Plantar Fasciitis
Table of Contents
What is Planter Fasciitis?
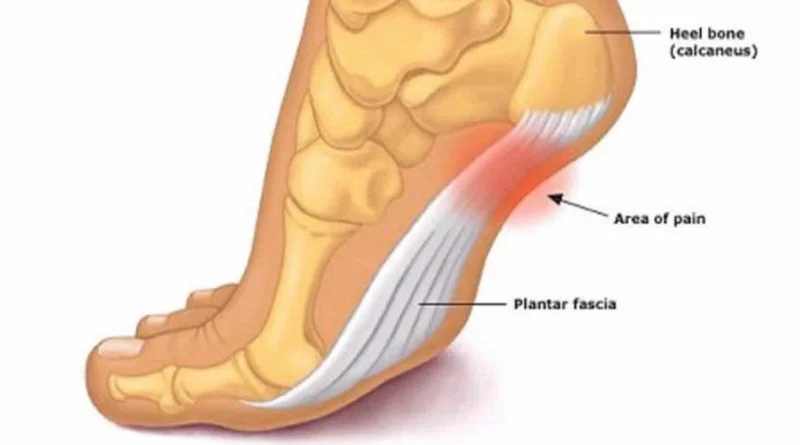
Plantar fasciitis is a disorder of the connective tissue which supports the arch of the foot. It results in pain in the heel and bottom of the foot that is usually most severe with the first steps of the day or following a period of rest.
Pain is also frequently brought on by bending the foot and toes up towards the shin. The pain typically comes on gradually, and it affects both feet in about one-third of cases.
Plantar Fascia Anatomr
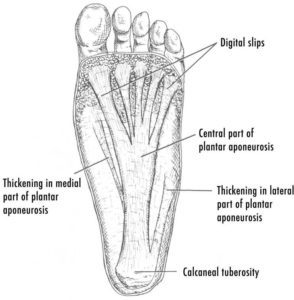
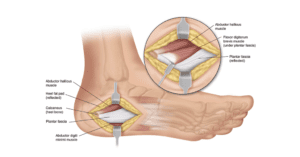
The plantar fascia is the fibrous tissue layer on the plantar surface of the foot that connects the heel bone to the toes. It supports the arch of the foot and protects the sole from injuries.
It is a thick white band of longitudinally extended collagen fibers. It originates posteriorly from the medial process of the tuberosity of calcaneus (heel bone). As it extends towards the toes, it divides into five separate bands that extend to the proximal phalanges (bones of the toes, closest to the foot).
The superficial layer of plantar fascia embeds into the skin fold between the sole and the toes.
The deeper layer extends to embrace the digital flexor tendons on each proximal phalanx.
The plantar fascia can be divided into three distinct parts:
- The medial part
- The central part
- The lateral part
The central part is the thickest and the largest part running between the relatively thinner and less prominent medial and lateral parts.
In young adults, the plantar fascia is also attached to the Achilles tendon or the Calcaneal tendon, which is the tendinous extension of lower leg muscles (the calf muscle). It passes behind the ankle and gets attached to the posterior surface of the heel bone (calcaneum). As these two anatomical structures have separate specific attachments on the heel bone, therefore, these do not affect each other directly. However, the upward movement of the toes tightens the Achilles tendon indirectly. This connection is used for the treatment of plantar fasciitis (painful inflammation of plantar fascia).
Pathophysiology
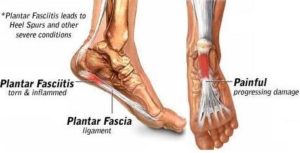
The plantar fascia is a thick fibrous band of connective tissue originating from the medial process of the calcaneal tuberosity. It extends towards the forefoot and inserts at each of the proximal phalanges.
Current theory suggests micro-tears to the plantar fascia occur, suggesting a chronic breakdown of the structure, rather than being solely due to an inflammatory process Individuals may be predisposed to the condition from the anatomical structure of the foot.
During the gait cycle, the hallux is dorsiflexed and the plantar fascia is forced to shorten and elevate the medial longitudinal arch; any anatomical abnormality to the foot can result in an asymmetric loading on the plantar fascia – leading to chronic repeated damage.
Causes of Plantar Fasciitis:
Plantar fasciitis is most commonly caused by repetitive strain injury to the ligament of the sole of the foot. Such strain injury can be from excessive running or walking, inadequate foot gear, and jumping injury from landing. Plantar fasciitis can also be caused by certain diseases, including reactive arthritis and ankylosing spondylitis.
Risk factors
>Age:- Plantar fasciitis is most common between the ages of 40 and 60.
>Certain types of exercise:- Activities that place a lot of stress on your heel and attached tissue — such as long-distance running, ballistic jumping activities, ballet dancing, and aerobic dance — can contribute to an earlier onset of plantar fasciitis.
>Foot mechanics:- Being flat-footed, having a high arch, or even having an abnormal pattern of walking can affect the way weight is distributed when you’re standing and put added stress on the plantar fascia.
>Obesity:- Excess pounds put extra stress on your plantar fascia.
>Occupations that keep you on your feet:- Factory workers, teachers, and others who spend most of their work hours walking or standing on hard surfaces can damage their plantar fascia.
Sign & Symptoms

sharp heel pain
insidious onset of heel pain, often when first getting out of bed
may prefer to walk on toes initially
worse at the end of the day after prolonged standing
relieved by ambulation
common to have symptoms bilaterally
> Physical exam
tender to palpation at medial tuberosity of calcaneus
dorsiflexion of the toes and foot increases tenderness with palpation
limited ankle dorsiflexion due to a tight Achilles tendon
tenderness at the origin of abductor hallucis
a small subset of patients
indicative of entrapment or irritation of the first branch of the lateral plantar nerve (Baxter’s nerve)
Differential Diagnosis:
> achilles tendonitis, Morton neuroma, calcaneal stress fracture, or inflammatory arthropathy.
Diagnosis:
>Radiographs

Plain film x-rays of the foot are of little benefit in typical cases of plantar fasciitis, although they may be helpful in ruling out other pathology.
X-rays are ordered initially if there is suspicion of a stress fracture or alternative cause of heel pain. Otherwise, x-rays are ordered subsequently if the patient does not improve with standard therapy. Radiographs may show infracalcaneal spurring but this is not needed for diagnosis and is more likely an incidental finding.
>investigations
Laboratory testing for rheumatoid factor is recommended when there are clinical or radiographic signs suggesting rheumatoid arthritis.
Rheumatoid factor is positive in 70% of patients with rheumatoid arthritis. Laboratory testing for HLA-B27 is recommended if there is any suspicion of a spondyloarthropathy (e.g., ankylosing spondylitis, Reiter disease).
Technetium bone scanning may be ordered if radiographs are inconclusive for stress fractures or if the patient does not respond to conservative treatment.
MRI is recommended in cases of recalcitrant heel pain (pain for more than 12 months) or if there are any soft tissue or osseous masses palpated or visualized in other imaging studies.
Ultrasound is an emerging investigation that may be used in place of MRI for the same indications. Ultrasound scanning demonstrates thickening of the plantar fascia by 4 mm or more in people with plantar fasciitis. Ultrasound investigation has also been able to reveal enthesopathy and hypoechogenicity.
Treatment of Plantar Fascitis
1.Pain Relievers Medicines mainly NSAIDs : Advil or Motrin (ibuprofen) and Aleve (naproxen), can help reduce plantar fasciitis pain and swelling.
Side effect: particularly when they are taken over a long period of time. Digestive system complaints, such as heartburn and nausea, are most common. Less common but serious side effects include allergic reactions, hypertension, and liver or kidney damage.
2. Cortisone Injections for Plantar Fasciitis: For severe pain and inflammation that do not respond to nonsteroidal medication.
side effect: Multiple injections can lead to a rupture of the plantar fascia or shrink the fat pad covering the heel bone.
Surgery for Plantar fasciitis
Plantar fasciotomy is often considered after conservative treatment has failed to resolve the issue after six months and is viewed as a last resort. Minimally invasive and endoscopic approaches to plantar fasciotomy exist but require a specialist who is familiar with certain equipment.
The availability of these surgical techniques is currently limited. A 2012 study found that 76% of patients who underwent endoscopic plantar
fasciotomy had complete relief of their symptoms and had few complications. Heel spur removal during plantar fasciotomy has not been found to improve the surgical outcome.
Plantar heel pain may occur for multiple reasons and release of the lateral plantar nerve branch may be performed alongside the plantar fasciotomy in select cases. Possible complications of plantar fasciotomy include nerve injury, instability of the medial longitudinal arch of the foot, fracture of the calcaneus, prolonged recovery time, infection, rupture of the plantar fascia, and failure to improve the pain. Coblation surgery has recently been proposed as an alternative surgical approach for the treatment of recalcitrant plantar fasciitis.
Physiotherapy Treatment of Plantar fasciitis
> Ice: simple and effective modality to reduce your pain and swelling. Please apply for 20-30 minutes each 2 to 4 hours during the initial phase or when you notice that your injury is warm or hot. A frozen water bottle can provide you with an ice foot roller that can simultaneously provide you with some gentle plantar fascia massage.
> Modalities Used in Treatment For Plantar Fasciitis :
-Iontophoresis
-Ultrasound therapy
–Deep friction massage
-Contrast bath
-TENS
> Shoe wear Modification (Running shoes) :
Flared, stable heel to help control heel stability. Firm heel counters to control the hindfoot. Soft cushioning of the heel, raising the heel 12-15 mm higher than the sole. Well molded Achilles pad. Avoid rigid leather dress shoes that increase torque on the Achilles tendon.
> Cushioned Heel Inserts in Treatment For Plantar Fasciitis :
Viscoheels. Soft cushions are placed in and out of whatever shoe the patient is wearing. Patients with abnormal biomechanics of the lower extremity, such as pes cavus or pes planus, may benefit from the eventual use of custom cushioned orthotics.
> Plantar fasciitis taping :
plantar fasciitis taping another useful technique for pain relief is taping. This technique reduces the pressure on your plantar fascia, which reduces your pain. When this taping technique is applied, you will feel an imminent relief of pain.
Exercise therapy
1. Standing calf stretch:

Stand facing a wall with your hands on the wall at about eye level. Keep your injured leg back with your heel on the floor. Keep the other leg forward with the knee bent. Turn your back foot slightly inward (as if you were pigeon-toed). Slowly lean into the wall until you feel a stretch in the back of your calf. Hold the stretch for 15 to 30 seconds. Return to the starting position. Repeat 3 times. Do this exercise several times each day.
2. Seated plantar fascia stretch:

Sit in a chair and cross the injured foot over the knee of your other leg. Place your fingers over the base of your toes and pull them back toward your shin until you feel a comfortable stretch in the arch of your foot. Hold 15 seconds and repeat 3 times.
3.Plantar fascia massage:

Sit in a chair and cross the injured foot over the knee of your other leg. Place your fingers over the base of the toes of your injured foot and pull your toes toward your shin until you feel a stretch in the arch of your foot. With your other hand, massage the bottom of your foot, moving from the heel toward your toes. Do this for 3 to 5 minutes. Start gently. Press harder on the bottom of your foot as you become able to tolerate more pressure.
4. Achilles stretch:

Stand with the ball of one foot on a stair. Reach for the step below with your heel until you feel a stretch in the arch of your foot. Hold this position for 15 to 30 seconds and then relax. Repeat 3 times.
5. Towel pickup:

With your heel on the ground, pick up a towel with your toes. Release. Repeat 10 to 20 times. When this gets easy, add more resistance by placing a book or small weight on the towel.
6. Heel raise:

Stand behind a chair or counter with both feet flat on the floor. Using the chair or counter as a support, rise up onto your toes and hold for 5 seconds. Then slowly lower yourself down without holding onto the support. (It’s OK to keep holding onto the support if you need to.) When this exercise becomes less painful, try doing this exercise while you are standing on the injured leg only. Repeat 15 times. Do 2 sets of 15. Rest 30 seconds between sets.
How to prevent Plantar Fascitis?
- Rest- Your body must rest to heal. If you start feeling pain in your feet, take some time off of your routine.
2. Ice and elevation – If you continue the movement that places pressure on your foot, even walking, it’s important to ice frequently and elevate to reduce swelling.
- Don’t push through the pain.
2. Don’t go barefoot



9 Comments