THE VOJTA APPROACH: NEURODEVELOPMENTAL TREATMENT IN SPECIAL CHILDREN
THE VOJTA APPROACH
Table of Contents
INTRODUCTION :-
- Vojta-Therapy is a dynamic neuromuscular treatment method based on the developmental kinesiology and principles of reflex locomotion. This method is supposed to treat patients with disorders of central nervous system and musculoskeletal system. It was developed by child neurologist Prof. Vaclav Vojta in the 20th century and now used predominantly in Europe.
INDICATION
- According to Vojta, this therapy can be applied to the patients of any age group and can be used as standard therapy in physiotherapy for almost every movement disturbance and for numerous illnesses:
> Severe and medium central coordination disorders
> Light but asymmetrical central coordination disorders
> Cerebral palsy
> Muscular and neurogen torticolis
> Peripheral Paralyses (child and adult)
> Spina bifida
> Congenital myopathies – congenital deformities (athrogryposis, club foot etc…)
> Morbus-Down syndrome and other syndromes – motor delays
> Various postural disorders (scoliosis, cyphosis)
> Hip dysplasies
> Adult hemiplegy (unexhaustive list)…
> Migraine
> Respiratory Distress Syndrom ( RDS)
CONTRAINDICATION
- Vojta Therapy should not be used in:
> acute feverish or inflammatory conditions
> vaccinations with live vaccines following doctor’s orders (as a rule 10 days after vaccination)
> existing pregnancy in patients
> certain illness, as e.g. imperfect osteogenesis, heart disease etc.
- In all illnesses that impact on patient’s general condition, Vojta Therapy can be carried out for shorter sessions, depending on the tolerance level of the patient, but does not have to be ruled out.
WHAT IS REFLEX LOCOMOTION?
- The reflex locomotion is the fundamental therapeutic process of Vojta therapy.
- The term “reflex” locomotion implies that the complete motor pattern does not appear spontaneously but only under peripheral stimulations, applied on different points of the body. However the provoked pattern concerns the whole body, including the four limbs.
- V. Vojta described several automatic global patterns of which kinesiological characteristic components have been precisely defined. In the different publications the provoked pattern in the prone position has been called “reflex creeping”; the pattern obtained in the supine position has been called “reflex rolling”.
- These neuromotorial complexe activities have been meticulously studied for many years among from 2 – 3 years up until 15 years old CP children. This observation has allowed to deduce that some spontaneous postures that can be seen among the oldest CP children are already apparent at pathological infants, and even at pathological new-borns. That means that postural automatisms generated by the central nervous system (CNS) of a CP child have something common with these of a new-born or of a much younger child.
- The complex muscular games observable during the reflex locomotion (therapy) at CP children can be obtained instantaneously with a valid new-born. It can be deduced that the muscular action provoked at this valid new-born, and the other one, artificially provoked by reflex means at a CP child, correspond to a common neurogenic process (functional pattern). A CP child go on exploiting motor patterns, coming from its new-born period, and whose progressive transformation could not normally occure because of the lesion of the CNS. Everything happens as if the motor development was blocked.
REFLEX LOCOMOTION OR PHASES OF VOJTA APPROACH
- The Vojta method can be divided into 2 main phases:
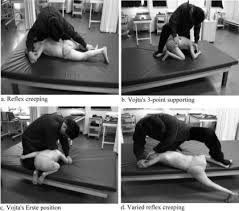
> Reflex creeping (lying ?at with the chest down and back up)
> Reflex rolling (lying ?at with the chest up and back down)
1. Reflex Creeping:
- Reflex creeping is a movement sequence that includes the most fundamental components of locomotion:
1. Specific postural control
2. Up-righting or extension against gravity and
3. Goal-directed stepping movements of the arms and legs.
- Thus, reflex creeping encompasses the basic patterns of human locomotion. The main position is prone lying with the head resting on the bed rotated to one side.
- The above illustration shows the starting position for reflex creeping and its stimulation zones. These “stimulus points”, in conjunction with the joint angles of the extremities and of the head, start the motor sequence for the creeping sequence with its muscular activities.
- In new-born babies, reflex creeping can be fully activated from one zone; in older children and in adults, a combination of several pressure points is necessary.
- Movement predominantly ensues in the so-called cross pattern, in which the right leg and the left arm, or vice versa, move simultaneously. A leg and its contralateral arm support the body and move the trunk forwards.
- In therapy, the therapist sets up an adequate resistance against the patient’s incipient head rotation. This strengthens the activation of the overall body musculature, thus creating the pre-conditions for uprighting.


Reflex Creeping & Vojta Tech.
# The goals of reflex creeping are notably:
- Activation of the muscular support and uprighting mechanisms necessary for supporting and grasping, rising and walking, as well as stepping movements of the arms and legs
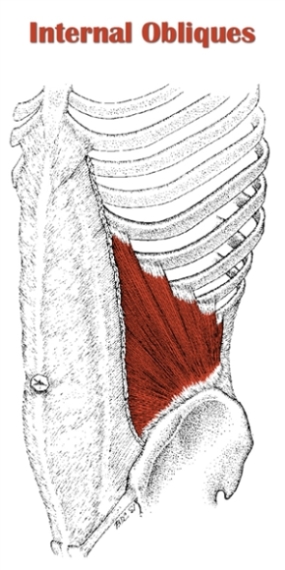
- Activation of the respiratory, abdominal, and pelvic floor musculature, as well as the sphincters of the bladder and bowel
- Swallowing (important for mastication)
- Eye movements
2. Reflex Rolling:
- Reflex rolling transitions from supine to side lying and leads to crawling. In a healthy new-born baby, part of this movement sequence is spontaneous, and can be observed in approximately the sixth month of life, with a further part of the sequence observable in the eighth/ninth month. With Vojta therapy, it can even be obtained in new-born babies.
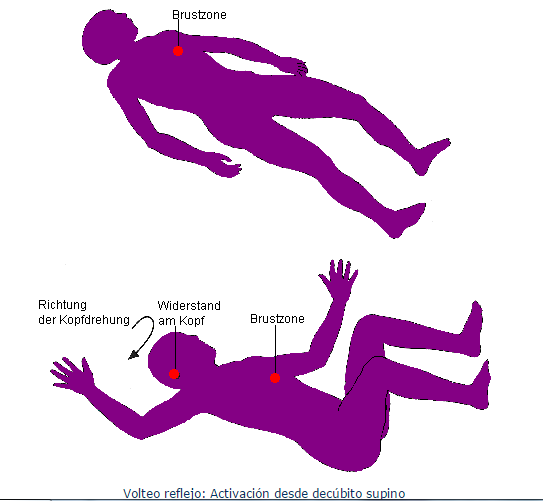
- Therapeutically, reflex rolling is used in different phases of supine and side-lying:
– Phase 1:
- The first phase starts with supine lying, arms and legs extended. Through stimulation of the breast zone in the intercostal space (7th/8th ribs) beneath the nipple on the mammillary line, rotation to the side is achieved. Rotation of the head is resisted by the therapist/practitioner.
- The fundamental reactions are:
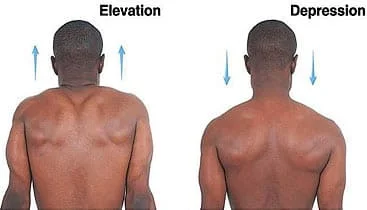
> Extension of the spine
> Flexion of the legs in hip, knee, and ankle joints
> Maintenance of the legs in this position against gravity, outside the support base of the back
> Preparation of the arms for the following support function
> Lateral eye movements
> Initiation of swallowing
> Increase in the depth of breathing
> Coordinated, differentiated activation of the abdominal muscles
– Phase 2:
The second phase of reflex rolling has its onset in side lying. It encompasses movement sequences that are also present in spontaneous rolling, crawling and lateral movement. The underlying upper arm and the underlying leg support the body. They move it upwards and forwards against gravity. In so doing, muscular activation in the underlying arm proceeds from the shoulder to the elbow and finally to the hand, where it finds support. The movement ends when the rolling sequence is completed in crawling.
- Fundamental Reactions are:
> Contrary flexion and extension movements of the over- and underlying arms and legs with increase in support function on the underlying shoulder progressing to the hand, and on the underlying pelvis progressing to the leg
> Extension of the spine during the entire rolling sequence
> Maintenance of the head in side lying, against gravity
- Even after treatment, the programme of the pattern of movement still remains active in the patient’s brain for differing lengths of time. Thus, the patient’s spontaneous access to the patterns activated in multiple daily treatment intervals often persists for the whole day, and the patient exhibits a lasting improvement in posture, movement and perception.

Reflex Rolling Tech. In Child
PHYSIOTHERAPY TREATMENT:
1. Passive Stretching:
- It is a manual application for spastic muscles to relieve soft tissue tightness. Manual stretching may increase range of movements, reduce spasticity, or improve walking efficiency in children with spasticity. Stretch may be applied in a number of ways during neurological rehabilitation to achieve different effects.
- The types of stretching used include:
> Fast / Quick
> Prolonged
> Maintained
When we look at the use of stretch for facilitation we employ a fast/quick stretch. The fast/quick stretch produce a relatively short lived contraction of the agonist muscle and short lived inhibition of the antagonist muscle which facilitates a muscle contraction. It achieves its effect via stimulation of the muscle spindle primary endings which results in reflex reflex facilitation of teach muscle via the monosynaptic reflex arc.
- The presence of increased tone can ultimately lead to joint contracture and changes in muscle length. When we look at the use of stretch to normalise tone and maintain soft tissue length we employ a slow, prolonged stretch to maintain or prevent lofss of range of motion. While the effects are not entirely clear the prolonged stretch produces inhibition of muscle responses which may help in reducing hypertonus, e.g. Bobath’s neuro-developmental technique, inhibitory splinting and casting technique. It appears to have an influence on both the neural compnents of muscle, via the Golgi Tendon Organs and Muscle Spindles, and the structural components in the long term, via the number and length of sarcomeres.
– Muscle Immobilised Shortened Position = Loss of Sacromeres and Increased Stiffness related to increase in connective tissue
– Muscle Immobilised Lengthened Position = Increase Sacromeres
– Studies in Mice show that a stretch of 30 mins daily will prevent the loss of sacromeres in the connective tissue of an immobilised muscle, although the timescale in humans mey not relate directly.

* Passive stretching may be achieved through a number of methods which include:
1. Manual Stretching:
Prolonged manual stretch may be applied manually, using the effect of body weight and gravity or mechanically, using machine or splints. Stretch should provide sufficient force to overcome hypertonicity and passively lengthen the muscle. Unlikely to provide sufficient stretch to cause change in a joint that already has contracture.
2. Weight Bearing:
Weight bearing has been reported to reduce contracture in the lower limb through use of Tilt-tables, and standing frames through a prolonger stretch. Angles are key to ensure the knees remain extend during the prolonged stretch as the force exerted on the knee can be quite high. Some research also challenges the assumption of the benefits of prolonged standing.
3. Splinting:
Splints and casts are external devices “Splints and casts are external devices designed to apply, distribute or remove forces to or from the body in a controlled manner to perform one or both basic functions of control of body motion and alteration or prevention in the shape of body tissue.” Splinting can be used to produce low- force, long duration stretching although there is a dearth of evidence to support this. A wide range of splint have been used to influence swelling ,resting posture, spasticity, active and passive ROM.
4. Serial Casting:
Serial casting is a common technique that is used and most effective in managing spasticity related contracture. Serial casting is a specialized technique to provide increased range of joint motion. The process involves a joint or joints that are tight which are immobilized with a semi-rigid, well-padded cast. Serial casting involves repeated applications of casts, typically every one to two weeks as range of motion is restored.
The duration of stretch to reduce both spasticity and to prevent contracture are not yet clear from the research and require further research to determine the most appropriate technique and duration to produce the required effect.
5. Static Weight-bearing Exercises:
Stimulation of antigravity muscle strength, prevention of hip dislocation, reduction in spasticity and improvements in bone mineral density, self-confidence and motor function have all been achieved through the use of Static Weigh Bearing exercises such as Tilt-Table and Standing Frame.
6. Muscle Strengthening Exercises:
It aims to increase the power of weak antagonist muscles and of the corresponding spastic agonists and to provide the functional benefits of strengthening in children with CP.
7. Functional Exercises:
Training related to specific functional activities combining aerobic and anaerobic capacity and strength training in ambulatory children, has been shown to significantly improve overall physical fitness, the intensity of activities, and quality of life. Training programs on static bicycles or treadmill have been shown to be beneficial for gait and gross motor development but have not shown to have any impact on spasticity or abnormal movement patterns.
8. Body Weight Supported Treadmill Training:
Stepping movements from Reflex Stepping Reactions are normally present in newborns and infants, before the infant starts to bear weight, stand and walk. Body Weight Supported Treadmill Training, is achieved through supporting the child in a harness on the treadmill in an upright posture limiting overall weight bearing, on a slow moving treadmill, eliciting the stepping movements. Treadmill training, thus allows development of stepping movements needed for ambulation. Studies using 3-4 sessions per week lasting for 3-4 months have shown improvement in lower extremity movements and gait patterns in children with cerebral palsy.
9. Electrical Stimulation:
The goal of the electrical stimulation is to increase muscle strength and motor function. Electrical stimulation is provided by Transcutaneous Electrical Nerve Stimulation (TENS) Unit which is portable, non-invasive and can be used in the home-setting by parents or the patient. Neuromuscular Electrical Stimulation (NMES) involves application of transcutaneous electrical current that results in muscle contraction. NMES has been postulated to increase muscle strength by increasing the cross-sectional area of the muscle and by increased recruitment of type 2 muscle fibers. Functional Electrical Stimulation (FES) refers to the application of electrical stimulation during a given task or activity when a specific muscle is expected to be contracting. Patel (2005) has shown there is some evidence to support the use and effectiveness of NMES in children with Cerebral Palsy but found that many of the studies are limited by confounding variables including concomitant use of other therapies, wide variation in methods of application, heterogeneity of subjects, difficulty in measuring functional outcomes and lack of control subjects. Mintaze (2009) proposes that neuromuscular and threshold electrical stimulation as a modality in Cerebral Palsy is used for strengthening the quadriceps muscles in ambulatory diplegic children with Cerebral Palsy, who have difficulty with specific resistive strength training.
10. Hippotherapy:
Gross Motor Function including Muscle tone, Range of Movement, Balance, Coordination and Postural Control in children with CP have been shown to improve with Therapeutic horse-back riding which may reduce the degree of motor disability. Many none physical benefits may also be developed through enjoyment and providing a setting for increased social interaction, cognitive and psychosocial development. Sharan et al (2005) have noted satisfactory results with Hippotherapy in Bangalore, especially in post-surgical rehabilitation. There is limited evidence available with two lower-quality trials on saddle riding on a horse found no between- group differences in muscle symmetry or in any of the seven different outcome measures, except on a sub-item of grasping.