Trapezium Fracture
Table of Contents
Introduction
A trapezium fracture refers to a break or fracture in the trapezium bone, which is one of the small bones in the wrist located at the base of the thumb. The trapezium bone plays a crucial role in the movement and stability of the thumb joint.
Fractures of the trapezium bone can occur due to various reasons, including falls on an outstretched hand, direct impact or trauma to the wrist, or repetitive stress on the bone. These fractures can range from hairline cracks to complete breaks, and the severity of the fracture will determine the treatment approach.
Trapezium fractures are very uncommon trauma that must not be ignored.
An isolated fracture of the trapezium is a not common injury accounting for only three to five percent of all carpal fractures. Regardless, they are very critical fractures to detect and treat initially given the significance of the trapezium in the carpometacarpal joint in actions for example grip and pinch. It is commonly a consequence of a high-impact trauma and can be typed into ridge and body fractures. Most are usually vertical body split fractures. Sometimes there can also be correlated ligament damage (anterior oblique ligament, dorsomedial ligament, intermetacarpal ligament, posterior oblique ligament).
Various techniques have been represented in the literature for the management of this rare fracture, from conservative management in plaster to open reduction and internal fixation Depending on the fracture’s displacement and the involvement of the carpometacarpal joint, its clinical presentation can vary radically differently. We document a case of a fracture of the trapezium with associated dislocation of the first carpometacarpal joint which was managed with closed manipulation under anesthesia and percutaneous Kirschner-wire insertion with a pleasing functional consequence at six months follow-up.
Cause of Trapezium Fracture
A fracture typically happens during participation in contact games. It happens when the hand is turned dorsally and forced toward the ulna, causing wrist hyperextension. They frequently happen as a consequence of a high-impact trauma and commonly affect either direct or indirect axial loading. These are the most common transverse loading injuries that occur when a thumb is abducted and the first metacarpal is positioned in the trapezium.
Direct contact with the volar surface, dorsomedial impaction, or an avulsion injury can all result in trapezial ridge fractures. Trapezial body fractures are primarily a consequence of axial stress or shearing through the first carpometacarpal joint.
Symptoms of Trapezium Fracture
- A fracture of the carpal bones of the wrist can present with swelling and bruising.
- There will commonly be tenderness to palpation on the involved bone.
- The range of movement can be reduced. The pain aggravates any kind of gripping activity.
- Tenderness exists over the base of the thumb
- Ecchymosis
- Trapezial ridge fractures can exist with more modest”achy” pain on the anterior base of the thumb
Trapezium Fracture Classification
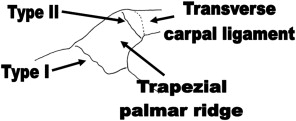
Body and ridge fractures are subcategories of trapezium fractures. The transverse carpal ligament (TCL) spreads radially from the anterior trapezial ridge. Type I and Type II ridge fractures are situated at the base and tip, correspondingly.
- Type I fractures are caused by a direct palmar hit.
- Type II avulsion fractures are reason by a sudden tension force applied to the TCL.
Body fractures happen as either vertical intra-articular, horizontal, posterior radial tuberosity, or comminuted patterns. Concomitant fracture of the first metacarpal is standard. A tuberosity fracture happens with hyperextension-abduction of the thumb, wedging the trapezium between the first metacarpal and the radial styloid. Horizontal fractures, caused by a horizontal shear load, are not very common.
Differential Diagnosis
- Triquetrum fracture
- Pisiform fracture
- Bennett fracture
- Metacarpal fractures
Diagnosis and Pathology
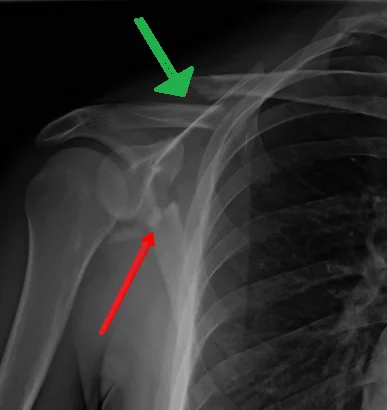
The trapezium is situated in the lower carpal row. It communicates proximally with the scaphoid and distally with the metacarpal of the thumb, where it creates a highly movable tapeziometacarpal or thumb CMC joint. Trapezium fractures account for three to five percent of all carpal fractures. Fractures of this bone happen most typically with a fall on a hyperextended and radially turned wrist with the thumb in the abduction position. Clinically, there is point tenderness present at the base of the thumb. Resisted wrist flexion movement will generally worsen the pain, and there may be correlated carpal tunnel syndrome.
Trapezium fractures, with or without other related injuries, are an uncommon but critical diagnosis. The cause of injury commonly involves either direct dorsomedial impaction or indirect axial loading. Though there are distinct kinds and patterns of fracture like ridge, body, vertical, transverse, and comminuted, the indirect force reason has been attributed to fractures of the body of the trapezium.
Depending on the fracture’s displacement and the involvement of the carpometacarpal joint, its clinical appearance may be drastically altered. Many patients just complain of slight pain at the base of the thumb in the absence of any significant swelling or deformity, whereas others, as in this case report, have swelling and painful restriction of movement. Thus, it is essential to have a high clinical suspicion based on the history and cause of injury. Imaging for this injury consists of plain radiographs, but frequently undisplaced fractures can be missed. With the hand in complete pronation, Robert’s AP view is a valuable way of imagining the trapezium on plain radiographs.
If the diagnosis is always in the query Computerised Tomography or bone scintigraphy is advised. It is necessary to determine the stability of the joint before treatment. Particularly in conditions with related dislocation, rupture of the nearby ligaments and the dorsal joint capsule can cause instability even if the fracture itself is appropriately stabilized and these may need repair. Reconstruction of the inter-metacarpal and capsular structures, for example, an inter-metacarpal abductor pollicis longus augmentation, as expressed by Brunelli et al may be needed, particularly in isolated dislocations. This can not be needed for fracture subluxations, where the metacarpal base and posterior trapezial fragment remain attached by the posterior capsule. A temporary additional stabilizing Kirschner wire will provide inter-metacarpal orientation and association.
Treatment of Trapezium Fracture
Treatment options for trapezium fractures depend on the type and severity of the fracture. For less severe fractures, non-surgical treatments may be sufficient. These can include immobilization with a splint or cast, pain management, and physical therapy to restore hand and thumb function.
This trauma can be managed in a volar splint of the wrist. Frequently this trauma can be managed definitively with cast immobilization. In the condition of symptomatic nonunions and fractures related to ulnar nerve complication, excision of the hook is suitable. Patients with ulnar nerve motor deficiencies may need urgent operative management.
The literature reports several management alternatives. Still, as it is the globally accepted orthopedic principle that fractures affecting an articular surface need accurate reduction, most authors adhere to management concerning the proper restoration of the articular surface. This is reinforced by two series which emphasized the demand for appropriate reduction of the articular surface with displacement more than 2 mm. One article reported successful conservative management of most nondisplaced trapezium fractures in a plaster cast simply. Regardless, another article presented dismal consequences in three patients with comminuted fractures managed in this manner.
Much of the literature proposes open reduction and internal fixation of vertically displaced intraarticular fractures of the trapezium as in this condition. Corey and Ferrer-Torrells were the first to suggest this and they operated Kirschner wire-fixation for a series of five patients. This or closed reduction and pinning, similar to what was done in this particular instance, was suggested by Foster and Hastings. Inston et al expressed the use of a Herbert screw which provided dynamic compression of the fragments and he documented very satisfactory success. Tolat and Jones documented a case of a trapezium fracture with related carpometacarpal dislocation in a skeletally immature 14-year-old who was managed with proper reduction and plaster and made satisfactory healing suggesting that proper reduction or fixation of the trapezium can be sufficient to stabilize the trapezia-metacarpal joint.
Lately, arthroscopic assisted fixation of this injury was conveyed. No studies have compared the consequence of Kirschner wire-fixation (percutaneous/open) to screw fixation (open) but Mcguigan and Culp looked at eleven patients (largest series) with intra-articular trapezium fractures who had some kind of operative management and documented generally helpful outcomes. Regardless, it is fundamental to note that 5/11 patients in this analysis showed degenerative changes at the trapeziometacarpal articulation at long-term follow-up (mean 47 months) despite exceptional functional consequences at earlier review. Therefore it is important to demonstrate this important long-term complication to all patients.
Precautions
Be conscious that pain is continually a continuing pain and the possibility of refracture still exists with the carpal bones. Thus, restoration of range of motion and strength must be within the patient’s pain tolerance, and aggressive treatment must always be prevented.
Recovery:
Recovery from a trapezium fracture can vary depending on the severity of the injury and the treatment approach. It may involve a period of immobilization, followed by rehabilitation exercises and therapy to regain strength, range of motion, and function in the hand and thumb.
FAQ
An immobilized short thumb spica splint can be used to treat non-displaced trapezium and trapezoid fractures for four to six weeks. Management for a non-displaced isolated capitate fracture comprises immobilization with a short arm thumb spica cast for six to eight weeks.
Trapezial ridge fractures can be a consequence of a direct hit to the base of the ridge (type 1) or avulsion of the transverse carpal ligament from the tip of the ridge. Fractures of the trapezium are not common and usually unnoticed and later diagnosed.
Trapezoid fractures Patients have a complaint of tenderness present at the base of the 2nd metacarpal. They can also complain of pain in the area of the snuffbox. On physical exam, they can have swelling present at the wrist and reduced range of motion of the wrist due to pain.
Patients with trapezoid fractures can complain of point tenderness present at the base of the 2nd metacarpal, pain with range of motion at the 2nd metacarpophalangeal joint, or pain and tenderness located at the anatomic snuffbox. Patients may or may not have posterior wrist swelling and decreased range of movement at the wrist.
The trapezium is an uneven-shaped carpal bone located within the hand. The thumb’s metacarpal bone and the trapezium are next to each other in the lower row of carpal bones. On its ulnar aspect are seen the trapezoid and scaphoid bones.







One Comment