Hippotherapy
Table of Contents
What is Hippotherapy?
Hippotherapy is a type of therapeutic intervention that involves using horses to help individuals with physical, cognitive, emotional, and sensory disabilities or challenges. The term “hippotherapy” is derived from the Greek word “hippos,” which means horse. This therapy aims to improve various aspects of an individual’s well-being through interactions with horses and horseback riding.
During hippotherapy sessions, a licensed therapist, often an occupational therapist, physical therapist, or speech-language pathologist, works with the individual while they are on horseback. The horse’s movements provide a dynamic and rhythmic motion, which can have therapeutic benefits. The therapist carefully designs activities that focus on specific goals, tailored to the individual’s needs.
Introduction:
- Physical Therapists: As a way to fulfill each patient’s motor needs and promote functional outcomes in gross motor skill domains including sitting, standing, and walking, the physical therapist can overlay a variety of motor activities over the horse’s movement.
- It supports physical rehabilitation programs, particularly for paralyzed people.
- According to the American Equestrian Association, hippotherapy enhances coordination, balance, postural control, cooperation, and motor growth. Therefore, enhancing balance, posture, function, and mobility is the main objective of hippotherapy.
- The equine movement offers varied, rhythmic, and repeated multidimensional movement. A dynamic base of support offered by the horse makes it a great tool for improving trunk strength and control, balance, general postural strength, and endurance, addressing weight bearing, and motor planning.
Who Can Benefit?
- Children as old as 2 may be allowed to take part.
Those who have the following diagnoses, including but not limited to:
- Cerebral Palsy
- Sensory Processing Difficulties
- Genetic Syndromes
- Developmental Delay
- Multiple Sclerosis
- Autism Spectrum Disorder
- Stroke
- Guillain -Barre Syndrome
- Traumatic Brain Injury (TBI)
Hippotherapy is a term for therapeutic horseback riding. Despite having a long history of use, the theoretical basis of it has only been the subject of a few research. On its psychological, physical, social, and educational implications in carefully trained youngsters, there is a dearth of information. With positive psychological, social, and educational impacts on a variety of organ systems, including the sensory, musculoskeletal, limbic, vestibular, and ocular systems, hippotherapy is a form of treatment.
History, and hippotherapy in the world
- Ancient Greek terms for “horse,” “hippos,” and “treatment” or “therapy” make up the term “hippotherapy.” It is defined as equine-assisted treatment. First of all, Hippocrates made reference to it in his writings. However, until the 1960s, it had not developed into a discipline with a set protocol. In Germany, Austria, and Sweden, it was utilized as a supplement to conventional physical therapy during the 1960s. The term “hippotherapy” was first used in medical literature to describe physical rehabilitation with horses in nations like Germany, Austria, and Sweden. Hippotherapy began to be standardized in the United States of America (USA) in the 1970s.
- A group of therapists from the United States and Canada who went to Germany to study hippotherapy at the end of the 1980s helped to standardize the practice. In 1992, the American Hippotherapy Association (AHA) was founded, and it set up a recognized, global protocol. The first certification exam takes place in 1999, while certification guidelines and standards for certified hippotherapy clinical specialists (HPSC) were created in the year 1994. This certification process includes three steps and a three-year training term.
- The American Hippotherapy Association’s certification program confers the designation of “hippotherapy clinical specialist” (HPSC) for hypnotherapists. These experts are knowledgeable and skilled in hippotherapy. The occupational therapist, speech, and language pathologist, and physiotherapist—each of whom has at least 6000 hours of formal education and 100 hours of practical experience—deserve to be on this team.
- Many American states, as well as Seul Province in Southern Korea, collaborate with AHA to offer their services globally. Many European nations, including Germany, Belgium, the Netherlands, Greece, and Sweden, offer general health insurance coverage for hippotherapy.
- Only a small number of centers in our nation offer comprehensive service. Additionally, the treatment these patients receive is non-standardized and uncontrolled. In our nation, standard health insurance does not cover hippotherapy. The Ministry of Health, Agriculture, and Livestock dedicates a number of hippotherapy facilities each year. It will be feasible to provide patients with efficient, secure, and dependable services thanks to the growth in the number of facilities offering certified hippotherapy training and the inclusion of hippotherapy sessions in standard health insurance.
What is the purpose of using horses?
- The horse’s rhythmic movement during ambulation produces anterior and posterior swinging movements.
The horse’s movements help the rider maintain good posture and balance. - The rider receives a wide range of sensory and motor information from the horse and the people around them.
- Through the horse’s varied, rhythmic, and repeated motions, horseback riding effectively and sensory stimulates the rider. The way the horse moves is similar to how the human pelvis normally moves when we walk. Therapists can assess sensory stimulation through variations in horse movement and combine these measures with therapeutic therapy to achieve desired results.
- The patient’s balance and muscle control are improved, and hippotherapy speeds up the healing process. The horse’s body moves slowly and rhythmically, which promotes paraspinal muscle growth and has therapeutic benefits. The pelvic girdle bones of a patient are affected by the complex swinging rhythm of a horse’s gait twice as strongly as they are by the gait of a patient. This interesting therapy method is receiving better cooperation and excitement from the patients. Therefore, hippotherapy enhances posture, movement, and balance.
Mechanism of action of hippotherapy
- While psychologists and mental health therapists take advantage of the horse’s mobility to encourage or promote patient cooperation, physical and educational therapists have taken advantage of the movements of the horse to treat patients.
- The horse pelvis exhibits a 3-axial movement pattern while walking, just like the human pelvis. Every stage of the patient’s treatment has involved carefully grading the horse’s gait. The patient receives physical and sensory feedback from these repetitive and varying rhythmic movements. Numerous studies have shown that equine-assisted treatment has positive physical effects on balance, muscle tonus, stiffness, endurance, and strength in addition to correcting abnormal movement patterns and improving gait.
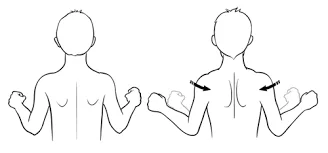
- There are four basic categories that describe how hypnosis works. The primary link is the first one. Balance, lying supine and walking, postural control, and core connection are known to be crucial for daily life performance. Hippotherapy also has a positive impact on core stability and postural control, which is only one of its many positive impacts. Direct touch with the patient’s spine and pelvis is made during horseback riding sessions used for hippotherapy. The horse’s movements give off sensory information and cause the pelvis and trunk to move. Sensory connection, communication connection, and neuro connection are further hippotherapy modes of action that might be listed.
- Hippotherapy has positive impacts on a variety of areas, including learning, adaptive behavior, and the physical, social, cognitive, and psychological domains.
Hippotherapy team
A therapist, a horse trainer, and riding instructors make up the Hippotherapy team. They all walk on opposite sides of the horse. Hippotherapy is conducted with a horse, a horse caretaker, and a skilled physiotherapist present. The patient experiences neuromuscular and sensory responses as a result of the physiotherapist controlling the horse’s gait, gait velocity, and orientation.
Indications for hippotherapy
Hippotherapy is effective for a variety of conditions, including cerebral palsy, traumatic brain injury, Down syndrome, autistic behavioral disorders, muscular dystrophy, amputees, multiple sclerosis, psychiatric disorders, spinal cord diseases, and rheumatoid joint diseases, among others.
Physical therapy using hippotherapy
- Equine multidirectional motions are used in physical therapy to train the horse’s gait, balance, postural control, strength, and range of motion. Numerous studies have shown that functional activities and gross motor skills have improved in children with disabilities.
- When used by a skilled therapist with the assistance of a horse, hippotherapy is a form of treatment whose effectiveness has been demonstrated in a significant number of patients with physical or mental problems. A lot of nations around the world use equine-assisted therapy. We believe that more patients and their families will benefit from hippotherapy as the value of this form of treatment is more widely acknowledged by doctors and therapists in our nation.
How does it work properly?
- A therapist with specialized training utilizes a horse as a “live” treatment tool in hippotherapy. Long-term and short-term therapeutic goals that are specific to each patient are achieved through the horse’s movement.
- The horses’ three-dimensional gaits closely resemble how the human pelvis often moves when walking. The patient’s anterior and posterior swinging movements are stimulated by the horse’s rhythmic, repeated, and multidirectional movements.
- A walking horse moves at a rate of 100 rhythmic impulses per minute. By repeatedly testing postural reactions, helps the patient stay balanced and in an upright position while continuing to sit on the horse. increasing paraspinal muscular development, muscle control, and balance.
- The horse and anyone nearby who are helping with the lesson provides the patient rider with a lot of sensory and motor information.
- Hippotherapy can produce good changes in children with neurological illnesses who present with a combination of cognitive, motor, and psychosocial difficulties when performed under the supervision of a licensed and qualified therapist. Strength, muscle tone, coordination, and sensory processing-all of which are important for speech, movement, and the use of fine motor skills for daily tasks-have all been shown to benefit patients.
Hippotherapy as a Physiotherapy Tool
The American Hippotherapy Association claims that hippotherapy is more appropriately referred to as a tool than as a therapeutic method, a stand-alone strategy, or a modality. Hippotherapy can therefore be used as part of a patient’s comprehensive treatment plan even though it requires a separate CPT (Current Procedural Terminology) billing code in countries like the US. The tool is not the horse itself. Instead, a trained physiotherapist using the horse to guide skillful movement and therapy procedures is the tool.
Who is qualified to offer hippotherapy?
- Once they have completed the required training and certification, the following healthcare professionals can either perform or supervise hippotherapy in most countries.
- Physiotherapists (PT)
- Occupational Therapists (OT)
- Speech-Language Pathologists (SLP)
- The Hippotherapy Clinical Specialist (HPSC) credential is provided by the American Hippotherapy Association in North America as a licensing program.
Safety measures and requirements for Hippotherapy participants, including horses, handlers, and assistants
- To ensure the security of everyone involved in hippotherapy, especially the patient, a team is necessary. A therapist who works with the patient is frequently part of a team that also includes a horse, a handler who leads the horse around an arena, and a therapy assistant or helper. In an emergency, therapists must be educated to safely demount the patient while the horse handler takes the animal away from the patient quickly and gently.
- The American Hippotherapy Association has specific criteria for horses that take part in hippotherapy. Horses used in hippotherapy have been evaluated and chosen based on their ability to maintain neutrality in the face of any potential distractions, such as other people, sounds, sights, and experiences. They have also been chosen based on their body mechanics and gait patterns while ambulating, ability to understand and follow instructions given by the handler rather than the patient mounted on the horse. When a patient is receiving therapy, the handler is in charge of the patient’s safety, the horse’s health, and the horse’s behavior in relation to the therapist’s instructions and guidance. A therapy assistant or sidewalk may also be used during therapy. These people are volunteers who are not licensed and who can help a therapist maintain a patient’s safety while they remain on the horse.
Who may benefit from hippotherapy?
Benefits of Hippotherapy:
- Balance
- Arousal and attention
- Body awareness
- Joint mobility
- Muscle strength
- Endurance
- Posture
- Timing
- Coordination
- Sequencing
- Hippotherapy can help a wide range of individuals of all different ages, backgrounds, and medical histories. Hippotherapy has been demonstrated to improve motor and neuromuscular re-education outcomes for patients with cerebral palsy. This would entail improved stability and control of the head and trunk as well as functional upper-limb reaching. Improvements in motor performance in activities requiring balance, strength, and postural control as well as psychological improvements in confidence and self-esteem have been observed in children with autism and developmental delays. Patients who frequently experience overstimulation have reported a soothing effect following periods spent walking on a horse, which has enabled improvements in speech, fine motor skills, and gross motor abilities.
- Children with various physical and mental problems make up the majority of the patient group for hippotherapy.
- Cerebral Palsy
- Autism
- Traumatic Brain Injury
- Behavioral Disorders
- Down Syndrome
- Muscular Dystrophy
- Cerebrovascular Accidents
- Amputees
- Multiple Sclerosis
- Rheumatism Joint Diseases
- Psychiatric Diseases
- Spinal Cord Injuries
- Rheumatism Joint Diseases
- Developmental Dyspraxia and Delay
Physiotherapy and Hippotherapy
- Patients’ physical requirements and riding capabilities can be taken into account when creating treatment programs by a physiotherapist with specialized training in hippotherapy. The therapist will adjust the rider’s position and the horse’s movements to achieve functional results in the following areas:
- Balance
- Gait training
- Strengthening
- Postural control
- Range of motion
- Proprioception
- Vestibular input
- Normalization of muscle tone
Common physical therapy exercises used in association with hippotherapy
- Numerous multi-targeted physiotherapy exercises can be combined with hippotherapy. Throwing a ball to a target to improve hand-eye coordination, reaching in all directions to challenge and improve trunk and postural control and balance, and normalizing muscle tone to elicit functional movement patterns are typical objectives set for pediatric populations. Basketball goals are a common piece of equipment used by physiotherapists to encourage patients to toss a ball to a target while remaining balanced and erect while mounted. To present the patient with even more of a challenge, the horse may occasionally be mobile. Other regular exercises include horseback fishing with a line and placing handheld objects in color-coated buckets as the patient extends outside their base of support and sitting forward with both upper extremities supporting a patient to maintain a modified quadruped position while the horse is ambulatory.
- Benefits Improvements in:
- Muscle tone and strength
- Gross motor skills
- Fine motor skills
- Range of motion
- Coordination
- Endurance
- Symmetry
- Body awareness
- Mobilization of the pelvis, lumbar region, and hip joints
- Balance
- Head and trunk control
- Body awareness
- Posture
- Mobility
- Hand-eye coordination
- Arousal, motivation, and attention span are all connected to limbic system function
- Sensorimotor function
- Voice quality, oral motor ability, and vocal communication
- Emotional and cognitive well-being
- Self-esteem
- Confidence
- Didactic and group interaction
- Concentration
Contraindications And Precautions
- Listed below:
- Active mental health problems that would be dangerous
- An acute herniated disc that may or may not cause nerve root compression
- Chiari II malformation with neurologic symptoms
- Atlantoaxial instability
- Coxarthrosis
- Grand mal seizures – uncontrolled by medications
- Haemophilia with recent episodes of bleeding
- Indwelling urethral catheters
- Medical disorders (Rheumatoid Arthritis, herniated nucleus pulposis, Multiple Sclerosis, Diabetes, etc.) during acute exacerbations
- Open wounds over a weight-bearing surface
- Pathologic fractures that have not been treated successfully for the underlying disease (e.g., severe osteoporosis, osteogenesis imperfecta, bone tumor, etc.)
- Tethered spinal cord with symptoms
- Unstable spine or joints, as well as the faulty internal hardware
- Uncontrollable seizures
- Moderate agitation with severe confusion, disruptive behavior
- Exacerbation of Multiple Sclerosis
- Hemophilia
- Coxarthrosis
- Any spinal fusion, organic or operative
- Spondylolisthesis
- Unstable spine, including subluxation at the cervical level
- Acute herniated disc
- More than 30 degrees of structural scoliosis; severe kyphosis or lordosis; hemivertebrae
- Atlantoaxial instability
- Pathological fractures
- The cerebrovascular accident was caused by an angioma that was not completely removed
- Cerebrovascular Accident secondary to an unclipped aneurysm or the presence of other aneurysms
- Open pressure sores or wounds
- Detached retina
- Anticoagulant medications
- Complete quadriplegia
- Acute stage of arthritis
- Severe osteoporosis
- Dosages of drugs that cause bodily states unsuitable for cycling
- Any patient with whom the therapist is not totally confident in treating
- Precaution:
Patient safety equipment
Before introducing a patient to and riding a horse, the correct riding equipment should be provided. A well-fitted helmet is a must-have item, and a variety of sizes should be available for patients to choose from. Helmets should be able to fit comfortably over the patient’s head and should come up just over the brow line. The chin strap should be tight enough to prevent side-to-side mobility with a head shake. Patients should also be provided with a gait belt. Gait belts frequently include two handles to offer optimal safety for both the therapist and the patient. Two handles allow the Physiotherapist and a side-walker to keep a firm grip on the patient. If the Physiotherapist is holding both handles, the side-walker should maintain gentle contact with the patient’s leg if necessary.
Hippotherapy horse care and criteria
- Horses have basic need requirements that include:
- Nutritious foliage (grass and hay)
- Adequate clean water
- Sufficient free roaming space and housing
- Teeth floating
- Hoof maintenance
- Annual vet visits for vaccinations and Coggins testing Because of their age and health requirements, certain horses may require more care.
- In the majority of cases, a PT will not be accountable for a horse’s care because the animal is cared for by someone else (the horse’s owner or barn management). Horses can be boarded off-site or on-site, depending on what is going on. Additional charges for off-site or on-site boarding may occur depending on the specifics of the situation. Another factor to consider is horse transportation if horses are housed off-site.
- Criteria of a therapy horse:
- The horse must exhibit a docile demeanor.
- The horse must be free of any problem that interferes with temperament or movement (for example, poor balance and symmetry).
- The horse must be desensitized to unexpected external motions, noises, and PT tools or objects.
- For mounting and dismounting, as well as grooming and tacking, the horse must be able to stand calmly. Horses must be knowledgeable in “barn etiquette.” People and other animals should avoid bothering them.
- These are generalized requirements. Depending on the situation, facilities may demand more detailed standards.
FAQs
Hippotherapy is administered by a physical, occupational, or speech therapist who has received American Hippotherapy Association (AHA) certification. Hippotherapy’s purpose is to increase function, not to teach riding abilities. The therapist directs the horse’s movement rather than the child’s in hippotherapy. If a disabled youngster wants to learn to ride, search for a riding instructor who has received the Professional Association of Therapeutic Horsemanship International (PATH) certification.
Activities may involve the head, trunk, pelvis, arms, and legs, depending on the child’s therapeutic goals. Balance, coordination, range of motion, posture, strength, and fine and gross motor skills are all developed through activities.
A doctor’s prescription is essential before beginning hippotherapy. A physical, occupational, or speech therapist will then assess your kid to determine if hippotherapy is the best treatment for him or her.
A 30-minute hippotherapy session is typical. The length of a course of hippotherapy is determined by a variety of factors, including the therapist’s initial assessment, the client’s goals, and subsequent reviews at regular intervals. Some individuals may just require a few sessions before they are ready to join a therapeutic riding group. Others may like riding and have a few hippotherapy sessions now and again to work on certain areas. Hippotherapy could be a regular treatment to supplement other therapies for some people.
Depending on the patient’s wishes and capacity, hippotherapy can serve as a bridge to riding, vaulting, and carriage driving.
Equine-facilitated psychotherapy (EFP), equine-assisted therapy (EAT), Equine Facilitated Wellness (EFW), Equine Facilitated Counselling (EFC), and Equine Facilitated Mental Health (EFMH) are some additional terms for equine psychotherapy.