Thoracic Injury
Table of Contents
What is Thoracic Injury?
Thoracic injuries can be broadly divided into blunt and penetrating injuries based on their mechanism. The most common cause of blunt chest injury is motor vehicle collisions (MVC) which account for up to 80% of injuries. Other causes include slips and falls, violent crimes, vehicles striking pedestrians, and blast injuries.
Children and adults both can suffer from thoracic injuries, which are a significant cause of morbidity and mortality. It is a leading cause of death in approximately 20% of multiple thoracic injury patients and, when associated with other injuries, it causes death in an additional 40% to 50% of multiple thoracic injury patients, normally as a result of hypoxia and hypovolemia. When The most important issue with thoracic injury is to prevent lethal outcomes because many more of these wounds are fatal shortly after the injury or a few hours afterward. The thoracic injury might occur in isolated thoracic trauma or in the presence of polytrauma.
Etiology divides thoracic injuries into damaging chest wounds and blunt traumas.
Pulmonary barotraumas, tracheobronchial tree burns from aspiration, blast lung injury, parenchymal lung damage from aspiration, and accidental harm are a few examples of specific injuries.
Fractures associated with the chest wall might be caused by a direct force, and the tissues and organs of the chest might be damaged including contusions, lacerations, or rupture. Additionally, traumatic forces may manifest their effects after the tissue has disintegrated (for example, an air embolism caused by the entry of air into the pulmonary veins following lung lacerations).
Road traffic accidents cause the majority of blunt injury cases (70%) while front-seat motor vehicle occupants and motorcycle drivers are substantially less likely to get injuries (10%) but are more likely to die at the scene of crashes (30%).
There are five different types of motor vehicle-related injuries: head-on collisions, side impacts, rear impacts, rotating impacts, rollovers, as well as injuries resulting from deceleration and crushing. A quickly moving body is suddenly halted to a stop when decelerating, causing injuries to the chest wall and internal organ damage as a result of reflex glottic closure and the resulting rapidly rising intra-thoracic pressure.
The transverse thoracic diameter increased quickly, and the tracheobronchial tree was injured along with the lung parenchyma, diaphragm, and mediastinal structures when the traumatic force overcame the elastic limit of the lungs. The identical mechanism that causes falls also causes injuries from deceleration.
Penetrating thoracic injuries occur as a result of side arms and are divided into three groups:
- ” Sleeper ” injuries (no exit injuries)
- Perforating injuries (entrance injuries and exit injuries)
- Injuries in which the projectile penetrates during the complete intra-thoracic space and remains in the subcutaneous tissue.
If a deformity in the chest wall is large, an open pneumothorax happens. In small deformities, injuries close spontaneously due to the contraction of muscle or blood clotting. still, it should be always borne in mind that initiating communication between the external environment and the pleural space leads to the suction of air and innervate tissue in the pleural space, favoring infection development and other complicating the clinical management of the injuries.
What are The Signs and Symptoms of Thoracic Injury?
Symptoms involve pain, which normally worsens with breathing if the chest wall is injured, and a few time shortness of breath.
Common findings involve chest tenderness, swelling, and respiratory distress; hypotension or shock might be present.
Neck vein distention can occur in tension pneumothorax or cardiac tamponade if patients have sufficient intravascular volume.
Decreased breath sounds can result from hemothorax or pneumothorax percussion on the affected areas is dull with hemothorax and hyper resonant with pneumothorax.
The trachea can diverge away from the side of a tension pneumothorax.
In the flail chest, a division of the chest wall moves paradoxically that is, in the opposite direction from the rest of the chest wall (outward during expiration and inward during inspiration) the flail division is often palpable.
Subcutaneous emphysema causes a crunch when palpated. Findings might be localized to a little area or include a large portion of the chest wall and extend to the neck. When a significant tracheobronchial tree or upper airway injuries should be taken into consideration, pneumothorax is most commonly the cause. Air in the mediastinum might annoy a typical crunching sound synchronous with the heartbeat (Hamman sign or Hamman crunch). The Hamman sign suggests pneumomediastinum and often tracheobronchial tree injury or, rarely, esophageal injury.
Causes of Thoracic Injury
Chest injuries can outcome from blunt or penetrating injuries. The most important chest injuries involve the following:
- Aortic disruption
- Blunt cardiac injury
- Cardiac tamponade
- Flail chest
- Hemothorax
- Pneumothorax (open pneumothorax, traumatic pneumothorax, and tension pneumothorax)
- Pulmonary contusion
More people suffer hemopneumothorax, which is a combination of hemothorax and pneumothorax.
Bone injuries are common, commonly including the ribs and clavicle, but fractures of the sternum and scapula might occur. Chest injuries may result in damage to the esophagus and diaphragm (see Overview of Abdominal Injury). Penetrating injuries to the chest at or below the nipple level may result in intra-abdominal injuries because the diaphragm can rise as high as the nipple line during exhale.
Pathophysiology of Thoracic Injury
Most mortality and morbidity due to thoracic injury occurs because injuries inhibit respiration, circulation, or both.
Respiration can be compromised by
- Direct damage to the lungs or airways
- Altered mechanics of breathing
Injuries that directly damage the lung include tracheobronchial disruption and pulmonary contusion. Injuries that alter the mechanics of breathing involve hemothorax, pneumothorax, and flail chest. Injury to the lung, tracheobronchial tree, or not often esophagus might allow air to enter the soft tissues of the chest and neck or mediastinum. This air itself rarely has significant physiologic consequences the key injury is the problem. Tension pneumothorax damages respiration as well as circulation.
Circulation can be impaired by
- Bleeding
- Decreased venous return
- Direct cardiac injury
Bleeding, as occurs in hemothorax, can be massive, causing shock (respiration is also damaged if hemothorax is large). Decreased venous return damages cardiac filling, causing hypotension. Decreased venous return can occur due to increased intrapericardial pressure in cardiac tamponade or increased intrathoracic pressure in tension pneumothorax. Heart failure and conduction abnormalities can result from a blunt cardiac injury that damages the heart valves or myocardium.
Diagnosis of Thoracic Injury
- Clinical evaluation,
- Chest x-ray,
- Sometimes more imaging studies (eg, CT, ultrasonography, aortic imaging studies).
Clinical evaluation
Five conditions are immediately life-threatening and quickly correctable:
- Massive hemothorax,
- Tension pneumothorax,
- Open pneumothorax,
- Flail chest,
- Pericardial tamponade.
Diagnosis and treatment begin during the primary survey (see Approach to the Injured Patient) and are based first on clinical findings. Depth and symmetry of chest wall excursion are evaluated, the lungs are auscultated, and the entire chest wall and neck are inspected and palpated. Patients in respiratory distress should be observed with successful assessments of clinical status and of oxygenation plus ventilation (eg, with pulse oximetry, arterial blood gas tests, and capnometry if intubated).
Penetrating chest wounds should not be probed. Still, their location assists predict the risk of injury. Most acute injuries are middle to the nipples or scapulae and traverse the chest from side to side. like wounds might injure the great vessels, heart, tracheobronchial tree, or not often the esophagus.
Patients with symptoms of complete or partial airway difficulty following blunt trauma should be quickly inserted to control the airway.
In patients with difficulty breathing, severe injuries to examine during the primary survey involve the following:
- Tension pneumothorax,
- Open pneumothorax,
- Massive hemothorax,
- Flail chest.
There is a simplified, rapid approach to assist differentiate these injuries.
In patients with thoracic trauma and impaired circulation (signs of shock), severe injuries to consider during the primary survey include the following:
- Massive hemothorax,
- Tension pneumothorax,
- Cardiac tamponade.
Other chest injuries (eg, blunt cardiac injury, aortic disruption, etc) may cause shock but are not treated through the primary survey. Simplified, fast approaches can assist differentiate between quickly repairable causes of shock due to chest injuries. However, hemorrhage should be excluded in patients who have shock after a crucial injury, regardless of whether a chest injury that could cause shock is remembered.
Treatment of injuries affecting the airway, breathing, or circulation initiates during the primary survey. After the primary survey, patients are clinically assisted in more detail for other acute chest injuries as well as less severe manifestations of the injuries considered during the primary survey.
Imaging
- Imaging studies are typically needed in patients with significant chest injuries. The chest X-ray is virtually always done. Outcomes are commonly diagnostic of certain injuries (eg, pneumothorax, hemothorax, moderate or acute pulmonary contusion, clavicle fracture, few rib fractures) and suggestive of more (eg, aortic disruption, diaphragmatic rupture). still, findings might evolve over hours (eg, in pulmonary contusion and diaphragmatic injury). Plain X-rays of the sternum or scapula are occasionally done when there is tenderness over those structures.
- In injury centers, during the E-FAST (Extended Focused Assessment With Sonography in Trauma) examination, ultrasonography of the heart is normally done during the resuscitation phase to look for pericardial tamponade few pneumothoraces can also be seen.
- Computed Tomography (CT) of the chest is usually done when the aortic injury is suspected and to diagnose small pneumothoraces, sternal and rib fractures, or mediastinal (eg, heart, esophageal, bronchial) injuries thoracic spine injuries also will be remembered.
- Other tests for aortic injury involve aortography and transesophageal echocardiography.
Laboratory and other testing
- The complete blood count is often done but is most valuable as a baseline for detecting ongoing hemorrhage. Arterial blood gas results assist monitor patients with hypoxia or respiratory distress. Cardiac markers (eg, troponin, creatine phosphokinase muscle band isoenzyme) can aid exclude blunt cardiac injury.
- ECG is normally done for chest injury that is acute or compatible with cardiac injury. The cardiac injury might cause arrhythmia, conduction deformity, ST segment deformity, or a combination.
Treatment of Thoracic Injury
- Supportive care
- Treatment of specific injuries
Immediately life-threatening wounds are managed at the bedside at the time of diagnosis:
- Respiratory distress along with suspected tension pneumothorax: Needle decompression
- Respiratory distress or shock along with decreased breath sounds or suspected hemothorax: Tube thoracostomy
- Respiratory distress along with suspected open pneumothorax: Partially occlusive dressing accompanied by tube thoracostomy
- Respiratory distress along with suspected flail chest: Mechanical ventilation
- Shock with suspected cardiac tamponade: Pericardiocentesis
- Suspected hypovolemic shock: Fluid resuscitation
Immediate resuscitative thoracotomy can be diagnosed for Injury victims if the clinician is skillful in the method and the patient has one of the following indications:
- Penetrating thoracic injury along with a need for cardiopulmonary resuscitation (CPR) of < 15 minutes
- Penetrating nonthoracic trauma along with a need for CPR of < 5 minutes
- Blunt trauma along with a requirement for CPR of < 10 minutes
- Persistent systolic blood pressure of < 60 mm Hg because of suspected cardiac tamponade, hemorrhage, or air embolism
Prognosis
- The prognosis for thoracic injury can differ widely, given that thoracic injuries can range from simple rib fractures to pneumothoraces to direct penetrating cardiac injuries. Ultimately the degree and mechanism of injury combined with the patient’s underlying comorbidities decide the prognosis of a patient who has suffered the thoracic injury.
Complications
The chances of a major complication can range from minimal for simple rib fractures to most likely if a major intervention is needed or the degree of injury is significant. Given the number of vital structures in the chest, complications can frequently be significant, involving damage to the vagus or phrenic nerves, the thoracic duct, or critical vascular structures with concomitant complications arising. The degree and mechanism of injury and the interventions taken to address them ultimately decide the type and severity of complications that might arise.
FAQs
Serious thoracic injuries are airway obstruction, tension pneumothorax, cardiac tamponade, open pneumothorax, massive hemothorax, and flail chest are immediate, life-threatening injuries that need evaluation and treatment during the primary survey.
The most important chest injuries involve the following:
Aortic disruption. Signs may involve asymmetric pulses or blood pressure, and decreased blood flow to the lower extremities.
Blunt cardiac injury,
Cardiac tamponade,
Flail chest,
Hemothorax,
Pneumothorax (traumatic pneumothorax),
Pulmonary contusion.
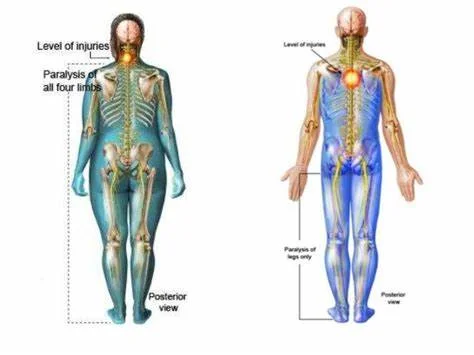
Vertebral compression fractures (VCFs) are the most usual injury to the thoracic spine. They occur when a vertebra in your spine collapses, which can lead to acute pain, deformity, and loss of height.
The most usual condition related to a thoracic spine injury is paraplegia or loss of motor function and sensation in the lower body. A thoracic spinal cord injury cause paralysis in the legs.
People with spinal cord injuries might experience a loss of function around the body. This loss of function can be permanent. Still, A few people do make a complete recovery. Spinal cord injuries can cause secondary conditions, like pressure sores and blood clots.
Early Postoperative Complications
Pulmonary Edema,
Bronchopleural Fistula,
Empyema,
ARDS and Acute Lung Injury,
Pneumonia,
Cardiac Herniation,
Other Early Complications.
Your recovery can take between 6 and 12 weeks depending on the type of operation you have had. The surgical team will be able to advise the likely length of recovery for your particular operation. You might feel tired and experience further discomfort when you get home.
Section 1: Mobility Exercises
Wall Rotations. To do this exercise: set yourself in a deep lung position with the back leg bent with the knee on the floor and resting on the wall,
Kneeling Rotations,
Rolled towel extension,
Preacher Position,
Side Lying Rotation.