Wrist mobilization exercise
Table of Contents
What is Mobilization for the Wrist joint?
- Wrist Mobilization is a passive, skilled, manual therapy technique applied to wrist joints and related to the soft tissue at various speeds and amplitudes using physiological or accessory movement for therapeutic purposes.
- small amplitude force applies at a fast velocity, and a large amplitude force applies to slow velocity
- it is a manual technique that includes appealing to the target forces on a painful, stiff, or otherwise negotiated jointly with regard to improving its overall function. Which is not convenient in all situations, joint mobilizations help improve the range of motion, reduce pain, and minimize stiffness.
- Wrist Joint mobilization is a hands-on treatment that is usually executed by physiotherapists or healthcare professionals who specialize in rehabilitation for movement disorders and chiropractors, health professionals treating disorders of the musculoskeletal system that include bones, muscles, and soft tissue, ligaments
Introduction of the wrist joint
- There are three joints in the wrist complex
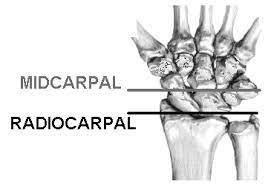
- Radiocarpal joint
- mid carpal joint
- ulnocarpal joint
- The wrist joint also specifies to as the radiocarpal joint is a condyloid variety of synovial joints of the distal upper limb that attaches and serves as a transition point between the forearm and hand. A condyloid joint is a modified ball and socket variety joint that permits flexion, extension, abduction, and adduction movements.
- The joint itself is rolled through the articulations between the distal radius and the scaphoid, lunate, and triquetrum bones. The proximal articulation forms a concave shape composed of a combination of the distal end of the radius and the articular disk. The distal articulation is convex and possessed of the scaphoid, lunate, and triquetrum bones of the proximal hand.
- The four ligaments responsible for maintaining the joint’s stability are the palmar and dorsal radiocarpal ligaments and the ulnar and radial collateral ligaments. The palmar radiocarpal ligaments are the most muscular ligaments helping structures, and these ligaments attach the radius to both the proximal and distal rows of carpal bones. Besides stability, the ligaments also assure that the hand and forearm move together during supination.
- The dorsal radiocarpal ligament is related to the palmar ligament excluding that it is located on the dorsal side of the wrist joint and its alternative function is to assure that the hand locomotes with the forearm during pronation. The ulnar collateral ligament is a distinction from the ulnar styloid process to the triquetrum and pisiform bones. The radial collateral ligament runs in distinction to the radial styloid process to the scaphoid and trapezium bones. Both collateral ligaments give stability by decelerating lateral motion.
- Surrounding the wrist joint is a double-layered joint capsule, which is common amongst all synovial joints. The outer layer is fibrous and connects to the radius, ulna, and carpal bones. The inner layer forms a synovial membrane which covered synovial fluid and lubricates the joint
Blood Supply of the radiocarpal joint
- Blood supply to the forearm and hand awakes from the ulnar and radial artery .ulnar and radial arteries give vasculature to the wrist joint through penetrating branches from the dorsal and palmar carpal arches.
Nerves supply the radiocarpal joint
- The wrist joint gain innervation from the three major nerves of the forearm.
- Median nerve: by the anterior interosseous branch
- Radial nerve: via the posterior interosseous branch
- Ulnar nerve: Directly terminated its deep motor branches
Muscles are for needed the movement of the radiocarpal joint
- Muscles in the forearm control wrist movement. The body of each muscle is addressed proximally in the forearm, and their tendons extend distally beyond the wrist joint. Their movements can group muscles corresponding with the wrist joint.
- Flexors: Flexor carpi radialis, flexor carpi ulnaris, flexor digitorum superficialis, flexor digitorum profundus, and to a lesser extent flexor pollicis longus and palmaris longus
- Extensors: Extensor carpi radialis longus, extensor carpi radialis brevis, extensor carpi ulnaris, extensor digitorum and to a lesser extent extensor indicis
- Abductors: Abductor pollicis longus, flexor carpi radialis, extensor carpi radialis longus, and extensor carpi radialis brevis
- Adductors: Flexor carpi ulnaris, extensor carpi ulnaris
Ulnocapal joint
- In The ulnocarpal joint the ulna, one of the forearm bones, joins with the lunate and triquetrum wrist bones.
Midcarpal joint
- The midcarpal joint is articulated by the eight carpal bones that make up the carpus. From lateral to medial, the proximal row of carpal bones is made up of the following bones:
- scaphoid
- lunate
- triquetrum
- pisiform
- From lateral to medial, the distal row is fabricated of the following bones:
- trapezium
- trapezoid
- capitate
- hamate
- The midcarpal joint is the articulation between the proximal row of carpal bones and the distal row of carpal bones mentioned above. At the lateral portion of the joint, the scaphoid connects with the trapezium and trapezoid bone. Centrally, the scaphoid and lunate connect with the capitate bone. The lunate also connects with the hamate bone, while the latter of bones also connects with the triquetrum of the proximal row.
Ligaments of the midcarpal joint
- As the carpal bones of the midcarpal joint are not grasped together by their shapes such as the ball and socket variety joint of the wrist, the joint capsule of the midcarpal joint is assisted by several ligaments along with the extensor and flexor retinaculum and various tendons of muscles to stabilize the joint along with the intercarpal (interosseous) ligaments involve the palmar intercarpal and dorsal intercarpal ligaments and radial and ulnar collateral ligaments.
- Intercarpal ligaments: They link some contiguous carpals.
- Palmar intercarpal ligament: Anteriorly, it extends from the proximal row of the carpal bones to mostly the head of the capitate sometimes known as the radiate capitate ligament or palmar ligament.
- Dorsal intercarpal ligament: Posteriorly, it projects from the proximal to the distal row of carpal bones.
- Radial collateral ligament: A strong ligament that is a sustaining of the radial collateral carpal ligament from the wrist joint that extends from the scaphoid bone to the trapezium bone.
- Ulnar collateral ligament: same as the radial collateral ligament, the ulnar collateral ligament is an extension. It is a continuation of the ulnar collateral carpal ligament and it connects the hamate bone to the triquetrum.
- movement of midcapal joint : flexion,extension,adduction,abduction
Diseases required mobilization of the wrist joint
- Scaphoid lunate advanced collapse (SLAC)
- Scaphoid nonunion advanced collapse (SNAC)
- Other degenerative wrist conditions
- Rheumatoid arthritis
- Pisotriquetral arthritis
- DRUJ abutment/arthrosis
Procedures need mobilization after surgery of the wrist joint
- Proximal row carpectomy (PRC)
- Scaphoid excision and 4-corner fusion
- Total wrist fusion
- Total wrist replacement
Goals for wrist joint mobilization
pain, muscle guarding, and spasm
- painful joint, reflex, muscle guarding, and muscle spasm can be mediated with gentle joint play techniques to stimulate neurophysiological and mechanical effect
Neurophysiological effect
- small amplitude oscillatory and distraction movement are acclimated to stimulate mechano receptors that may inhibit the transmission of nociceptive stimuli at the spinal cord or brain stem level
Mechanical effect
- small amplitude distraction or gliding movement of the joint is acclimated cause synovial fluid motion, which is a vehicle for carrying nutrients to avascular portions of the articular cartilage
- gentle joint play procedures help to maintain nutrient exchange and prevent the painful and degenerating effects of statis when the joint is swollen or painful, and can not go through a range of motion
- when adapted to treat pain, muscle spasms, and muscle guarding these techniques should not place stretch on the reactive tissue
Reversible joint hypomobility
- reversible joint hypomobility can be mediated with progressively vigorous joint play stretching procedure to elongate hypermobile capsular and ligamentous connective tissue
- sustained or distraction stretch forces are acclimated to distend the shortened tissue mechanically
Positional faults/subluxations
- A faulty position of one bony partner with regard to its opposing surface may outcome in limited motion or pain
- positional faults can occur with traumatic injury, after periods of immobility, muscle imbalance
- the faulty position may be preserved by maladapted neuromuscular control across the joint
- during attempting an active range of motion, faulty tracking of the joint surface results in pain or limited motions
Progressive limitations
- diseases that progressively restrict movement can be treated with joint play techniques to maintain available motion or lessen progressive mechanical restrictions
- the patient’s response manner the dosage of distraction or glide to treatment and the state of the disease
Functional immobility
- when the patient can’t functionally move a joint for a longer period of time
- the joint can be mediated with nonstretch gliding or distraction procedure to maintain available joint play and prevent the degenerating and restricting effect of immobility
Grades of mobilization of the wrist joint
Non-thrust oscillation techniques
- the oscillation may be performed using physiological movement
- grade 1:small amplitude rhythmic oscillation is applied at the beginning of the range, rapid oscillation like manual vibration
- grade 2:large amplitude rhythmic oscillation is done within range, not reach the limit, perform 2 or 3 seconds for 1 to 2 minutes
- grade3:large amplitude rhythmic oscillation is applied up to an available range of motion, stress into tissue resistance, perform 2 or 3 seconds for 1 to 2 minutes
- grade4:small amplitude rhythmic oscillation is executed at the available range of motion, the stress in tissue resistance, rapid oscillation like manual vibration
- grade 1 and 2 are used to treat joint limitation of movement by pain or muscle guarding
- grade 3 and 4 are helpful for stretch maneuver
Nonthrust sustained joint play techniques
- This system interprets only joint play techniques that separate (distract) or glide the joint surface
- grade 1(loosen): small amplitude distraction is applied when no stress is placed on the capsule, it equalizes cohesive force, muscle tension, and atmospheric pressure acting on joint
- grade2(tighten): enough distraction or glide is applied to tighten the tissue surrounding the elbow joint
- grade3(stretch): a distraction or glide is applied with an amplitude large enough to put a stretch on the joint capsule surrounding the periarticular structure
- grade 1 distraction is applied with all glide motion
- apply periodic distraction for 7 to 10 seconds with a few seconds of rest in between several cycles
- grade 2 distraction is helpful to determine the sensitivity of the joint, once the joint reaction is known treatment dosage increases and decreases
- gentle grade 2 distraction apply periodically used to prevent pain and maintain joint play when ROM is not allowed
- grade 3 distractions or glides are helpful to stretch joint structure, increase joint play motion
- for restricted joints apply a minimum of 6 seconds of stretch force chased by partial release (grade 1 or 2)
- reps:3 to 4-second intervals
Radiocarpal joint mobilization
- the concave distal radius articulates with the convex proximal row of carpal bones, which is composed of scaphoid, lunate, triquetrum
- resting position: a straight line position till the radius and third metacarpal with slight ulnar deviation
- treatment plane: the articulating surface of the radius is perpendicular to the long axis of the radius
- stabilization: distal radius and ulna
Radiocarpal distraction

- patient position: sitting with the forearm supported on the treatment table and the wrist over the edge of the table
therapist position and hand placement
- the hand which is closest to the patient, grasp the hand around the styloid process
- fixate the radius and ulna against the treatment table
- grasp around the distal row of carpal bones with your other hand
mobilizing force
- pull in the distal direction with respect to the arm
- radiocarpal distraction is used to control the pain and improve the general mobility of the wrist
Radiocarpal joint dorsal glide

- patient position: sitting with forearm supported on the treatment table in pronation position
therapist position and hand placement
- the hand which is closest to the patient, grasp the hand around the styloid process
- fixate the radius and ulna against the treatment table
- grasp around the distal row of carpal bones with your other hand
- progress by moving the wrist to the end of the available range of motion
- gliding in a dorsal direction
mobilizing force
- the force comes around the distal row of carpal bones
- this glide is used to increase flexion
Radiocarpal joint volar glide

- patient position: sitting with forearm supported on the treatment table in pronation position
therapist position and hand placement
- the hand which is closest to the patient, grasp the hand around the styloid process
- fixate the radius and ulna against the treatment table
- grasp around the distal row of carpal bones with your other hand
- progress by moving the wrist to the end of the available range of motion
- gliding in a volar direction
mobilizing force
- the force comes around the distal row of carpal bones
- this glide is used to increase extension
Radiocarpal radial glide

- patient position: sitting with forearm supported on the treatment table in the mid-prone position
therapist position and hand placement
- the hand which is closest to the patient, grasp the hand around the styloid process
- fixate the radius and ulna against the treatment table
- grasp around the distal row of carpal bones with your other hand
- progress by moving the wrist to the end of the available range of motion
- gliding in the ulnar direction
mobilizing force
- the force comes around the distal row of carpal bones
- this glide is used to improve ulnar deviation
Radiocarpal ulnar glide

- patient position: sitting with forearm supported on the treatment table in the mid-prone position
therapist position and hand placement
- the hand which is closest to the patient, grasp the hand around the styloid process
- fixate the radius and ulna against the treatment table
- grasp around the distal row of carpal bones with your other hand
- progress by moving the wrist to the end of the available range of motion
- gliding in the radial direction
mobilizing force
- the force comes around the distal row of carpal bones
- this glide is used to improve radial deviation
carpal bones mobilization

- patient position: sitting with forearm supported on the treatment table
therapist position
- stand and grasp the patient’s hand so the elbow hangs and is unsupported
- the weight of the arm provides a slight distraction to the joints, so you need to apply only glides
hand placement
- identify the specific articulations to be mobilized
- place your index finger on the volar surface of the bone to be stabilized
- place the protruding thumbs on the dorsal surface of the bone to be mobilized
- the rest of the fingers hold the patient’s hand so it is relax
mobilizing force
- force comes from the overlapping thumb on the dorsal surface
- pressure against the nerve, blood vessels, the tendon in the carpal tunnel, and Guyon’s canal is minimized
- stronger mobilization force can be utilized without pain
- high-velocity thrust technique can be used by providing quick downward and upward flick of your wrist and hands while pressing against the respective carpals

- To increase flexion: place the stabilizing index finger under the bone that is concave
- mobilizing thumb overlapped on the dorsal surface of the bone that is concave
- the thumbs on the dorsum of the concave radius, index finger stabilized scaphoid
- the thumbs on the dorsum of the concave radius, index finger stabilized lunate
- the thumbs on the dorsum of the trapezium-trapezoid unit, index finger stabilize scaphoid
- the thumbs on the dorsum of concave lunate, index finger stabilize capitate
- the thumbs on the dorsum of the concave triquetrum, and index finger stabilize hamate
- To increase extension: place the stabilizing index fingers under the bone that is concave (volar surface)
- protruding thumb place the dorsal surface of the bone that is convex
- thumbs provide the manipulating force
- the thumbs on the dorsum of the convex scaphoid, index finger stabilized radius
- the thumbs on the dorsum of the convex lunate, index finger stabilized radius
- the thumbs on the dorsum of the convex scaphoid, and index finger stabilize the trapezium-trapezoid unit
- the thumbs on the dorsum of convex capitate, index finger stabilize lunate
- the thumbs on the dorsum of convex hamate, index finger stabilize triquetrum
carpometacarpal and intermetacapal joint digits 2 to 5 mobilization
- The bases of the second, third, fourth, and fifth metacarpal bones articulate with one another by small surfaces covered with cartilage and are attached together by dorsal, palmar, and interosseous ligaments.
- The dorsal and palmar ligaments pass transversely from one bone to another bone on the dorsal and palmar surfaces. The interosseous ligaments connect the contiguous surfaces of the bones, just distal to their collateral articular facets.
- The synovial membrane of these joints is continuous with the carpometacarpal articulations.
- opening and closing the hand and maintenance of the arches in the hand requires general mobility between carpals and metacarpals
Carpometacarpal distraction

stabilization and hand placement
- stabilize the respective carpal with the thumb and index finger of the one hand
- another hand grasp around the proximal portion of a metacarpal
mobilizing force
- apply long axial traction to the metacarpal
Carpometacarpal and intermetacarpal volar glide

- patient position: sitting with forearm supported on the treatment table
- place the rolled towel under the wrist joint
stabilization and hand placement
- stabilize the carpals with the thumb and index finger of the one hand
- place the thenar eminence of your other hand along the dorsal aspect of the metacarpal to provide mobilizing force
mobilizing force
- glide the proximal portion of the metacarpal volar ward
- this glide is used to increase the mobility of the arch of the hand
Precaution for mobilization of the wrist joint
Hypermobility
- the joint of a patient with potential necrosis of the ligaments should not be manipulated with stretching techniques
Joint effusion
- the joint effusion as a result of trauma or disease
- rapid swelling of the joint generally indicates bleeding in the joint and may occur with diseases
- medical intervention is necessary for aspiration of the blood to decrease the necrotizing effect on the articular cartilage
- slow swelling for more than 4 hours generally specifies serious joint effusion or edema on the joint due to mild trauma irritation or disease
- do not stretch swollen joints with mobilization because the capsule is already stretched by being expanded to contain the extra fluid
- the limitation of movement is from extra fluid and muscle response to pain, not from shortened fibers
- a slight oscillating movement that does not stress or stretch the capsule may need to block the transmission of a pain stimulus so it is not anticipated and may use to regain fluid flow during maintaining available joint play
- if the patient’s response to slight techniques is accelerated pain or joint irritability
- the techniques were applied too forcefully or should not do with the current state of pathology
Inflammation
- whenever inflammation is present, stretching cause increase pain and muscle guarding and result in greater tissue damage
- gentle distraction motions may temporarily prevent the pain response
- neglect excessive wrist flexion or extension during activities of daily living. neglect speedy changes in workload and/or activity. Remember that the body will modify to a given workload if it is given adequate time to modify. When evaluating a new activity, restrict the amount of new activity for a given session. Try to vary activities as much as possible to change the type of stress. understand that the body can be made deconditioned during an extended leave of absence such as a long vacation, sick leave, or maternity leave. Upon return, accelerate activity gradually.
- neglect excessive wrist flexion or extension during activity and neglect wrist flexion at night.
- neglect large forces on the wrist especially when the wrist is extended. Whenever possible, try to keep the wrists straight during the activity. Use two hands to grasp relatively heavy objects such as full binders. The use of two hands helps distribute the load and results in increased control of wrist position.
FAQS
- can we do mobilization with rheumatoid arthritis of the wrist joint ??
manual mobilization of the hands of patients with RA was shown to be achievable, safe, and effective to integrate into specialized healthcare clinics.
- how much time is taken for mobilization after total wrist replacement?
After 1 or 2 months of POP, mobilization is applied because the synovial formation of bone takes time to connect the bone
- How does joint mobilization reduce pain?
grade 2:large amplitude measured oscillation is done within the range of motion, not arrive the limit, performing 2 or 3 seconds for 1 to 2 minutes
that transfer center way into the joint range of motion, obtaining any part of the range and yet not reaching the end range. This technique can be utilized to treat joint stiffness by accelerating the range of motion and joint pain - can mobilization of the wrist be good before surgery ??
Early mobilization decelerates the risk of postoperative complications, accelerates the rehabilitation of functional capacity, positively impacts several patient-reported outcomes, and decreases hospital length of stay, thereby fewer care costs.
- How long do you do joint mobilization for the wrist?
Typical treatment of the wrist joint may involve a series of three to six mobilizations persisting up to 30 seconds, with one to three oscillations or glide per second