Calcaneus Bone
Table of Contents
Introductions
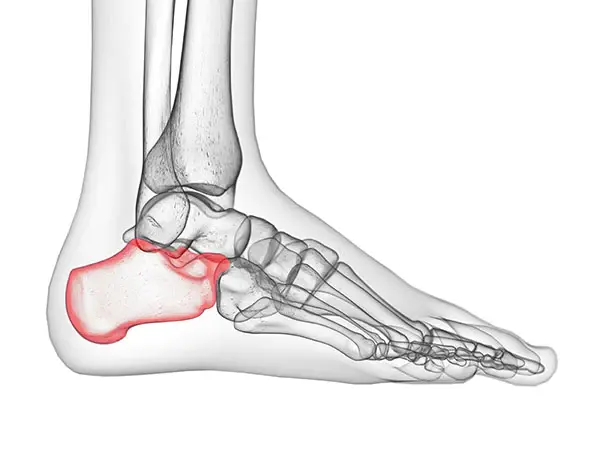
The calcaneus bone, also known as the heel bone, is a large and unique bone located at the back of the foot. It is the largest bone in the foot and plays a crucial role in supporting body weight and transmitting forces during walking, running, and jumping.
Anatomy of Balcaneus Bone
The anatomy of the calcaneus bone can be described in detail as follows:
- Body: The body of the calcaneus forms the majority of the bone and provides a stable base for the foot. It has a convex shape on its superior surface, which articulates with the talus bone to form the subtalar joint. The body of the calcaneus also has a concave shape on its inferior surface, which helps to distribute forces evenly across the foot.
- Sustentaculum Tali: This is a bony prominence on the medial side (inner side) of the calcaneus. It supports the talus bone, which sits above it, and helps maintain the stability of the foot. The sustentaculum tali acts as a shelf for the talus bone to rest upon.
- Tuberosity: The posterior part of the calcaneus has a large, roughened area called the tuberosity. This serves as an attachment site for several muscles, tendons, and ligaments involved in foot movement and stability. The tuberosity provides leverage for these structures and helps in movements such as plantarflexion (pointing the toes downward).
- Calcaneal Tubercle: Located at the bottom of the tuberosity, the calcaneal tubercle provides attachment for the Achilles tendon. The Achilles tendon connects the calf muscles to the heel bone and is responsible for movements such as plantarflexion and propulsion during walking or running.
In addition to these prominent features, the calcaneus bone also has various other structures such as articular facets, grooves for tendons, and bony processes. These structures provide attachment sites for muscles, tendons, and ligaments that contribute to the stability and mobility of the foot.
The calcaneus bone works in conjunction with other bones in the foot, such as the talus bone and cuboid bone, to support body weight and facilitate movements. It acts as a lever arm for various muscles and tendons involved in foot movement and provides stability to the foot through its articulations with other bones.
Understanding the detailed anatomy of the calcaneus bone is important for diagnosing and treating injuries or conditions that may affect this bone. Fractures, Achilles tendonitis, plantar fasciitis, and heel spurs are some examples of conditions that can affect the calcaneus bone. Treatment for these conditions may involve rest, physical therapy, orthotics, pain management, and in severe cases, surgery. It is important to seek medical advice if you experience persistent heel pain or have concerns about your foot health.
Functions of Calcaneus Bone
The calcaneus bone, or heel bone, plays several crucial functions in the foot. These functions can be explained in detail as follows:
- Support: The calcaneus bone is the largest bone in the foot and provides a stable base for the foot to bear the weight of the body. It helps distribute body weight evenly across the foot, allowing for efficient walking, running, and jumping.
- Shock absorption: The calcaneus bone acts as a shock absorber, cushioning the impact of the foot hitting the ground during activities such as walking or running. Its unique shape and structure help to absorb and dissipate forces, reducing stress on other structures of the foot.
- Lever arm: The calcaneus bone acts as a lever arm for various muscles and tendons involved in foot movement. For example, the Achilles tendon attaches to the calcaneal tubercle, and when it contracts, it causes plantarflexion (pointing the toes downward). This movement is essential for walking, running, and propelling the body forward.
- Stability: The calcaneus bone plays a crucial role in maintaining the stability of the foot. It articulates with the talus bone to form the subtalar joint, which allows for inversion (turning the sole of the foot inward) and eversion (turning the sole of the foot outward) movements. These movements are important for maintaining balance and stability while walking on uneven surfaces.
- Muscle and tendon attachment: The calcaneus bone provides attachment sites for various muscles, tendons, and ligaments involved in foot movement and stability. These structures include the Achilles tendon, which attaches to the calcaneal tubercle, as well as other tendons and ligaments that help support and control foot movements.
Overall, the calcaneus bone is essential for supporting body weight, absorbing shock, facilitating foot movements, maintaining stability, and providing attachment sites for important structures involved in foot function. Understanding the functions of the calcaneus bone is crucial for diagnosing and treating conditions that may affect this bone and ensuring proper foot health.
Muscle attachment
The calcaneus bone provides attachment sites for various muscles, tendons, and ligaments involved in foot movement and stability. These structures play a crucial role in controlling the movements of the foot and maintaining its stability.
One of the most important muscle attachments to the calcaneus bone is the Achilles tendon. The Achilles tendon is the largest and strongest tendon in the body, and it attaches to the posterior aspect of the calcaneal tubercle. This tendon is formed by the fusion of the gastrocnemius and soleus muscles in the calf. When these muscles contract, they cause plantarflexion, or the pointing of the toes downward. This movement is important for day-to-day activities such as walking, running, and jumping.
Other muscles that attach to the calcaneus bone include the flexor digitorum longus, flexor hallucis longus, and peroneus brevis. These muscles are located in the lower leg and are responsible for flexing and extending the toes. They attach to the calcaneus bone through their respective tendons, which run along the back of the foot and insert into the base of the distal phalanges of the toes.
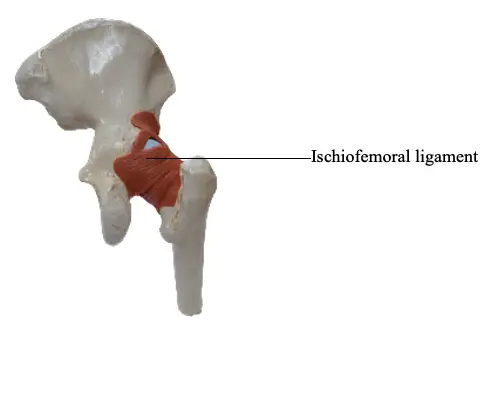
In addition to muscles, several ligaments also attach to the calcaneus bone. These ligaments help provide stability to the foot and control its movements. One example is the plantar fascia, a thick band of connective tissue that runs along the sole of the foot. It attaches to the calcaneus bone at its origin and extends forward to attach to the metatarsal heads. The plantar fascia helps support the arch of the foot and plays a role in shock absorption during weight-bearing activities.
Understanding the muscle and tendon attachments to the calcaneus bone is crucial for diagnosing and treating conditions that may affect these structures. Injuries or inflammation of these attachments can lead to pain, limited mobility, and difficulty with activities that involve foot movement. Physical therapists, orthopedic specialists, and other healthcare professionals may use this knowledge to develop treatment plans and rehabilitation exercises to address these issues and restore proper foot function.
Palpation of calcaneus bone
Palpation of the calcaneus bone involves using touch or pressure to assess the structure, position, and condition of the bone. It is commonly performed by healthcare professionals, such as doctors, physical therapists, or chiropractors, to diagnose and evaluate conditions related to the foot and ankle.
Here is a step-by-step guide on how to perform palpation of the calcaneus bone:
- Preparation: Ensure that the patient is in a comfortable position, either sitting or lying down. Make sure there is adequate lighting and access to the foot and ankle area.
- Locate the calcaneus bone: The calcaneus bone is the largest bone in the foot, forming the heel. It is easily identifiable as the prominence at the back of the foot. Gently run your fingers along the back of the foot until you feel a bony prominence. This is the calcaneus bone.
- Positioning: Place your thumb or fingers on the sides of the calcaneus bone, just above the attachment of the Achilles tendon. The Achilles tendon attaches to the posterior aspect of the calcaneus bone.
- Palpation technique: Apply gentle pressure with your thumb or fingers to palpate the calcaneus bone. Start with light pressure and gradually increase if necessary. Move your thumb or fingers in a circular motion or back and forth to feel for any irregularities, tenderness, or pain.
- Assess for tenderness: Ask the patient if they experience any tenderness or pain during palpation. Tenderness may indicate inflammation, injury, or underlying conditions such as plantar fasciitis or Achilles tendonitis.
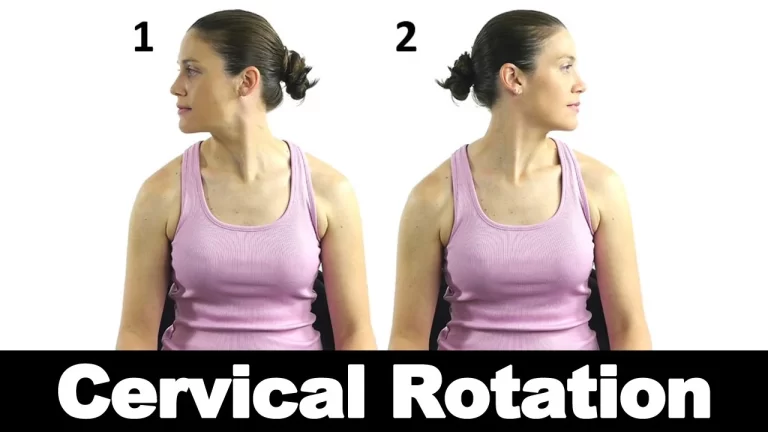
- Evaluate range of motion: While palpating the calcaneus bone, you can also assess the range of motion of the foot and ankle. Ask the patient to move their foot up and down (dorsiflexion and plantarflexion) and side to side (inversion and eversion). Observe for any limitations, stiffness, or discomfort.
- Compare with the other side: It is essential to compare the palpation findings of the calcaneus bone on both feet. This allows for a baseline comparison and helps identify any asymmetries, abnormalities, or discrepancies.
- Documentation: Record your findings, including any tenderness, abnormalities, or limitations in range of motion. This documentation will assist in monitoring progress, tracking changes, and determining appropriate treatment plans.
It is important to note that palpation of the calcaneus bone should be performed by trained healthcare professionals who are familiar with the anatomy and techniques involved. If there is any concern or suspicion of an injury or underlying condition, further diagnostic tests or imaging may be necessary for a comprehensive evaluation.
Blood and Lymph supply
The calcaneus bone, also known as the heel bone, receives its blood supply from several arteries and has lymphatic drainage to ensure proper nourishment and waste removal. Here is a detailed explanation of the blood and lymph supply of the calcaneus bone:
Blood Supply:
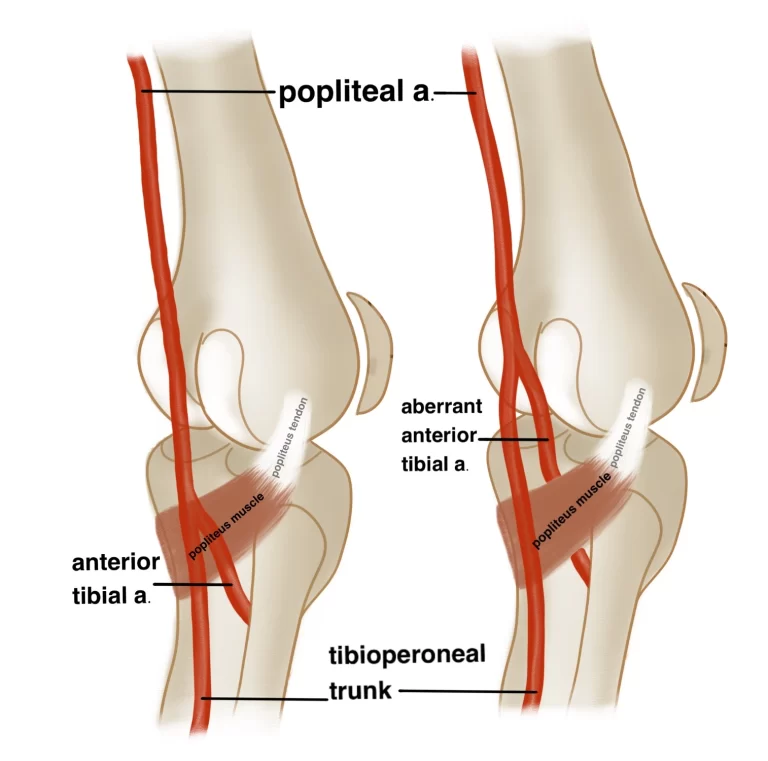
- Medial Calcaneal Artery: This artery arises from the posterior tibial artery, which is a branch of the popliteal artery in the leg. The medial calcaneal artery supplies the medial side of the calcaneus bone, including its sustentaculum tali (a bony prominence that supports the talus bone).
- Lateral Calcaneal Artery: This artery is a branch of the posterior tibial artery or the peroneal artery. It supplies the lateral side of the calcaneus bone, including the lateral tubercle.
- Perforating Branches: These small branches arise from nearby arteries, such as the peroneal artery or the lateral malleolar artery. They penetrate the soft tissues and reach the calcaneus bone to provide additional blood supply.
- Arteries of the Sinus Tarsi: The sinus tarsi is a small cavity located between the talus bone and calcaneus bone. It contains several arteries that contribute to the blood supply of the calcaneus bone.
Lymphatic Drainage:
The lymphatic vessels in the foot and ankle region help drain excess fluid, waste products, and immune cells from the calcaneus bone. The lymphatic drainage of the calcaneus bone follows a pattern similar to its blood supply:
- Medial Calcaneal Lymph Nodes: Lymphatic vessels from the medial side of the calcaneus bone drain into the medial calcaneal lymph nodes. These nodes are located near the Achilles tendon, close to where it attaches to the posterior aspect of the calcaneus bone.
- Lateral Calcaneal Lymph Nodes: Lymphatic vessels from the lateral side of the calcaneus bone drain into the lateral calcaneal lymph nodes. These nodes are located in the subcutaneous tissue on the lateral aspect of the foot.
- Popliteal Lymph Nodes: Some lymphatic vessels from the calcaneus bone may also drain into the popliteal lymph nodes, which are located in the popliteal fossa behind the knee.
From these regional lymph nodes, lymphatic fluid eventually flows into larger lymphatic vessels and eventually reaches the lymphatic system’s main drainage points.
Understanding the blood and lymph supply of the calcaneus bone is crucial for healthcare professionals when evaluating and treating conditions related to the foot and ankle. It helps ensure proper healing, identify potential complications, and guide treatment decisions.
Conditions that affect Calcaneus Bone
There are several conditions that can affect the calcaneus bone. Here are some of the most common associated conditions:

Calcaneal Fractures: Fractures of the calcaneus bone are typically caused by high-energy trauma, such as a fall from a height or a car accident. These fractures can be complex and may involve multiple fragments. Treatment usually involves immobilization, pain management, and sometimes surgical intervention.
Plantar Fasciitis: This condition includes inflammation of the plantar fascia, a thick band of tissue that runs along the base of the foot and connects to the calcaneus bone. It is sometimes known as heel pain, especially in the morning or after long periods of rest. Treatment options include stretching exercises, orthotics, physical therapy, and in severe cases, corticosteroid injections or surgery.
Achilles Tendonitis: The Achilles tendon attaches the calf muscles to the calcaneus bone. Tendonitis refers to inflammation of the tendon, which can cause pain and stiffness in the back of the heel. Treatment involves rest, physical therapy, stretching exercises, orthotics, and sometimes corticosteroid injections.
Haglund’s Deformity: This condition is characterized by a bony enlargement on the back of the calcaneus bone, near where the Achilles tendon attaches. It is often associated with pressure and friction from footwear, leading to pain and inflammation. Treatment may include shoe modifications, padding, orthotics, physical therapy, and in some cases, surgical removal of the bony prominence.
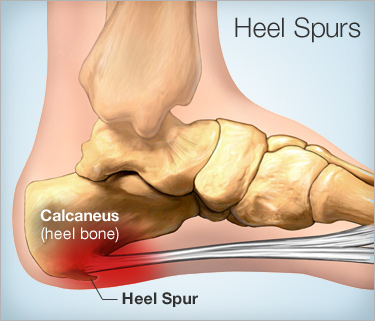
Calcaneal Spurs: These are bony outgrowths that develop on the underside of the calcaneus bone. They are often associated with plantar fasciitis or other conditions that cause chronic inflammation in the foot. Treatment focuses on managing the underlying condition and may include stretching exercises, orthotics, physical therapy, and occasionally surgery.
Osteomyelitis: This is a bone infection that can affect the calcaneus bone. It is usually caused by bacteria entering the bone through an open wound or as a complication of previous surgery. Treatment involves antibiotics, surgical debridement (removal of infected tissue), and sometimes bone grafting.
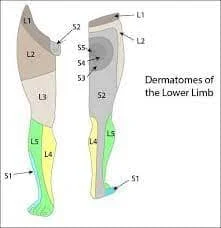
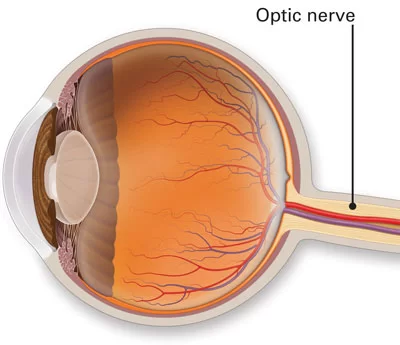
Tarsal Tunnel Syndrome: This condition involves compression of the tibial nerve as it passes through a narrow tunnel in the ankle, called the tarsal tunnel. It can cause pain, numbness, and tingling in the heel and foot. Treatment may include rest, orthotics, physical therapy, corticosteroid injections, and in severe cases, surgery to decompress the nerve.
It is important to note that these are just a few examples of conditions that can affect the calcaneus bone. There are many other potential disorders and injuries that can impact this bone, and proper diagnosis and treatment should be sought by a healthcare professional.
Rehabilitation of Calcaneus Bone
The rehabilitation of calcaneus bone conditions depends on the specific condition and severity of the injury. Here is a general overview of the rehabilitation process for some common calcaneus bone conditions:
- Calcaneal Fractures: After immobilization or surgical intervention, rehabilitation typically begins with non-weight-bearing exercises to maintain joint mobility and prevent muscle atrophy. As healing progresses, weight-bearing exercises and gait training are introduced under the guidance of a physical therapist. The focus is on restoring range of motion, strength, and balance. Gradually, functional activities such as walking and running are incorporated into the rehabilitation program.
- Plantar Fasciitis: Rehabilitation for plantar fasciitis usually involves a combination of stretching exercises, strengthening exercises, and orthotic management. Physical therapy may include manual therapy techniques to improve tissue flexibility and reduce pain. A gradual return to weight-bearing activities is emphasized, along with modifications to footwear and activity levels to prevent recurrence.
- Achilles Tendonitis: Rehabilitation for Achilles tendonitis aims to reduce pain, and inflammation, and improve tendon strength and flexibility. Treatment may involve eccentric strengthening exercises, stretching exercises, and modalities such as ultrasound or laser therapy. Physical therapy can also help address any biomechanical factors contributing to the condition. Gradual progression of activity is important to avoid re-injury.
- Haglund’s Deformity: Rehabilitation for Haglund’s deformity focuses on reducing pain and inflammation, improving flexibility, and addressing any underlying biomechanical issues. Treatment may include stretching exercises, physical therapy modalities (such as ice or ultrasound), shoe modifications, and orthotics. In some cases, surgical intervention may be necessary to remove the bony prominence, followed by a period of immobilization and rehabilitation.
- Heel Spurs: Rehabilitation for calcaneal spurs primarily involves managing the underlying condition causing chronic inflammation, such as plantar fasciitis. Treatment may include stretching exercises, orthotics, physical therapy modalities, and activity modification. Surgical intervention is typically not necessary for calcaneal spurs unless conservative measures fail.
- Osteomyelitis: Rehabilitation for osteomyelitis of the calcaneus bone focuses on treating the infection and promoting bone healing. This usually involves a combination of antibiotic therapy, surgical debridement to remove infected tissue, and possibly bone grafting. Rehabilitation may include a range of motion exercises, weight-bearing activities as tolerated, and physical therapy to restore strength and function.
- Tarsal Tunnel Syndrome: Rehabilitation for tarsal tunnel syndrome aims to relieve compression of the tibial nerve and reduce pain and numbness. Treatment may involve rest, orthotics, physical therapy modalities (such as ultrasound or electrical stimulation), and stretching exercises. In severe cases, surgical decompression of the tarsal tunnel may be necessary, followed by a period of immobilization and rehabilitation.
It is important to note that rehabilitation programs should be individualized based on the specific condition, severity, and the patient’s goals and needs. A healthcare professional, such as a physical therapist or orthopedic specialist, can provide a comprehensive evaluation and develop a tailored rehabilitation plan.
FAQs
The duration of rehabilitation for calcaneus bone conditions can vary depending on the specific condition and severity of the injury. It can take time from some weeks to many months.
In many cases, rehabilitation plays a crucial role in the treatment of calcaneus bone conditions. However, some severe cases may require surgical intervention in addition to rehabilitation.
Rehabilitation can help address underlying biomechanical issues and strengthen the affected area, which may reduce the risk of recurrence. However, it is important to follow proper preventive measures and continue with any recommended exercises or modifications even after rehabilitation is completed.
Overuse or improper footwear can contribute to the development of certain calcaneus bone conditions such as plantar fasciitis, Achilles tendonitis, and Haglund’s deformity. It is important to wear appropriate footwear and avoid activities that put excessive strain on the heel.


8 Comments