graves’ disease, the doctor may be able to narrow down the diagnosis based on your medical history and a physical examination.
Doctors need to confirm the diagnosis through thyroid blood tests. A doctor who specializes in diseases related to hormones, known as an endocrinologist, may handle tests and diagnoses.
Your doctor may also advise some of the following tests:
- Blood test: These tests can measure the levels of the thyroid hormones in the body and also check for TSI.
- Thyroid ultrasound
- Radioactive iodine uptake test: This test measures the amount of iodine the thyroid gland is taking up from the bloodstream to make thyroid hormones. If the thyroid is taking up large amounts of iodine, a person may have Graves’ disease.
- Thyroid scan: This test, often done together with the radioactive iodine uptake test, reveals how and where iodine is distributed in your thyroid. In Graves’ disease, iodine shows up throughout the gland. With other reasons for hyperthyroidism such as nodules that are small lumps in the gland—the iodine shows up in a different pattern.
- Thyroid-stimulating hormone test
Thyroid-stimulating immunoglobulin test - Doppler blood flow measurement NIH external link: This test, is also known as Doppler ultrasound. This test there is use sound waves to detect increased blood flow in the thyroid due to Graves’ disease. A doctor may order this test if radioactive iodine uptake is not a good option for a person, such as during pregnancy or breastfeeding.
The integrated results of these may help your doctor learn if you have Graves’ disease or another type of thyroid disorder.
Treatment of Grave’s Disease:
The treatment goals for Grave’s disease are to stop the production of thyroid hormones and to block the impact of the hormones on the body. Some treatments include:
- Radioactive iodine therapy:
With this therapy, the patient takes radioactive iodine (radioiodine) by mouth. Because the thyroid gland needs iodine to produce hormones, the thyroid takes the radioiodine into the thyroid cells and the radiation destroys the overactive thyroid cells over time. This causes the thyroid gland to shrink, and symptoms lessen gradually, usually over several weeks to several months.
Radioiodine therapy may increase the risk of new or worsened symptoms of Grave’s ophthalmopathy. This side effect is usually mild and temporary, but the therapy may not be recommended if the person already has moderate to severe eye problems.
Other side impacts may include tenderness in the neck area and a temporary boost in thyroid hormones. Radioiodine therapy is not used for treating pregnant women or women who are breastfeeding.
Because this treatment causes thyroid activity to decrease, you’ll likely need treatment later to supply the body with normal amounts of thyroid hormones.
- Anti-thyroid medications:
Anti-thyroid medications interrupt the thyroid’s use of iodine to make hormones. These prescription medications involve propylthiouracil and methimazole (Tapazole).
Because the chance of liver disease is more common with propylthiouracil, methimazole is considered the first choice when doctors prescribe medication. However, propylthiouracil is preferred as an anti-thyroid drug during the first trimester of pregnancy, as methimazole has a slight chance of birth defects. Pregnant women will typically go back to taking methimazole after the first trimester.
When these two drugs are used alone without the use of other treatments, a relapse of hyperthyroidism may occur at a later time. Taking drugs for longer than a year may result in adequate long-term results. Anti-thyroid drugs may also be used before or after radioiodine therapy as a supplemental medicine.
Side effects of both drugs include rash, joint pain, liver failure, or a decrease in disease-fighting white blood cells(WBC).
- Beta-blockers:
These medications do not inhibit the production of thyroid hormones, but they do block the influence of hormones on the body. They may provide relatively rapid relief of irregular heartbeats, tremors, anxiety or irritability, heat intolerance, sweating, diarrhea, and muscle weakness.
Beta blockers include:
- Propranolol (Inderal, InnoPran XL)
- Atenolol (Tenormin)
- Metoprolol (Lopressor, Toprol-XL)
- Nadolol (Corgard)
- Beta-blockers are not often prescribed for people with asthma because the drugs may trigger an asthma attack. These drugs may also confuse the management of diabetes.
- Surgery:
Surgery to remove part or most of the thyroid gland is used small often to treat hyperthyroidism. Sometimes doctors use the option of surgery to treat people with large goiters or pregnant women who cannot take antithyroid medicines to treat hyperthyroid conditions.
A close-up of a woman’s neck shows a scar from thyroid surgery.
In some cases, doctors use surgery to remove a part or most of the thyroid gland.
Pros
When part of the thyroid is removed, the thyroid hormone levels may return to normal.
Cons
Thyroid surgery needs general anesthesia, which can lead to thyroid storm a condition in which a sudden, severe worsening of symptoms if antithyroid medicines are not taken before surgery to relieve this condition.
When part of the thyroid is removed, a person may develop hypothyroidism after surgery and need to take thyroid hormone medicine. If the whole thyroid is removed, the patient will need to take thyroid hormone medicine for life. After surgery, the doctor will continue to check the thyroid hormone levels and will adjust the thyroid medicine dosage as needed.
Risks of this surgery include :
Potential damage to the nerve that controls the vocal cords and the tiny glands located adjacent to the thyroid gland (parathyroid glands).
Parathyroid glands make a hormone that controls the level of calcium in the blood.
Complications are rare under the care of a surgeon experienced in the surgery of the thyroid. You will need to take thyroid medication for your whole life after this surgery.
Summary:
Without treatment, Grave’s disease can contribute to cardiac problems, weak and brittle bones, and pregnancy complications. Prompt treatment, however, can improve the symptoms and help lower the chances of health complications.
A doctor or healthcare specialist can offer more information about the treatment options, plus their benefits and risks.
What does Graves disease do to a person?
In Grave’s disease, the immune system attacks the thyroid gland, provoking it to make more thyroid hormones than the body needs. Due to this increase in the production of thyroid hormone, many of the body’s functions speed up. The thyroid gland is a small gland located in the neck that produces thyroid hormones.
Can Graves disease be cured?
A permanent cure for Graves’ hyperthyroidism is possible. The cure rate would be even lower if the cure also considers the absence of TSH receptor antibodies.
Is Graves disease a fatal disease?
Grave’s disease is infrequently life-threatening. However, without treating the condition, it can lead to heart problems and weak and brittle bones. Grave’s disease is termed an autoimmune disorder. That’s because, with the disease, the immune system attacks the thyroid — a small, butterfly-shaped gland at the base of the neck.
What are the signs and symptoms associated with Graves disease?
The symptoms may contain anxiety, irritability, a racing heart, feeling hot, sweating, and tremor. A person may have bulging eyes and an enlarged thyroid gland (goiter) in the neck. A doctor can diagnose Graves’ disease with blood tests and treat a person with medications and sometimes surgery.
What is the best treatment for Graves disease?
These prescription medications include propylthiouracil and methimazole (Tapazole). Because the risk of liver disease is more common with propylthiouracil, methimazole is regarded as the first choice when doctors prescribe medication.