Cardiac Arrest
- During cardiac arrest, an electrical problem creates your heart to stop pumping blood to your body. Without blood flowing, you become unconscious and do not have a pulse. Cardiac arrest (CA), or sudden cardiac arrest, can be fatal in minutes. This is why you should call 911 and begin CPR right away. Chances of survival are better with immediate assistance.
- Cardiac arrest (CA) is a serious heart condition. The word arrest means to end or bring to a pause. In cardiac arrest, the heart halts to beat. It is also referred to as sudden cardiac arrest.
- Your heartbeat is controlled by electrical impulses. When these impulses exchange patterns, the heartbeat becomes irregular. This is also called arrhythmia. Certain arrhythmias are slow, others are rapid. Cardiac arrest happens when the rhythm of the heart stops.
- Cardiac arrest is an extremely serious health issue. The Institute of Medicine reports that every year, more than half (1/2) a million people experience cardiac arrest (CA) in the United States (US). The condition can cause death or disability. If you or someone you are with is experiencing symptoms of cardiac arrest, seek emergency health assistance immediately. It can be fatal. Immediate response & treatment can save the life.
Table of Contents
What is cardiac arrest?
- Cardiac arrest (CA) happens when your heart ends up beating or beats so fast that it ends up pumping blood. During cardiac arrest (CA), people typically collapse & become unresponsive.
- Symptoms begin without warning. This is why it is also known as unexpected cardiac arrest. The condition can become fatal if you do not get immediate treatment.
Why do cardiac arrests happen?
- With cardiac arrest (CA), abnormal, rapid impulses abruptly override the normal electrical impulses that begin your heartbeat. When your heart is not beating, there is no way to get oxygen-rich blood to the rest of your body.
Cardiac arrest vs. heart attack
Here is how cardiac arrest and heart attack are different:
- Cardiac arrest (CA) occurs when rapid, abnormal impulses override your heart’s natural rhythm. It is an electrical issue.
- A heart attack occurs when a clogged artery disrupts blood flow to your heart. A heart attack is a usual cause of cardiac arrest.
Is cardiac arrest the same as sudden cardiac death?
- With cardiac arrest (CA), your heart stops beating, yet a rescue is still possible. With immediate treatment, you can survive.
- Sudden cardiac death refers to a cardiac arrest (CA) without someone saving you.
Who does cardiac arrest affect?
- Sudden cardiac arrest (CA) occurs in people with and without heart disease. Having a heart attack or another heart condition can significantly increase your risk.
- More than 356,000 Americans each year experience cardiac arrest (CA) outside of a hospital. It typically harms adults. Only 3% of cases include children.
What are the symptoms of cardiac arrest?
Fainting can mean you are going into cardiac arrest. Symptoms of cardiac arrest involve:
- Racing heartbeat (heart palpitations),
- Dizziness,
- Lightheadedness.
Are there warning signs before cardiac arrest?
Yes. Previous you faint, you may have other cardiac arrest symptoms, involving:
- Chest pain,
- Nausea and vomiting,
- Shortness of breath.
Is cardiac arrest painful?
Certain people have chest pain before they become unconscious from cardiac arrest (CA). However, you who not feel pain once you lose consciousness.
What causes cardiac arrest (CA)?
Irregular heart rhythms (arrhythmias) are the immediate cause of cardiac arrest (CA).
Abnormal heart rhythms that cause cardiac arrest may involve:
- Ventricular fibrillation,
- Ventricular tachycardia.
Conditions and situations that can conduct to these abnormal heart rhythms are the underlying causes of sudden cardiac arrest. These involve:
- Cardiomyopathy
- Drugs for other medical conditions, involving cold medicine (in some people)
- Heart attack
- Heart failure
- Illegal drugs, like cocaine,
- Inherited heart disorders, such as Brugada syndrome,
- Long QT syndrome (LQTS)
- Severe illness or harm (trauma) with major blood loss.
What are the most common causes of sudden cardiac arrest in children?
Conditions or accidents that can make a child’s heart suddenly stop beating involve:
- Congenital heart disease
- Infectious diseases
- Respiratory conditions
- Severe injury (trauma)
- Toxins (ingesting poisonous substances).
These issues lower oxygen levels or decrease the volume of blood. This cures your heart from functioning.
How do you detect cardiac arrest?
Cardiac arrest (CA) symptoms start suddenly, leaving little time for tests. The condition can become a few within minutes. This is why a fast diagnosis is essential.
A person’s symptoms are sometimes the best way to diagnose cardiac arrest, especially if they:
- Are unconscious,
- Have no pulse.
Diagnosing Cardiac Arrest
- During a cardiac event that causes your heart to end beating efficiently, it is vital to seek medical attention immediately. Medical treatment will focus on getting the blood flowing back into your body.
- Your doctor will most likely perform a test known as an electrocardiogram to identify the type of abnormal rhythm your heart is experiencing.
- To treat the condition, your doctor will such as use a defibrillator to shock your heart. An electric shock can sometimes return the heart to a normal rhythm.
Other tests can also be used later you have experienced a cardiac event:
- Blood tests can be used to see for signs of a heart attack. They can measure potassium & magnesium levels.
- Chest X-ray can see for other signs of disease in the heart.
How is cardiac arrest treated?
Emergency cardiac arrest treatment involves restarting your heart and restoring a regular rhythm. Care involves using:
- Cardiopulmonary resuscitation (CPR): Immediate cardiopulmonary resuscitation (CPR) is one of the most important treatments to improve cardiac arrest survival. cardiopulmonary resuscitation (CPR) is often performed until an automatic or external defibrillator is ready. cardiopulmonary resuscitation (CPR) uses chest compressions to replace the heart’s pumping action. It moves little amounts of blood from your heart to your brain.
- Automatic defibrillator or external defibrillator: Once connected, this device delivers a short electrical current (shock) to your chest. The current moves to your heart. This stops the abnormal impulses & restores the normal impulses that create it beat. It may take more than one shock for your heart to pump on its own again.
- Cardiopulmonary resuscitation (CPR) is the first form of emergency treatment for cardiac arrest (CA). Defibrillation is another one. These treatments bring your heart to beating again once it has stopped.
- If you survive a cardiac arrest (CA), your doctor may begin one or more treatments to reduce the risk of another attack.
- Medication can lower high blood pressure (HBP) and cholesterol.
- Surgery can repair damaged blood vessels or heart valves. It can bypass or remove blockages in the arteries.
- Exercise may increase cardiovascular fitness.
- Dietary changes can assist you to lower cholesterol.
Cardiac Rehabilitation: Physical Therapy After a Heart Attack
- A heart attack or cardiac arrest (CA) can be a frightening experience. Still, many people who have had a heart attack go on to enjoy full lives.
- As part of your recovery, your doctor may recommend cardiac rehabilitation later in a heart attack or cardiac arrest (CA).
- Cardiac rehabilitation is a program designed to improve your cardiovascular health & quality of life later in a heart attack or another heart problem.
The program is supervised by a team of medical professionals, involving:
- physical therapists
- registered dieticians
- doctors
- nurses.
Physical therapy is a main part of the cardiac rehabilitation process. It might assist you:
- Decrease your risk of having another heart attack
- increase your quality of life,
- improve your cardiovascular fitness.
What is cardiac physical therapy?
- Heart attacks are the conducting cause trusted Source of death in the United States (US). According to the American Heart Association (AHA)Trusted Source, the average age for a 1st heart attack in the United States (US) is 65.6 years for men & 72.0 years for women.
- Cardiac rehabilitation is a program to assist you to recover from a heart attack & improve your quality of life. This program is critical for minimizing your chances of having another heart attack (HA). It often begins while you are in the hospital or shortly later you leave.
- According to the Centers for Disease Control & Prevention (CDC)Trusted Source, anybody who has had a heart problem, such as a heart attack (HA), can benefit from cardiac rehabilitation. Most programs last about three months, but they can last anywhere from two to eight months.
A cardiac rehabilitation program consists of:
- exercise counseling & training
- education for managing risk factors
- counseling to decrease stress.
- A physical therapist commonly leads the physical activity portion of a cardiac rehabilitation program. A 2014 review trusted Source suggests the aim of the program is to increase your exercise capacity & quality of life in the short term & long term.
- Staying physically active later in a heart attack is the main for keeping your heart strong. Research from 2018Trusted Source has found that increased physical activity in the 1st year later a heart attack is related to a reduced chance of death.
- A physical therapist can assist assess your current fitness levels & create a detailed exercise program for you to improve your fitness.
What are the benefits of cardiac physical therapy?
- Attending a cardiac rehabilitation program gives you the best chance to avoid a future heart attack (HA) and increase your quality of life.
Research has found that cardiac rehabilitation can:
- increase your health-related quality of life trusted Source and functional capacity
- decrease your risk of future heart attack trusted Sources
- increase your lung capacityTrusted Source
- increase your heart health
- strengthen your heart and body
- assist you to maintain moderate body weight
- increase your blood pressure
- increase your mental healthTrusted Source
- increase your ability to work
- decrease your body pain
- assist you to reduce stress
- increase your energy and endurance
- increase your exercise, dietary, and lifestyle habits.
Cardiac rehabilitation is not just for heart attacks (HA)
- Physical therapy & cardiac rehabilitation are important parts of the recovery for many types of heart surgery or cardiac events.
Rehabilitation can assist you to bounce back from:
- heart failure
- heart valve surgery
- coronary artery bypass
- stent placement
- heart transplant
- chronic stable angina
- acute coronary artery syndrome (CAS).
What can you expect during cardiac physical therapy?
- Cardiac rehabilitation often starts while you are in the hospital or just later leaving. Each program is tailored to your personal requirements.
- A 2016 review indicates that the physical activity program commonly consists of 36 sessions over 12 weeks, yet some programs can be longer.
- At the beginning of your rehab, a physical therapist will assess your ability with a physical exam and possibly fitness tests or imaging of your heart. They will then design a custom program that improves in intensity over time.
According to 2020 guidelines, your physical therapy may involve:
- aerobic exercise to strengthen your heart,
- counseling to increase exercise and lifestyle habits,
- resistance training to strengthen your bones & muscles,
- exercises to retrain your breathing mechanics,
- balance & flexibility training.
- While you are also in the hospital, your physical therapist may guide you through exercises in bed that are not strenuous. These exercises aim to increase your range of motion and prevent deconditioning and stiffness from extended bed rest.
- Once you leave the hospital, a typical exercise session might include riding an exercise bike, jogging, or using other cardiovascular fitness. Your physical therapist will monitor your heart rate, blood pressure (BP), respiration rate, & oxygen level while you exercise to assess how your body responds.
What are the risks of cardiac physical therapy?
- Certain people may not make good candidates for the exercise portion of cardiac rehabilitation, like people with unstable anginaTrusted Source. Your doctor can assist you to figure out if you have a condition that may preclude you from exercise.
- Programs that involve intensive aerobic exercise and resistance training are considered safe by many leading health authorities.
- Serious risks are very certain. A 2006 study from France found that the rate of cardiac arrest (CA) was 1.3 per million hours of Trusted Source of exercise.
- A little 2017 study trusted Source of people who received heart rhythm management devices found that those who underwent cardiac rehabilitation had fewer complications than those who did not.
What do I need to know previous I start cardiac rehabilitation?
- Cardiac rehabilitation needs a referral from your doctor. Your doctor can let you know what your program will involve.
- If you have insurance, it is a good idea to make sure your policy will cover treatment before you start. Certain people may not be covered, such as those who have received a heart rhythm management device.
- The AHATrusted Source says that Medicare and most other insurance providers offer reimbursement for cardiac rehabilitation for treating heart attacks (HA). According to the National Heart, Lung, & Blood Institute, Medicare covers 36 supervised sessions rushed Source over 12 (twelve) weeks.
What is the outlook for later cardiac rehabilitation?
- Attending cardiac rehabilitation gives you the best chance to maintain a high quality of life and cure another heart attack.
- A 2021 review indicates that participants may have a 13 percent trusted Source lower chance of having another heart attack (HA).
- A 2016 study by trusted Sources found that in a group of 4,929 people who experienced heart attacks (HA), people who underwent cardiac rehabilitation lived significantly longer.
- Studies have found that cardiac rehabilitation decreases your chances of dying in the 5 (five) years after a cardiac event from any cause by about 32 percent trusted Source.
- Talk with your doctor about how cardiac rehabilitation can improve your recovery later a heart attack (HA).
How quickly should I receive treatment for cardiac arrest (CA)?
- Cardiac arrest can be fatal if it lasts longer than eight minutes without CPR. Brain damage can occur after just 5 minutes.
- Cardiac arrest treatment should begin right away, even if you are not in the hospital. If you are in a public area, like a school, mall, or sports venue, CPR & an automated external defibrillator (AED) can assist.
- An automated external defibrillator (AED) is a device that a person without medical training can use to shock someone else’s heart. The automated external defibrillator (AED) confirms there is no heartbeat before delivering the shock.
How can I reduce my risk?
If abnormal heart rhythms run in your family, you may want to ask a genetic counselor. They can tell you who might be at risk or require testing for an issue that causes arrhythmia.
Testing can let you know whether you are at risk for sudden cardiac arrest. Healthcare providers or doctors may recommend:
- Cardiac catheterization: A procedure to check arteries overlying your heart for obstruction of normal blood flow.
- Echocardiogram (echo): A test that uses sound waves to see heart movement to understand heart function & heart valve function.
- Electrocardiogram (EKG): A test that data on the electrical activity of your heart.
- Electrophysiology study: A detailed assessment of the electrical activity in your heart.
- Exercise stress echocardiogram: A test that assesses heart movement during monitored exercise.
- Magnetic resonance imaging (MRI): A scan that uses a magnet & radio waves to produce heart images.
- Multigated acquisition (MUGA) scan: A test that assesses heart functioning using a radioactive substance.
How can I prevent cardiac arrest (CA)?
Treatments that can cure cardiac arrest (CA) or lower your risk of a second episode involve:
- Implantable cardioverter defibrillator (ICD).
- Other arrhythmia treatments in susceptible people.
- Medicines like beta-blockers.
- Fixing heart artery blockages with either coronary artery bypass surgery (CABG) or angioplasty.
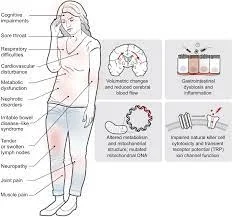
What can I expect if I have a cardiac arrest (CA)?
- Nearly nine out of ten people who survive cardiac arrest (CA) have permanent brain damage from a lack of oxygen. This can lead changes to in your daily life and abilities.
You may experience:
- Ataxia, which harms movement & coordination
- Coma and persistent vegetative state
- Difficulty concentrating
- Dysphagia (swallowing issues)
- Fatigue
- Forgetfulness
- Muscle weakness
- Seizures
- Speech disorders, involving dysarthria
- Stroke
- Unusual behaviors, such as being impulsive
- Vision problems, like low vision.
Survival without brain injury is far more likely with early CPR and defibrillation.
Does cardiac arrest (CA) mean death?
- While most people do not survive a cardiac arrest, survival rates are better than they were just ten years ago. About 11% of people who have a cardiac arrest (CA) outside a hospital and get emergency treatment to survive and go home from the hospital. About 26% of people who have cardiac arrest (CA) inside a hospital survive & go home.
How will life be different later in surviving sudden cardiac arrest (CA)?
- You may have no memory of your heart-stopping. Certain people wake up in the hospital days after. After returning home, it is not uncommon for complications to happen. You may require to go back to the hospital for more treatments.
- Rehabilitation later during your hospital stay can assist maximize your abilities. It can months to relearn once-simple activities like walking and getting dressed. Many people return to their daily lives, yet some need ongoing help.
- Researchers have seen improvements in cardiac arrest survivors’ quality of life later in 6 months.
What else can I expect?
Surviving life-threatening conditions can cause mental health challenges (post-intensive care syndrome).
You may benefit from mental health services to assist you to cope with:
- Anxiety.
- Depression.
- Post-traumatic stress disorder (PTSD).
- Stress.
How do I take care of myself?
A cardiac arrest is a traumatic event that most people do not survive.
- Be patient with yourself while you steadily get back to being able to do things you did every day.
- Take advantage of any programs that assist you to get back to normal life.
- Keep your checkup appointments with your healthcare provider or doctor.
When should I go to the ER?
If you look at someone unconscious, the better thing to do is call 911. They can send assistance & talk you through giving CPR.
What questions should I ask my doctor?
- Should I buy an AED to retain at home?
- Are there any programs available to assist me to adjust to my new reality?
- Is my family at risk for cardiac arrest?
FAQs
Cardiac arrest occurs when your heart suddenly stops beating. Unlike heart attacks, which are due to blocked arteries, this condition occurs when there is a problem with your heart’s electrical system. It is life-threatening and requires immediate treatment.
Cardiac arrest is the abrupt loss of heart function in a person who may or may not has been diagnosed with heart disease. It can come on suddenly, or in the wake of other symptoms. Cardiac arrest is often fatal if appropriate steps aren’t taken immediately. Get support. Or offer it. Make a connection. For life.
Sudden cardiac arrest occurs in people with and without heart disease. Having a heart attack or other heart condition can significantly increase your risk. More than 356,000 people each year experience cardiac arrest outside of a hospital. It typically affects adults. Only 3% of cases involve children.
Certain heart conditions and health factors can increase your risk of cardiac arrest. This type of heart disease begins in the coronary arteries. These arteries supply the heart muscle itself. When they become blocked, your heart does not receive blood. It may stop working properly.
Fainting can mean you are going into cardiac arrest. Symptoms of cardiac arrest include:
1. Racing heartbeat (heart palpitations).
2. Dizziness.
3. Lightheadedness.




One Comment