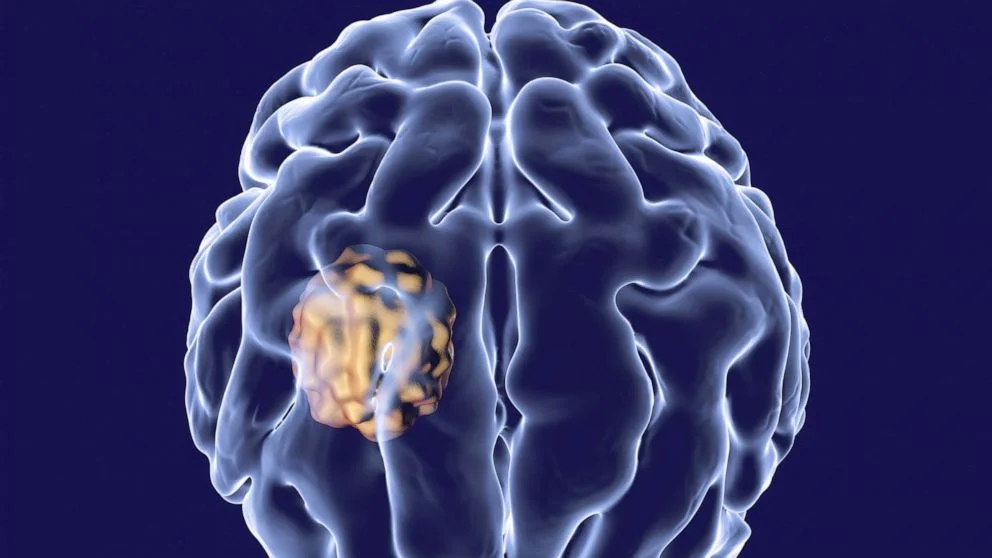
Brain Abscess
Table of Contents
What is Brain Abscess?
A Brain abscess is a swelling of the brain that is filled with pus. It typically happens after an infection or serious head injury when bacteria or fungi get into the brain tissue.
Although there is very little chance of getting a brain abscess in England, it is a serious condition that needs to be identified and treated right away.
Symptoms of a brain abscess
Brain abscess symptoms can appear suddenly or gradually and can include:
- a headache (69–70 percent of cases)
- a fever (45–53 percent)
- seizures (25–35 percent)
- nausea and vomiting (40 percent)
The first indication of an abscess may be a seizure. As the pressure inside the brain increases, nausea and vomiting frequently happen.
Pain may start slowly or suddenly and typically begins on the side of the abscess.
In 65% of cases, changes in mental status occur, and they can result in:
- confusion
- drowsiness and lethargy
- irritability
- poor mental focus
- poor responsiveness
- slow thought processes
- coma (possibly)
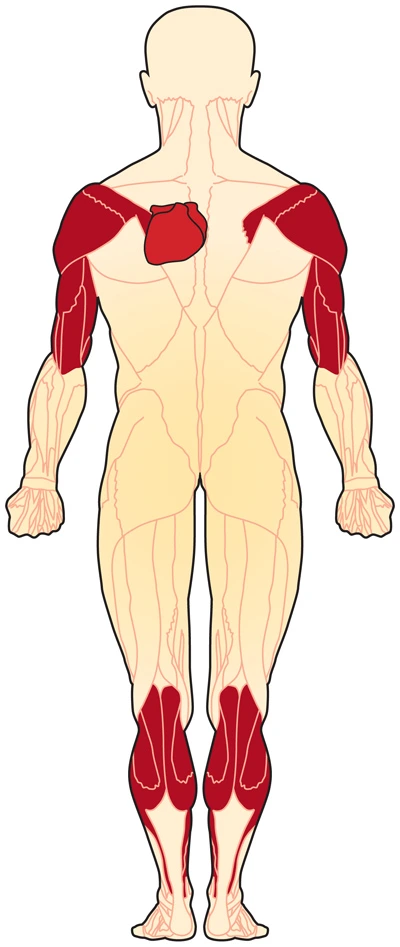
Between 50 and 65 percent of those with brain abscesses experience neurological problems. These problems frequently develop days or weeks after a headache and can include:
- muscle weakness
- One side of the body is weak or paralyzed
- Speech problems, such as slurred speech
- Poor coordination
Other symptoms may include:
A stiff neck, back, or shoulders
Blurred, double, or graying vision
Infection, damage to brain tissue, and pressure on the brain as the abscess expands to take up more space all contribute to the symptoms of a brain abscess.
The abscess may have ruptured if the headache suddenly gets worse.
It is true that symptoms can last up to two weeks in two-thirds of cases. Doctors typically identify the problem eight days after the onset of symptoms.
Causes of a brain abscess
The most common cause of a brain abscess is a bacterial or fungal infection in the brain. An abscess may also result from parasites.
Inflammation and swelling take place when bacteria, fungi, or parasites infect a portion of the brain. In these situations, the abscess will contain pathogenic organisms, active and dead white blood cells, and infected brain cells.
A wall or membrane forms around the abscess as the cells gather. Preventing the infection from spreading to healthy tissue, this aids in its isolation.
An expanding abscess increases the pressure on the surrounding brain tissue.
The skull cannot expand because it is rigid. As a result of the abscess’s pressure, blood vessels may become blocked and stop supplying the brain with oxygen, which may cause delicate brain tissue to be damaged or even destroyed.
Three main factors can lead to a brain abscess. Which are:
- A dental abscess, sinus infection, or ear infection in another part of the skull has the potential to spread to the brain.
- an infection in another area of the body, such as pneumonia that spreads through the blood into the brain.
- trauma that cracks open the skull, allowing bacteria or fungi to enter the brain, such as a head injury
How infection enters the brain
For a variety of reasons, brain infections are not very common.
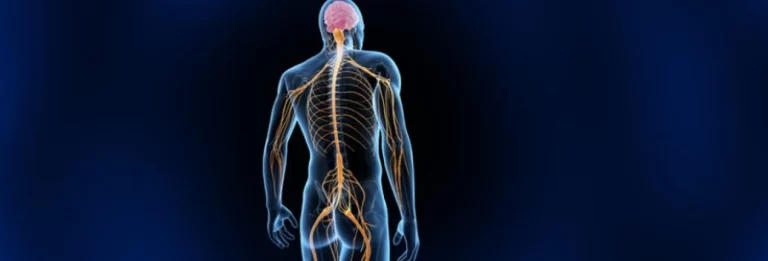
The blood-brain barrier, a defense system made up of blood vessels and cells, is one cause. It allows some substances to pass through while blocking others from the blood that travels to the brain.
An infection may occasionally cross the blood-brain barrier. This may occur when inflammation weakens the barrier and creates openings.
It may:
Spread from a nearby site, like the ear, through the blood from an infection in another area of the body.
result from surgery or traumatic injury
Infection coming from another body part.
If an infection develops elsewhere in the body, the infectious agents can cross the blood-brain barrier without being stopped by it and then enter the bloodstream to infect the brain.
Pathogens that have traveled to an abscess from another part of the body account for 9 to 43% of them.
A lesion elsewhere in the body often serves as the origin of bacterial brain abscesses. Finding that initial infection is essential to prevent future infections from occurring.
A bloodborne infection increases the risk of a brain abscess in people with compromised immune systems.
A person may have a compromised immune system if they:
AIDS and HIV
Are children younger than six months old receiving chemotherapy, taking long-term steroid medication, receiving organ transplants, and taking immunosuppressant medications to prevent organ rejection?
The following infections are the most frequently associated with brain abscesses:
Pneumonia, bronchiectasis, endocarditis, a heart valve infection, and other lung diseases and conditions
Abdominal infections like peritonitis, an inflammation of the abdomen’s and pelvis’ inner walls
Bladder inflammation is known as cystitis, along with other pelvic infections
Direct contagion
A nearby area can become infected, and this is the True Source of 14–58% of brain abscesses.
The brain may become infected if an infection begins inside the skull, such as in the nose or ear.
The infections mentioned below can lead to brain abscess:
Middle ear infection, or otitis media
An infection of the bone behind the ear known as sinusitis mastoiditis
The site and nature of the initial infection may affect where the abscess develops.
Direct trauma
Trauma, such as from neurological surgery or a penetrating brain injury, can lead to a brain abscess.
An abscess may develop as a result of:
A concussion results in a compound skull fracture, which pushes bone fragments into the brain.
If a foreign object, such as a bullet, is present and not removed
An uncommon surgical complication
How is a Brain abscess diagnosed?
Many of these symptoms resemble other illnesses or health issues very closely. If you start to experience any of the symptoms, consult your doctor right away. A neurological examination is probably necessary. This help to find any elevated pressure in the brain that could result due to swelling. Brain abscesses can also be identified using CT and MRI scans.
Your doctor might occasionally need to perform a spinal tap, also known as a lumbar puncture. To test for any issues other than an infection, a small amount of cerebral spinal fluid must be removed. If significant brain swelling is suspected, a lumbar puncture won’t be done because it might make the pressure inside the head temporarily worse. This reduces the possibility of a brain hematoma or a brain blood vessel rupture.
They will need to know if the person:
has recently been infected
has a compromised immunity
It may take some time to definitively determine the diagnosis because symptoms can resemble those of other diseases and conditions. If the doctor can pinpoint precisely when symptoms began and how they developed, the diagnosis will be simpler.
Tests might consist of Trusted Sources:
A blood test to look for an infection-related increase in white blood cells
MRI or CT scans, in which one or more spots representing an abscess will appear
A type of needle biopsy called a CT-guided aspiration involves collecting pus for analysis.
Because CT and MRI scans are being used more frequently for detection, the number of fatalities from brain abscesses has decreased in recent years.
What’s the Treatment for a brain abscess?
An abscess in the brain is a serious medical condition. Brain damage that is permanent can result from pressure brought on by brain swelling.
If your abscess is less than 2.5 centimeters in diameter or is deeply embedded in your brain, antibiotics will likely be used to treat it. Any underlying infections that may have contributed to the brain abscess will also be treated with antibiotic drugs. The most frequently prescribed antibiotics are those with a broad spectrum of activity that kills numerous bacteria. More than one kind of antibiotic may be required.
Surgery is frequently the next course of action if antibiotics don’t reduce an abscess. Additionally, it might be the preferred course of action for abscesses wider than 2.5 centimeters. An abscess is typically surgically removed by opening the skull and draining the abscess. The extracted fluid is typically sent to a lab to identify the infection’s origin. Your doctor can choose the best antibiotics by understanding the infection’s underlying cause. If antibiotics are ineffective, surgery might also be required in order to identify the organism causing the abscess and determine the best course of action.
In the worst conditions, when the abscess leads to a risky increase in pressure in the brain, immediate surgery is required. In the following situations, your doctor might prefer surgery as the best available option:
You run the risk of your brain abscess rupturing inside your skull.
Your brain abscess contains gases that bacteria occasionally produce.
Surgery and medication are typically used as treatment options.
A doctor will typically prescribe broad-spectrum antibiotics right away if they suspect a brain abscess because an abscess can be fatal.
If tests reveal a viral infection rather than a bacterial infection, the doctor will adjust the course of treatment.
The following factors will affect how well the therapy works:
The abscess’s size.
The number of abscesses and the origin of the abscess
The overall health of the individual
Only intravenous antibiotic, antifungal, or antiviral medication will likely be given to the patient if the abscess is smaller than 1 inch in diameter. To decide which antibiotics will work best, a physician might first need to drain a smaller abscess.
A doctor will need to aspirate, drain, or cut out an abscess if it is larger than 1 inch in diameter.
Cutting out multiple abscesses might be too dangerous. Aspiration will be advised by the surgeon.
Additionally, the patient will require medical attention for any primary infections, such as those in the nose, stomach, or lungs.
Surgery
Surgery might be required if:
The abscess does not respond to treatment, and the pressure in the brain continues to increase.
Since the abscess contains gas, there is a chance that it could rupture.
A craniotomy is a procedure in which a skull incision is made by the surgeon.
The following are the steps:
A small portion of the scalp will be shaved by the surgeon.
To access the brain, a small piece of bone is removed.
With the help of a CT scan, they may be able to either drain the pus or remove the abscess.
They stitch the skin together and replace the bone.
Medication
If there is an increase in intracranial pressure and a possibility of complications, such as meningitis, a brief course of high-dosage corticosteroids may be beneficial.
However, doctors don’t usually recommend trusted Source corticosteroids.
Anticonvulsants can be prescribed by a doctor to treat seizures, and they may be necessary for up to five years for someone who has had a brain abscess.
Can a brain abscess be prevented?
An abscess in the brain is a serious medical condition. Preventive action is crucial. By keeping an eye out for any conditions that might result in a brain abscess, you can reduce your risk. At the first indication of a brain abscess, contact your doctor.
Before having any dental or urological procedures, discuss with your doctor if you have any type of heart disorder. You may be given antibiotics to take before these procedures by your doctor. Your chance of developing an infection that could affect your brain will go down as a result.
According to studies, 5-32 percent of brain abscesses result in death.
Depending on the degree of damage, there might be long-term effects among those who live. Long-term neurological issues brought on by a brain abscess can include seizures, personality changes, and problems with physical function.
It’s critical to be aware of the potential signs of a brain abscess and to seek medical attention right away if they materialize. A patient’s chances of survival increase with the likelihood that treatment will be effective as soon as possible.
The characteristics of the abscess also influence the prognosis. Treatment is more challenging for abscesses with multiple lesions and those deep inside the brain.
Since an abscess may return, the doctor will keep an eye on the patient as they recover. This might entail having a minimum of two weeks’ worth of weekly CT scans. Additionally, an abscess may come back after months or even years, making long-term monitoring crucial.