Calcaneal fracture (Lovers Fracture)
Table of Contents
What is a Calcaneal fracture?
A calcaneal fracture, also known as a broken heel bone, is a fracture or break in the calcaneus, which is the largest bone in the foot. Calcaneal fractures usually occur as a result of high-energy injuries, such as falls from heights, motor vehicle accidents, or sports-related trauma.
Definition
A Calcaneal fracture is a heel bone fracture. It is a periodic kind of fracture but has potentially debilitating consequences. Traditionally, a burst fracture of the calcaneus was called a “Lovers Fracture” as the damage would happen as a suitor would jump off a lover’s balcony (axial loading) to prevent detection.
Clinical Anatomy
A better knowledge of the anatomy of the calcaneus is a fundamental element in determining the kind of damage and the kind of therapy strategies and alternatives.
Calcaneus is the biggest talar bone out of seven tarsal bones which together with the talus form the hindfoot. The calcaneus has a comparatively thin cortex. It has 4 facets: 1 anteriorly which articulates with a cuboid forming a calcaneocuboid joint and 3 superiorly (anterior, middle, and posterior, with the posterior facet describing the major weight-bearing surface) which articulate with talus comprising talocalcaneal joint (subtalar joint). The subtalar joint permits inversion and eversion movement of the foot.
The interosseous ligament and medial, lateral, and posterior talocalcaneal ligaments deliver accessory support for the joint. The sustentaculum talus is a medial bony projection keeping the neck of the talus. The tibial artery, nerve, posterior tibial tendon, and flexor hallucis longus tendon are situated medially to the calcaneus and are at threat for impingement with a calcaneal fracture, as are the peroneal tendons situated on the outer side of the calcaneus. This also creates the surgical procedure challenging. The lateral aspect of the calcaneus and due to its flat nature is emphasized as the most practical for internal fixation, but the impractical soft tissue surface challenges wound recovery. These anatomic landmarks are significant due to fractures associated with these areas may cause involve joint involvement, tendon, and neurovascular injury.
The calcaneus has four important functions:
- Acts as a basis and support for the body’s weight
- Keeps the lateral column of the foot and acts as the main articulation for inversion and eversion
- Shows as a lever arm for the gastrocnemius muscle complex
- Makes normal walking potential
Cause of Calcaneal fracture
- Calcaneal fractures comprise 1-2 percent of all fractures and 60 percent of tarsal fractures.
- Less than 10 percent present as open fractures.
- Earlier, calcaneum fracture was predominately in males as they used to do more industrial work. But current studies recommend a regional variation in male and female predominance.
- Calcaneal fractures are infrequent in youngsters. In those 8-14 years old, 60 percent of calcaneal fractures are extra-articular. This number raised to 90 percent for those under 7 years old.
- 20-25 percent of calcaneal fractures are correlated to compression fractures of the vertebrae of the lumbar.
- Several patients with calcaneus fractures are young, with the 20 to 39 age level being the most typical.
- Osteoporosis, diabetes mellitus, peripheral neuropathy, osteomalacia, and long-term immunosuppressive treatment are the risk factor.
Mechanism of Injury
- Calcaneal fractures are mostly the cause of high-impact events leading to axial loading of the bone.
- Especially, falls from distant and road traffic accidents (such as a foot depressed in front of an accelerator, brake, or floorboard) are classic modes of injury. The talus function as a wedge resulting in depression and therefore flattens, broadens, and compresses the calcaneal body.
- Calcaneal fractures can even happen with less painful accidents like an ankle sprain or a stress fracture in the athlete.
- Jumping into firm surfaces, sharp or piercing trauma, and twisting or shearing possibilities may happen resulting in calcaneus fracture.
- Especially, injuries that happen in isolation. Considerable seen concomitant injuries were lower extremity (13.2 percent) or spinal injuries (6.3 percent).
- The posterior tibial neurovascular bundle passes along the medial side of the calcaneal body and is shielded by the sustentaculum tali consequently neurovascular trauma is not common with calcaneal fractures.
Symptoms of Calcaneal fracture
Firstly, a patient may present with an above-mentioned traumatic event with the following clinical features:
- Patients will complain of diffuse pain, edema, and ecchymosis at the involved fracture place.
- The patient is not possibly capable to take the weight, walk, and move the foot.
- Swelling in the heel region
- Plantar ecchymosis spreading through the plantar arch of the foot must increase suspicion significantly.
- There can be correlated impairment of the Achilles tendon.
- Skin quality about the heel should be considered for tenting and threatened skin. This is particularly significant in the setting of Tongue-kind calcaneus fractures.
- Overall unlocalized pain in the heel region that mainly progresses slowly (over several days to weeks) – most regularly with stress fractures
- Deformity of the heel or plantar arch: Secondary to the displacement of the lateral calcaneal edge exterior, there is a potential widening or broadening of the heel.
Classification of Calcaneal fracture
The calcaneus, also called the heel bone, is the biggest of the tarsal bones and articulates with the cuboid bone and the talus bone superiorly. It is responsible for transmitting the majority of the body’s load from the talus bone to the ground.
Calcaneal fractures are classified as intra-articular or extra-articular on the cause of subtalar joint involvement. Intra-articular fractures are very general and possess the dorsal talar articular facet of the calcaneus. The Sanders classification groups these fractures into four types depending upon the site of the fracture at the dorsal articular surface. Extra-articular fractures are less ordinary and can be placed in any place outside the subtalar joint. Extra-articular fractures are categorized depending on whether the involvement of the calcaneus is anteriorly (Type A), middle (Type B), or dorsally (Type C).
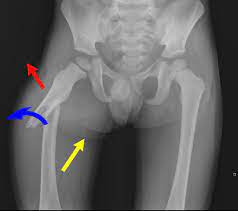
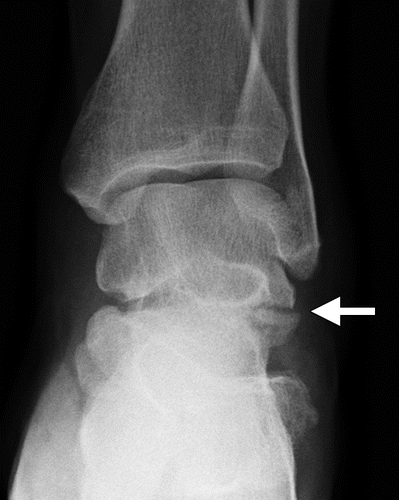
The Angle of Gissane, or “Critical Angle”, is the angle created by the downward and upward inclines of the calcaneal superior surface. On a lateral X-ray, an angle of Gissane more than 130 degrees advises fracture of the posterior subtalar joint surface. Böhler’s angle, or the “Tuber Angle”, is another normal anatomic position found in lateral X-ray. It is formed by the intersection of 1) a line from the highest end of the posterior articular facet to the highest end of the posterior tuberosity, and 2) a line from the former to the highest end of the anterior articular facet. Böhler’s angle is usually twenty-five degrees to forty degrees. It is called after Austrian physician Lorenz Böhler. A decreased angle is signifying a calcaneal fracture.
The Sanders classification system is the most usually utilized system for categorizing intra-articular fractures. There are 4 kinds:
- Type I fractures are non-displaced fractures (displacement more than 2 mm).
- Type II fractures comprise a single intra-articular fracture that separates the calcaneus into 2 segments.
- Type IIA: Fractures happen on the lateral side of the calcaneus.
- Type IIB: fracture happens on a central aspect of the calcaneus.
- Type IIC: fracture happens on the medial aspect of the calcaneus.
- Type III fractures consist of two intra-articular fractures that separate the calcaneus into 3 particular segments.
- Type IIIAB: two fracture lines exist, one lateral and one central.
- Type IIIAC: two fracture lines exist, one lateral and one medial.
- Type IIIBC: two fracture lines exist, one central and one medial.
- Type IV fractures comprise fractures with greater than three intra-articular fractures.
Extra-articular fractures contain all fractures that do not affect the dorsal facet of the subtalar joint.
- Type A involve the anterior calcaneus
- Type B involve the middle calcaneus. This possesses the sustentaculum tali, trochlear process, and lateral process.
- Type C involves the dorsal calcaneus, the dorsal tuberosity, and the medial tubercle possessed.
Examination
- Palpation: Tenderness over calcaneus while pressing the heel from both sides. A compression test is positive for a stress fracture of the calcaneus.
- A detailed neurovascular assessment is necessary. The pulse rate of the same side of the dorsal pedis or posterior tibial can approximate the opposite good extremity. If there is any doubt of arterial injury, additional investigation with angiography or Doppler scanning can be performed.
- Assessment of all lower extremity tendon function is also required.
- Assessment of spine fracture as a correlated fracture of calcaneus from axial loading.
Diagnostic Procedures
Radiological examination:
X-ray: AP, lateral, and oblique lines drawn of the foot bone and ankle are required. A Harris view can be accepted which reveals the calcaneus in an axial direction.
- Axial -Determines direct fracture line and indicates the body, tuberosity, and central and posterior facets.
- Lateral – Determines Bohler angle.
- Oblique or Broden’s view – This shows the degree of displacement of the preliminary fracture line.
CT scan: It is the first choice for traumatic calcaneal damage.
Bone scan or MRI: are suggested in a stress fracture of the calcaneus.
- Mondor’s Sign is a hematoma or contusion identified on computed tomography that extends across the sole and is regarded as pathognomic for calcaneal fracture.
- Bohler’s Angle is described as the angle between two lines marked on plain film. The first line connects the peak on the tuberosity to the peak on the posterior facet, while the second connects the peak on the anterior process to the peak on the dorsal facet. The standard angle is between 20-40 degrees. It can be pushed on plain radiographs if it’s a calcaneus fracture.
- The Critical Angle of Gissane is represented as the angle between two lines marked on plain film. The first is along the anterior downward incline of the calcaneus and the second is across the superior upward slope. A standard angle is 130 to 145 degrees. It can be an increase in calcaneus fracture.
Treatment of Calcaneal fracture
There is no one treatment or surgical method for all calcaneal fractures. Treatment of calcaneal fractures relies on the particular fracture pathoanatomy, attending soft-tissue injury, related trauma, functional need, and comorbidities of the patient.
The treatment of calcaneus fractures can be separated into surgical and non-surgical treatments.
Non-Operative Care
Non-surgical management is chosen when there is an absence of impingement of the peroneal tendons and the fracture segments are undisplaced (or are displaced < 2 mm). Nonsurgical care is even suggested when, in spite of the existence of a fracture, appropriate weight-loading alignment has been sufficiently supported, and articulating surfaces are not disturbed. Extra-articular fractures are commonly managed conservatively. Patients who are above the age of 65 years old or who have pre-existing health conditions, for instant diabetes, neurovascular deficit, noncompliance (e.g., drug abuse), and extreme systemic disorders with immunodeficiency and or inadequate general prognosis are too typically managed using nonoperative methods.
RICE protocol for soft tissue conditions can be followed with immobilization in non-surgical management.
Immobilization: A cast, splint, or brace will keep the bones in your foot in the correct place while they recover. A cast needs to wear for 6 to 8 weeks — or maybe longer depending on follow-up radiographic findings. During this time, weight-loading is strictly forbidden.
Operative Care
For the majority of patients with calcaneus fracture, the operation is the indicated treatment. Intraarticular fractures are frequently treated operatively. The objective of the surgical procedure is to rebuild the absolute form of the calcaneum and surfaces of the joint to achieve a satisfactory functional outcome. This is achievable by performing an open reduction and internal fixation of the fracture. There are several methods for performing open reduction and internal fixation. This procedure decreases the possibility of developing arthritis ( post-traumatic subtalar arthritis) and maximizes the possibility of inversion and eversion movement of the foot.
Extraarticular fractures with a significant hindfoot varus or valgus deformity (more than 10 degrees) and those with significant flattening, widening, or shortening of the heel must also be reduced, ideally using a tiny or percutaneous approach. An unsafe extraarticular subtype of a tongue-type fracture with extreme displacement of the superior margin of the calcaneal tuberosity (“beak fracture”) is an operation emergency.
Physical Therapy Treatment
There are many similarities between nonsurgical and surgical physiotherapy treatment of calcaneal fractures. These similarities possess a Time period of immobilization with restricted weight loading, joint mobilization, range of motion exercises, pain management, strengthening, proprioception training, gait training, plyometrics, and slowly gently loading to resume more challenging activities.
These are a few result measures that may be utilized to measure the functional abilities of the patient to find the prognosis which may be used during the rehabilitation time period:
- Lower Extremity Functional Scale (LEFS)
- Foot and Ankle Ability Measure (FAAM)
Pre-Surgery
Early stability is very important for open reduction internal fixation of intraarticular calcaneal fractures.
Presurgical revalidation possesses:
- Immediate elevation of the involved foot to minimize the swelling.
- Compression for example ankle toe movement, intermittent compression devices, or compression wraps is bearable.
- Instructions for using wheelchairs, bed transfers, or crutch walking.
Post-Surgery
Advancement of the non-surgical and post-surgical treatment of calcaneal fractures keeps traditional immobilization and earlier movement rehabilitation protocols. In particular, the standard immobilization protocols of nonsurgical and post-surgical management are comparable and are thereby combined in the progression of the treatment below. Phases II and III of traditional and initial movement rehabilitation protocols afterward to non-surgical or post-surgical care are comparable as well and are defined together below.
Phase I: Weeks 1-4
Goals:
- Minimized edema and pain
- Avoid extension of fracture or loss of surgical stabilization
- Minimize loss of function and cardiovascular endurance
Intervention:
- Cast with the foot in neutral and sometimes little eversion movement
- Elevation
- Toe curl and active ankle joint (dorsiflexion and plantar flexion)-encourage to do from the first postoperative day.
- After 2-4 days, guide the patient in non-weight-bearing ambulation using crutches or walker-crutch walking exercise
- Instruct wheelchair users with an appropriate sitting schedule to limit the time involved extremity spend in dependent-gravity position
- Instruct in comprehensive exercise and cardiovascular schedule using upper limb and good lower limb
- Strengthening adjacent joint musculature (hip and knee)
Phase II: Weeks 5-8
Goals:
- Control remaining or residual edema and pain
- Avoid re-injury or complication of fracture by progressing weight-loading safely
- Avoid contracture and recover movement at ankle or foot joints
- Minimize lack of function and cardiovascular endurance
Intervention:
- Persisted elevation, icing, and compression as required for the affected lower limb.
- After 6 to 8 weeks, instruct in partial-loading ambulation using crutches or a walker
- Initiate strong exercise and range of motion to recover and maintain activity at all joints: tibiotalar, subtalar, mid-tarsal, and toe joints, including active range of motion in large amounts of movement and progressive isometric or resisted exercises
- Improvement and monitor comprehensive upper limb and cardiovascular program
Phase III: Weeks 9-12
Goals:
- Progress weight-bearing status
- Normal gait on all surfaces
- Restore full range of motion
- Restore full strength
- Allow return to previous work status
Intervention:
- After 9-12 weeks, instruct in normal complete-weight bearing ambulation with the suitable assistive device as required
- Improvement and observe the subtalar joint’s capacity to adjust to ambulation on all surfaces, involving graded and irregular surfaces
- Joint mobilization to all hypermobile joints containing tibiotalar, subtalar, midtarsal, and to-toe joints
- Soft tissue mobilization to hypermobile tissues of the gastrocnemius complex, plantar fascia, or other appropriate tissues
- Progressive resisted strengthening of gastrocnemius complex via the help of pulleys, weighted exercise, toe-walking ambulation, climbing or descending stairs, skipping or another plyometric activity, aquatic therapy, and additional climbing activities
- Work hardening program or activities to permit the return to work between 13 to 52 weeks
FAQ
If your injury is minor, for example, a crack in the bone with a slight muscle tear, you can be capable to return to normal activities 3 to 4 months after the operation. If your fracture is intense, yet, it can take 1 to 2 years before recovery is absolute.
While your cracked calcaneus is recovering, you will not be capable to take the load on your feet. You will probably be immobilized in a well-padded splint. Occasionally physical therapy is advisable to assist with motion and weight-bearing once the bone recovers.
Wound necrosis is the most repeatedly followed postoperative complication in calcaneal fractures, which is noticed in up to 14 percent of cases after traditional osteosynthesis through an extended lateral technique and up to 27 percent with a bilateral procedure.
Pain is generally painful sufficiently to need an emergency room stay. If the fracture is caused by a stress fracture, over the period, then symptoms may be distant and more unclear. There may be some pain, increasing throughout the day, usually described as being dull and achy. Bruising may or may not exist.
Clinical sequences with greater than 100 patients and followed for greater than 1 year demonstrated satisfactory to excellent results with open reduction and lateral plate fixation in 60 percent to 85 percent of cases using various outcome criteria.





3 Comments