Plantar Fascia Tear
Table of Contents
Introduction:
A painful tear in the plantar fascia is known as a plantar fascial rupture. The plantar fascia is a band of connective tissue that runs over the sole of the foot. Plantar fasciitis may increase the probability of a rupture. A plantar fascial rupture can sometimes confuse with plantar fasciitis or even a calcaneal fracture.
A plantar fascia tear refers to the partial or complete rupture of the plantar fascia, which is a thick band of connective tissue located on the sole of the foot. This tear can occur due to various factors, including overuse, sudden trauma, or pre-existing conditions like plantar fasciitis.
When the plantar fascia tears, it can lead to sharp and often intense heel pain, particularly during activities that place stress on the foot, such as walking, running, or standing. The pain is typically felt at the bottom of the heel and can extend along the arch of the foot. Other symptoms might include swelling, tenderness, stiffness, and discomfort when flexing or pointing the toes.
Plantar fascia tears can range from mild to severe, depending on the extent of the tear and the underlying factors involved. Diagnosis usually involves a physical examination, medical history review, and sometimes imaging tests like ultrasound or MRI to confirm the extent of the tear and rule out other possible conditions.
What is a Plantar Fascia Tear?
Plantar fascia tears are uncommon, however, they can occur in conjunction with plantar fasciitis. Plantar fascia rips typically develop as a result of a stressful experience, such as walking on something or being subjected to a quick force that strains the plantar fascia.
People with plantar fascia tears, also known as plantar fasciitis, generally experience a painful heel and pain when they first get out of bed, which subsides significantly with initial walking but returns with continuous walking.
In the context of the plantar fascia, a tear refers to a disruption or rupture of the tissue fibers due to injury or strain. Tears can vary in severity from small microtears to larger ruptures.
Tears in the plantar fascia can occur due to sudden trauma, chronic stress, or as a result of untreated plantar fasciitis. Small tears might cause mild discomfort, while larger tears can lead to significant pain, swelling, and limited mobility. Severe tears might even cause a complete rupture of the plantar fascia.
Anatomy of Plantar Fascia:
The plantar fascia, also known as the plantar aponeurosis, is a strong connective tissue aponeurosis that supports the arch of the foot on the bottom (plantar side). Recent research suggests that the plantar fascia is an aponeurosis rather than a genuine fascia. It reaches the heads of the metatarsal bones (the bones between each toe and the bones of the mid-foot) from the calcaneus tuberosity (heel bone).
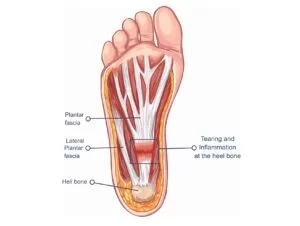
Origin and Attachment: The plantar fascia originates from the medial tubercle of the calcaneus (heel bone), which is a bony prominence on the inner side of the heel. From this point, the plantar fascia extends forward towards the toes.
The plantar fascia is the thick central tissue that surrounds the plantar muscles. It runs from the medial process of the tuber calcanei to the proximal phalanges of the toes. It offers some connection to the toe flexor muscles.
The plantar fascia becomes continuous distally, with fibrous sheats encircling the flexor tendons as they progress to the toes. The plantar aponeurosis creates the superficial transverse metatarsal ligament at the anterior extremity of the sole, inferior to the metatarsal heads.
Structure:
The plantar fascia is mostly composed of longitudinally oriented collagen fibers.
Three Bands: The plantar fascia can be divided into three distinct bands or portions:
- Medial Band: This is the largest and most prominent band of the plantar fascia. It extends from the medial tubercle of the calcaneus towards the base of the big toe (first metatarsophalangeal joint).
- Central Band: This portion lies adjacent to the medial band and extends toward the bases of the second and third toes.
- Lateral Band: The lateral band extends from the calcaneus to the base of the fifth toe (fifth metatarsophalangeal joint).
Function: The plantar fascia serves multiple functions that are crucial for the biomechanics of the foot and lower limb:
- Arch Support: It helps to maintain the shape of the foot’s arches, providing stability and distributing weight evenly across the foot.
- Shock Absorption: The plantar fascia acts as a shock absorber, dissipating the impact forces generated during activities like walking, running, and jumping.
- Energy Storage and Release: During activities like walking and running, the plantar fascia stores elastic energy as it stretches and then releases that energy as the foot pushes off the ground, aiding in propulsion.
Fibrous Structure: The plantar fascia is primarily composed of dense, fibrous connective tissue. It consists of collagen fibers that provide tensile strength and stability to the structure.
Muscular Attachments: The plantar fascia is connected to several muscles in the foot, including the intrinsic muscles of the foot that control its movements. These muscles play a role in stabilizing the foot during various activities.
Blood Supply: The blood supply to the plantar fascia is limited, particularly in comparison to muscles. This can impact its healing capacity when injured.
Arch Support: One of the primary functions of the plantar fascia is to support the arches of the foot. The plantar fascia helps maintain the integrity of these arches, providing stability and shock absorption during activities like walking, running, and standing.
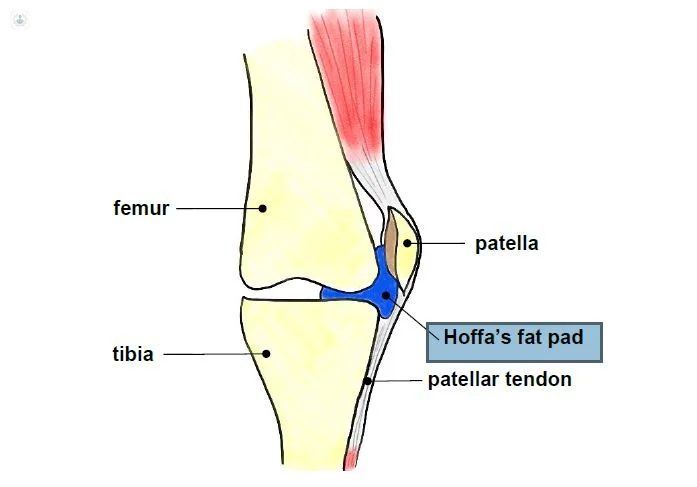
Fat Pad: Beneath the plantar fascia, there’s a layer of adipose (fat) tissue known as the plantar fat pad. This pad provides additional cushioning and shock absorption, enhancing the foot’s ability to absorb forces during weight-bearing activities.
Nerve Supply: The plantar fascia is innervated by sensory nerves. Injuries or irritation of these nerves can contribute to pain in conditions like plantar fasciitis.
Symptoms of Plantar Fascia Tear
1. Sharp Heel Pain: The hallmark symptom is a sharp, stabbing pain in the bottom of the heel. This pain is typically worse in the morning when you take your first steps out of bed or after periods of rest. It may also intensify after prolonged periods of standing or activity.
2. Localized Tenderness: The area where the plantar fascia attaches to the heel bone (calcaneus) becomes tender to touch. Pressing on this area can elicit pain.
3. Swelling: The affected area might become swollen due to inflammation and irritation of the torn tissue. Swelling can contribute to discomfort and may be more noticeable after prolonged activity.

4. Stiffness: You might experience stiffness in the bottom of your foot, especially in the morning or after periods of inactivity. This can improve with movement but may return after rest.
5. Pain Along the Arch: The pain can also extend along the arch of the foot, as the plantar fascia runs from the heel to the base of the toes. This pain might be more pronounced during walking or other weight-bearing activities.
6. Pain Progression: If left untreated, the pain can worsen over time and become more constant. It may start affecting your daily activities and quality of life.
7. Reduced Range of Motion: Some individuals with a plantar fascia tear might experience limitations in their ability to flex and point their toes, which can affect their gait and movement.
Causes of Plantar Fascia Tear
1. Overuse: Repetitive strain and overuse of the plantar fascia, often from activities that involve excessive running, jumping, or standing, can lead to small tears in the tissue over time.
2. Sudden Impact or Trauma: A sudden impact to the heel, such as from a fall or landing incorrectly, can cause the plantar fascia to tear.
3. Age: As we age, the plantar fascia can become less flexible and more prone to injury, including tearing.
4. Improper Footwear: Wearing shoes that do not provide enough arch support or cushioning, or that do not fit properly, can put additional strain on the plantar fascia and increase the likelihood of tears.
5. Tight Calf Muscles: Tight calf muscles can place additional strain on the plantar fascia, making it more susceptible to tears.
6. Obesity: Excess body weight can increase the load placed on the plantar fascia, leading to increased stress and potential tearing.
7. Structural Factors: Abnormal foot arches (high arches or flat feet) can lead to improper distribution of forces on the plantar fascia, increasing the risk of tears.
8. Inadequate Warm-up: Engaging in physical activities without proper warm-up exercises can increase the risk of injury, including plantar fascia tears.
9. Pre-existing Conditions: Certain conditions like plantar fasciitis (inflammation of the plantar fascia) can weaken the tissue and make it more susceptible to tears.
10. Biomechanical Issues: Abnormalities in foot mechanics, such as overpronation (excessive inward rolling of the foot) or supination, can contribute to increased stress on the plantar fascia.
Risk factors:
Several risk factors can increase the likelihood of developing a plantar fascia tear. These include:
1. Age: The risk of a plantar fascia tear increases with age, as the tissue becomes less flexible and more prone to injury.
2. Physical Activity: Engaging in high-impact activities like running, jumping, or dancing can place repeated stress on the plantar fascia, raising the risk of tearing.
3. Improper Footwear: Wearing shoes that lack proper arch support or cushioning, especially during activities that involve prolonged standing or walking, can contribute to the risk of injury.
4. Obesity: Excess body weight places added strain on the plantar fascia, increasing the chances of injury and tears.
5. Foot Structure: Having flat feet, high arches, or other structural abnormalities can alter how weight is distributed across the foot, making the plantar fascia more vulnerable to tearing.
6. Tight Muscles: Tight calf muscles or Achilles’ tendons can increase tension on the plantar fascia, increasing the risk of tearing.
7. Sudden Increase in Activity: Rapidly increasing physical activity intensity, duration, or frequency without proper conditioning can strain the plantar fascia and lead to tears.
8. Poor Foot Mechanics: Abnormal foot mechanics, such as overpronation or supination, can lead to uneven stress on the plantar fascia and heighten the risk of injury.
9. Occupational Factors: Jobs that involve prolonged standing or walking on hard surfaces can contribute to the development of plantar fascia tears.
10. Previous Foot Injuries: If you’ve had previous foot injuries or conditions like plantar fasciitis, your plantar fascia might already be weakened, making it more susceptible to tears.
11. Inadequate Warm-up or Stretching: Skipping warm-up exercises or neglecting to stretch the calf muscles and plantar fascia before physical activity can increase the risk of injury.
12. Genetics: Certain genetic factors might influence the structure and strength of your plantar fascia, affecting your risk of developing tears.
Classification:
Plantar fascia tears can be classified based on their severity and extent. There are generally three classifications:
- Grade I (Mild Tear): In this classification, the plantar fascia has minor microtears or stretching. It may be inflamed and cause mild pain, especially during activity. Swelling and tenderness might be present, but the overall structural integrity of the fascia is maintained.
- Grade II (Partial Tear): A Grade II tear involves a more significant tearing of the plantar fascia, where a portion of the tissue is torn but still partially connected. This can result in moderate to severe pain, especially during weight-bearing activities. Swelling, tenderness, and difficulty with movement might be more pronounced.
- Grade III (Complete Tear): A Grade III tear is a complete rupture of the plantar fascia, where the tissue is fully torn. This can cause severe pain and functional impairment. The ability to bear weight and move the foot might be greatly compromised. Swelling and bruising could also be more noticeable.
The classification helps guide treatment decisions and gives a sense of the severity of the tear. Mild tears might respond well to conservative measures like rest, icing, and physical therapy. Partial tears might require more structured interventions such as immobilization, orthotics, and possibly corticosteroid injections. Complete tears might need more intensive treatments, including immobilization, physical therapy, and in some cases, surgical repair.
Differential diagnosis:
When considering a possible plantar fascia tear, it’s important to rule out other conditions that can cause similar symptoms. Differential diagnosis involves identifying and distinguishing between various conditions that might present with heel pain and related symptoms.
- Plantar Fasciitis: This is inflammation of the plantar fascia, often caused by repetitive stress. It can cause intense heel pain, especially in the morning or after rest. While not a tear, it can mimic some of the symptoms.
- Heel Spurs: These are bony growths that can form on the heel bone due to prolonged plantar fasciitis. They may aggravate discomfort and heel pain.
- Achilles Tendonitis: Inflammation of the Achilles tendon can cause pain at the back of the heel. It can sometimes be mistaken for plantar fascia issues due to the proximity of the pain.
- Stress Fractures: Fractures in the heel bone (calcaneus) or other bones of the foot can cause similar pain and discomfort, especially during weight-bearing activities.
- Tarsal Tunnel Syndrome: This is a condition similar to carpal tunnel syndrome but in the foot. The bottom of the foot may experience discomfort, tingling, and numbness as a result.
- Nerve Entrapment: Conditions like Baxter’s neuritis involve the entrapment of nerves in the foot, leading to localized pain.
- Calcaneal Bursitis: Inflammation of the bursa, a fluid-filled sac near the heel, can lead to pain and swelling in the area.
- Fat Pad Atrophy: Thinning of the fat pad in the heel can cause pain due to reduced cushioning.
- Rheumatoid Arthritis or Gout: These systemic conditions can also affect the feet and cause pain in the heel region.
- Nerve Impingement: Conditions like sciatica can radiate pain into the foot and heel.
- Ankle Instability: Chronic ankle instability can lead to improper foot mechanics, contributing to heel pain.
Proper differential diagnosis involves a comprehensive medical history review, physical examination, and sometimes imaging tests such as X-rays, ultrasounds, or MRIs to accurately identify the underlying condition.
Mechanism of injury:
The mechanism of injury for a plantar fascia tear often involves sudden or repetitive stress that exceeds the tissue’s capacity to withstand tension. Several things can cause this tear, including:

- Overuse: Prolonged and repetitive activities like running, jumping, or standing on hard surfaces can gradually weaken the plantar fascia over time. The cumulative stress can lead to micro-tears that eventually result in a tear.
- Sudden Impact: A sudden and forceful impact to the heel, such as from a fall or landing incorrectly, can place excessive stress on the plantar fascia, causing it to tear.
- Excessive Force: Activities that involve sudden changes in direction, pivoting, or sudden acceleration can put significant force on the plantar fascia, potentially leading to a tear.
- Improper Footwear: Wearing shoes with inadequate arch support or cushioning can contribute to improper distribution of forces on the plantar fascia, making it more susceptible to tearing.
- Changes in Activity Level: Rapidly increasing physical activity intensity, duration, or frequency without proper conditioning can strain the plantar fascia and lead to tears.
- Structural Factors: Foot abnormalities like high arches or flat feet can alter the mechanics of the foot, placing uneven stress on the plantar fascia and increasing the risk of a tear.
- Tight Muscles: Tight calf muscles or Achilles’ tendons can increase tension on the plantar fascia, making it more vulnerable to tearing.
- Age: The aging process can result in decreased flexibility and strength of the plantar fascia, increasing the risk of injury.
- Pre-existing Conditions: Conditions like plantar fasciitis or other foot problems can weaken the plantar fascia and make it more prone to tearing.
- Obesity: Excess body weight places additional stress on the plantar fascia, increasing the likelihood of injury.
The mechanism of injury can vary depending on the individual’s activities, foot structure, and other contributing factors.
Diagnostic Procedures:
Diagnosing a plantar fascia tear typically involves a combination of clinical evaluation, medical history review, and sometimes imaging tests.
- Medical History Review: Your healthcare provider will ask you about your symptoms, including the nature and duration of your heel pain, any recent activities or injuries that might have triggered the pain, and your medical history.
- Physical Examination: A thorough physical examination will be conducted, focusing on your foot and lower leg. Your healthcare provider will look for signs of swelling, tenderness, bruising, and changes in foot mechanics.
- Palpation: Your healthcare provider may press on different areas of your foot to assess tenderness and pinpoint the source of pain. Palpation of the plantar fascia attachment points may be particularly informative.
- Range of Motion Assessment: You may be asked to move your foot and toes in different directions to assess your range of motion and any pain associated with movement.
- Clinical Tests: Various clinical tests can help confirm a plantar fascia tear. These might include the “Windlass Test,” where pressure is applied to the toes to stretch the fascia and reproduce pain.
- Functional Movement Assessment: The physiotherapist observes how you walk, stand, and perform specific movements to assess your gait and foot mechanics.
- Foot Posture Assessment: Observing your foot posture and alignment, along with assessing factors like arch height, can provide clues about the health of the plantar fascia.
- Calf Muscle Length Assessment: The physiotherapist checks the flexibility of the calf muscles. Tight calf muscles can affect foot mechanics and the plantar fascia.
Imaging Tests: In some cases, imaging tests may be recommended to confirm the diagnosis and assess the extent of the tear. Common imaging methods include:
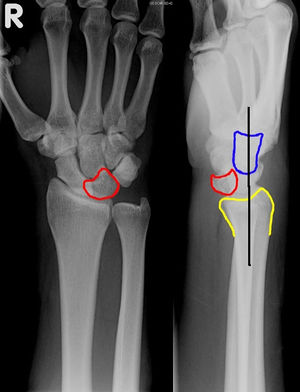
- X-rays: While X-rays don’t directly show soft tissues like the plantar fascia, they can help rule out other conditions such as bone fractures or heel spurs.
- Ultrasound: This imaging method can visualize soft tissues like the plantar fascia and identify tears, inflammation, and thickness changes. In general, thickening of the plantar fascia at its connection to the heel is seen in patients with long-standing plantar fasciitis. Furthermore, there are localized regions of fiber disruption, with separation and swelling between the fibers caused by hemorrhage. When we stretch the heel, we can show the separation of the plantar fascia fibers on ultrasound, which confirms a rupture.
- MRI (Magnetic Resonance Imaging): MRI provides detailed images of soft tissues, making it a valuable tool for confirming a plantar fascia tear, assessing its severity, and ruling out other conditions. MRI demonstrates plantar fascia thickening, comparable to plantar fasciitis. However, we find an extremely bright signal indicative of a tear rather than plantar fasciitis on some of the more advanced MRI sequences. This strong signal also travels to the heel and soft tissues, indicating hemorrhage and edema.
- Differential Diagnosis: Your healthcare provider will consider other potential causes of your symptoms and rule out conditions with similar presentations, such as plantar fasciitis, heel spurs, stress fractures, and nerve entrapment.
- Consultation with Specialists: In some cases, a referral to a podiatrist, orthopedic specialist, or sports medicine physician might be recommended for a more specialized assessment and treatment plan.
Special tests:
Physiotherapy professionals use a variety of special tests to assess the presence of plantar fascia tears or related conditions. These tests help in diagnosing the issue and developing an appropriate treatment plan.
- Plantar Fascia Palpation: Your healthcare provider will palpate (press and feel) along the plantar fascia, looking for areas of tenderness, swelling, and changes in texture that might indicate a tear.
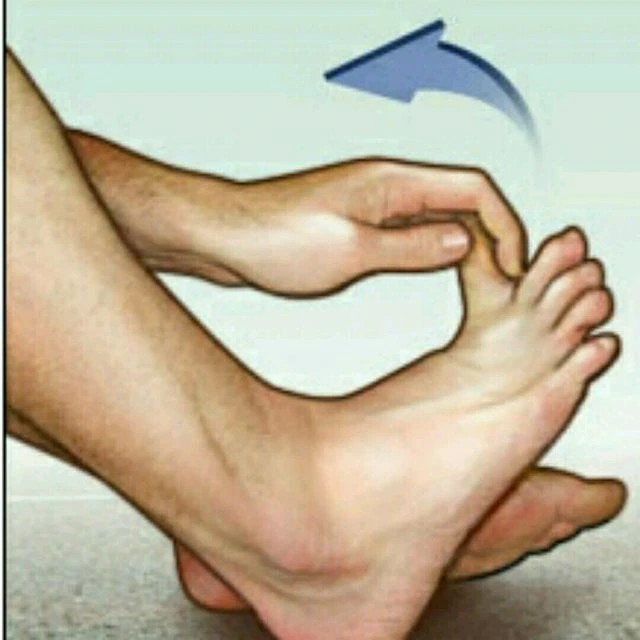
- Windlass Test: This test involves dorsiflexing the toes (pulling them towards the shin) while the foot is passively plantarflexed (pointed). If pain is reproduced in the area of the plantar fascia, it can suggest a tear or inflammation.
- Silfverskiöld Test: This test checks for Achilles tendon tightness. When you perform a calf stretch with your knee straight, and then with your knee bent, it can help identify tightness that might impact the plantar fascia.
- Thompson Test: While not directly related to the plantar fascia, this test assesses the integrity of the Achilles tendon. It involves squeezing the calf while observing the foot for movement. If the foot doesn’t move (no plantarflexion) during calf squeeze, it could indicate an Achilles tendon rupture.
- Plantar Fascia Tension Test: This test involves passive dorsiflexion of the toes to stretch the plantar fascia. If pain is elicited in the area of the fascia, it could indicate a tear or inflammation.
- Heel Drop Test: The patient stands on a step or elevated surface and drops their heels down, allowing the calf muscles to stretch. If this causes pain in the heel or along the plantar fascia, it might be a sign of an issue.
- Navicular Drop Test: This test assesses pronation and the arch of the foot. If there’s excessive navicular drop (lowering of the arch) when going from a seated to a standing position, it could indicate biomechanical issues affecting the plantar fascia.
- Toe Flexor Endurance Test: The patient performs toe flexion exercises (like picking up marbles with the toes) until fatigued. This test can provide insights into the strength and endurance of the intrinsic foot muscles that affect the plantar fascia.
- Arch Compression Test: Pressure is applied to the medial arch of the foot. Pain during this compression might be indicative of plantar fascia involvement.
Medical Treatment of Plantar Fascia Tear
Rest and Activity Modification: Avoid activities that aggravate foot discomfort and stress. It is critical to let the injured plantar fascia heal.
Ice: Ice applied to the afflicted region might help decrease inflammation and relieve discomfort. Ice should be administered for 15-20 minutes at a time, multiple times each day.
Pain Management: Nonsteroidal anti-inflammatory medicines (NSAIDs), such as ibuprofen, can help control pain and decrease inflammation. These, however, should only be used under physician supervision.
Orthotics and Supportive Footwear: Orthotic inserts, whether custom-made or over-the-counter, can provide arch support and cushioning to relieve tension on the plantar fascia. Supportive footwear with cushioning can help reduce strain during daily activities.
- Brace or Splint: A brace or splint may be used to provide support and prevent movement of the foot. These devices can help stabilize the injured area while allowing some flexibility for healing.
- Walking Boot: A walking boot is a common choice for plantar fascia sprain. It offers better support than a brace and allows for gradual weight-bearing as healing progresses. Walking boots are adjustable and may have removable inserts to accommodate changes in swelling.
Night Splints: Wearing a night splint while sleeping can help keep the plantar fascia stretched, decreasing morning discomfort.
Corticosteroid Injections: In some cases, healthcare providers may recommend corticosteroid injections to reduce inflammation and pain. However, these injections are generally not a first-line treatment and should be used cautiously due to potential side effects and risks.
Surgical management:
Surgical management of a plantar fascia tear is usually considered when conservative treatments have failed to provide relief, and the tear is severe or causing significant functional impairment. Surgery is typically a last resort and is reserved for cases where non-surgical approaches haven’t been successful in alleviating pain and restoring normal foot function.
Plantar Fascia Repair: In cases of severe or complete tears, a surgeon might opt to repair the torn ends of the plantar fascia using sutures. This involves reattaching the tissue to promote healing and restore its functional integrity.
Open Plantar Fasciotomy: An incision is made on the bottom of the foot, close to the heel, during an open plantar fasciotomy. The surgeon accesses the plantar fascia and partially cuts or releases a portion of it to alleviate tension. This reduces strain on the torn area and allows the fascia to stretch more easily. It’s an effective method for relieving pain and improving mobility.
Endoscopic Plantar Fasciotomy: Endoscopic surgery is a minimally invasive approach that uses small incisions and specialized instruments, including an endoscope with a camera. The surgeon creates a small tunnel to access the plantar fascia. With the guidance of the camera, the surgeon can visualize and release the tight or torn portions of the fascia. This approach often results in less scarring and a quicker recovery compared to open surgery.
Ligament Repair or Reconstruction: Surgical repair or reconstruction of damaged ligaments to restore stability to the foot.
A Rehabilitation program after surgery or conservative management:
Importance of Rehabilitation program:
A rehabilitation program after surgery or conservative management for a plantar fascia tear is essential for ensuring a successful and comprehensive recovery.
After Surgery:
- Optimal Healing: A well-structured rehabilitation program aids in proper wound healing, tissue recovery, and scar tissue formation.
- Restoring Function: Specific exercises help regain range of motion, muscle strength, and joint mobility lost due to surgery.
- Preventing Complications: Rehabilitation reduces the risk of complications like muscle atrophy, joint stiffness, and post-operative complications.
- Supporting Surgical Outcome: Active participation in rehabilitation contributes to the success of the surgery and long-term functionality.
- Guided Progression: Gradual exercises and controll movements prevent overexertion, allowing tissues to heal without being stressed excessively.
- Addressing Imbalances: Rehabilitation corrects muscle imbalances and movement compensations that may have contributed to the injury.
- Gait Correction: Gait training ensures that you walk correctly, avoiding any improper mechanics that could re-injure the plantar fascia.
- Restoring Confidence: Rehabilitation boosts psychological well-being by providing a structured plan and visible progress.
After Conservative Management:
- Promoting Healing: Gentle exercises and modalities in a rehabilitation program aid in the healing process of the injured plantar fascia.
- Strengthening: Strengthening exercises target muscles around the foot and ankle, providing stability and preventing re-injury.
- Range of Motion: Controlled exercises maintain or restore joint mobility, preventing stiffness and improving overall foot function.
- Addressing Muscle Imbalances: Rehabilitation addresses any underlying muscle imbalances or weaknesses that contributed to the injury.
- Enhancing Function: Gradual progression in exercises supports a gradual return to daily activities, work, and sports.
- Preventing Recurrence: Rehabilitation educates on proper movement patterns and foot mechanics, reducing the risk of re-injury.
- Long-Term Foot Health: Engaging in a rehabilitation program improves overall foot health and prevents chronic issues.
- Patient Empowerment: A structured program empowers patients by involving them actively in their recovery process.
Physical Therapy:
Physiotherapy modalities are various techniques and tools used by physical therapists to manage pain, reduce inflammation, promote healing, and improve overall function. In the context of a plantar fascia tear, these modalities can play a significant role in your recovery.
- Ultrasound Therapy: Ultrasound involves the use of high-frequency sound waves that create vibrations within tissues. It can help increase blood flow, promote healing, and reduce inflammation in the plantar fascia. The therapist applies a gel to your skin and moves a small ultrasound wand over the affected area.
- Electrical Stimulation: Electrical stimulation involves the application of electrical currents to the skin using electrodes. This can help alleviate pain, decrease muscle spasms, and improve blood circulation. Electrical Stimulation may be used to target specific trigger points or muscle groups.
- Cold Therapy (Cryotherapy): Cold therapy involves the application of ice or cold packs to the affected area. It can help reduce pain, inflammation, and swelling in the plantar fascia. Cold therapy is typically applied for short periods, and the therapist may use techniques like ice massage or ice packs.
- Heat Therapy (Thermotherapy): Heat therapy involves the application of heat to increase blood flow and relax muscles. It can help relieve muscle tension, enhance tissue elasticity, and prepare the foot for therapeutic exercises. Heat might be applied using moist heat packs or other methods.
- Iontophoresis: Iontophoresis is a technique that uses a low-level electric current to deliver anti-inflammatory medications through the skin. It can be used to target inflammation in the plantar fascia and surrounding tissues.
- Laser Therapy: Low-level laser therapy (LLLT) uses low-intensity lasers to stimulate cell function and promote tissue healing. It can be used to target inflammation and pain associated with a plantar fascia tear.
- Shortwave diathermy: It is a therapeutic technique that uses electromagnetic waves to generate heat deep within tissues. It’s sometimes used for conditions like a plantar fascia tear. The heat can help with pain relief, blood flow, and muscle relaxation. However, its effectiveness varies from person to person, and it’s often used alongside other treatments.
Exercises:
Exercises play a crucial role in the rehabilitation of a plantar fascia tear. They help improve flexibility, strength, and stability in the foot and lower leg, promoting healing and preventing future issues. Here are some exercises that may be beneficial for individuals recovering from a plantar fascia tear:
Stretching exercise:

Face the wall and place your hands flat on it at shoulder height to do a wall calf stretch.
Step backward with one foot, ensuring the heel is firmly planted on the ground.
Lean against the wall while maintaining the rear leg straight and bending the front knee slightly.
The calf of the hind leg must expand.
Hold the stretch for 30 seconds.
With the opposite leg, repeat the stretch.
Plantar Fascia Stretch:
With your legs out in front of you, sit down on a soft surface.
Keep your back straight and shoulders relaxed.
Cross the affected leg over the opposite knee, so the ankle of the affected foot is resting on the opposite knee.
Use your hand to gently hold the toes of the affected foot.
If you have difficulty reaching your toes, you can loop a towel or exercise band around the arch of your foot and hold onto the ends.
While holding your toes, gently pull them back toward your shin.
Stretching should be felt in the arch and along the bottom of your foot.
Stop when you feel a comfortable stretch; avoid pushing to the point of pain.
Hold the stretch for about 20-30 seconds while taking slow, deep breaths.
Focus on relaxing and allowing the tension to release.
Release the stretch slowly and gently.
Repeat the stretch for a total of 2-3 repetitions on each side.
Big toe stretch:
The “big toe stretch” is a simple workout that targets the tendons and muscles surrounding the big toe joint. This practice may be beneficial for persons suffering from ailments such as plantar fascia tears since it can assist the toe to become more flexible. The big toe stretch should be performed in the following manner:
Sit with a straight back.
Place one foot’s heel firmly on the ground.
Raise the toes of the same foot while keeping the big toe in contact with the floor.
Slowly and gradually bend your big toe upward (towards the top of your foot) as far as you can comfortably do so. The bottom of your foot should extend somewhat.
Maintain the stretch for 10 seconds.
While maintaining regular breathing, hold the stretch for 15 seconds.
After releasing the stretch, return the big toe to the floor.
Repeat the stretch 5-10 times for each foot.
Achilles Tendon Stretch:
Instructions:
Find a level, sturdy surface to stand on, such as a step, a curb, or a solid platform. You may also use the edge of a step, but make sure you have something nearby to grip onto if you need to keep your balance.
Stand at the surface’s edge, with your feet shoulder-width apart and your heels hanging off the back.
Cling to a nearby item for balance if necessary.
Lower your heels gently towards the ground until they are below the step and your ankles can flex.
Maintain your stretch for 15 to 30 seconds. You should feel a slight pull or strain in your calves and Achilles tendon.
Return to the starting position with caution by elevating your heels.
Repeat the stretch three to four more times.
Range of motion exercise:
Toe Flexion:
Sit or stand with your feet flat on the floor for toe flexion.
Curl your toes softly downward, as if you’re making a fist.
Hold your foot in this posture for 5-10 seconds to feel the bottom of your foot expand.
Wring your toes and relax.
Ten to fifteen times, repeat this stretch.
Toe Extension:
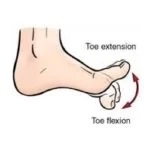
Take a comfortable seat with your feet on the ground.
Maintain a tight grip on your heels while extending all of your toes off the ground.
Hold this stance for 5 to 10 seconds.
Return your feet to the ground.
Ten to fifteen times, repeat this stretch.
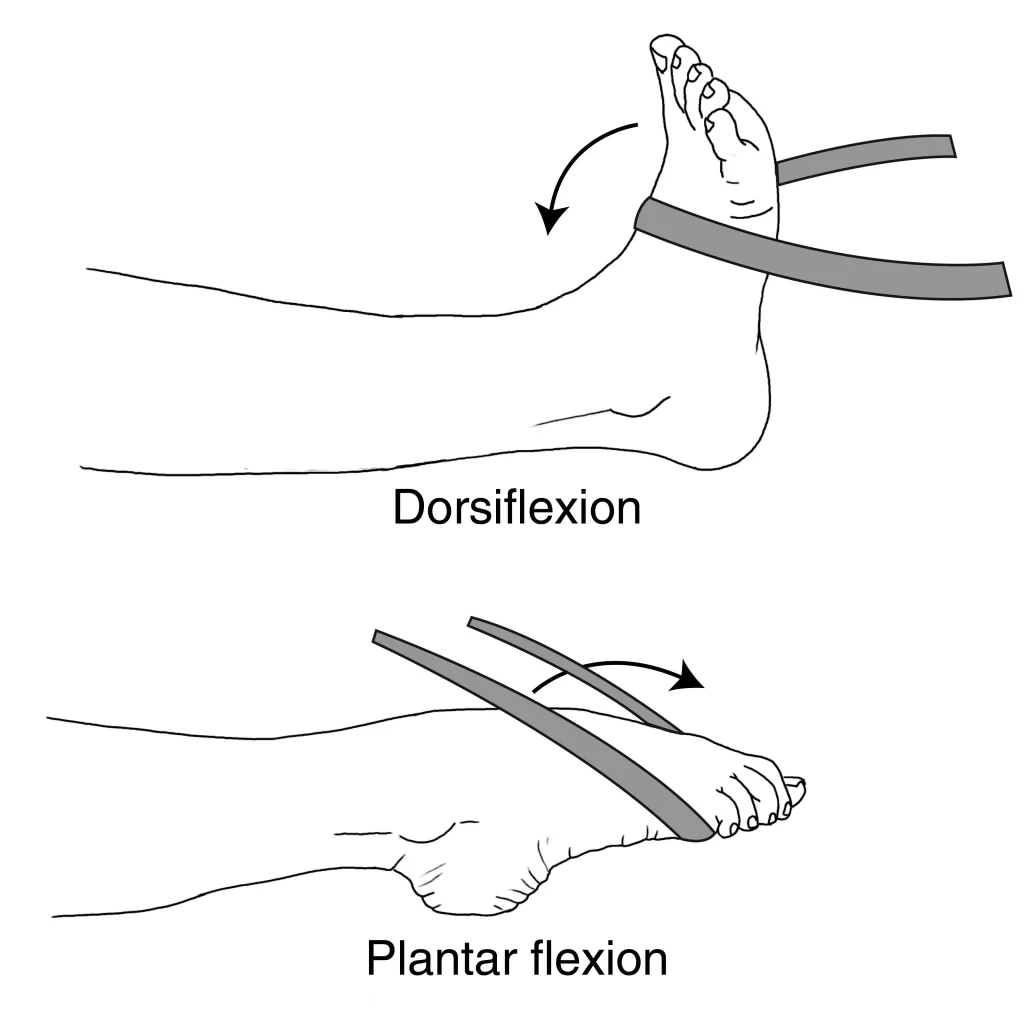
Dorsiflexion:
It is the movement of pulling your toes towards your body or raising the front of your foot off the ground.
This motion is controlled by the muscles at the front of the lower leg, namely the tibialis anterior muscle.
Dorsiflexion is achieved by lifting your toes up towards your shin while keeping your heels on the floor. This motion is performed when you walk and your foot is about to strike the ground.
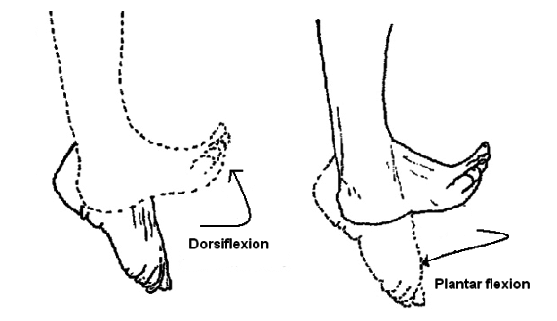
Plantar Flexion:
Plantar flexion is the act of pointing your toes away from your body. Consider standing on your toes.
This action is primarily controlled by the gastrocnemius and soleus muscles of the calf.
Push into the balls of your feet to do plantar flexion.
Toe Towel Scrunches:
Towel scrunches are a simple and effective foot exercise that helps tone the muscles in your toes and the arch of your foot. This is an excellent foot exercise for boosting support, stability, and dexterity. How to scrunch a towel is as follows:
A little towel is a required thing.
Instructions:
Sit on a chair or table and put your foot on the ground.
The little towel should be placed on the ground just in front of your feet.
Fold the towel towards you with your toes. Consider grabbing the towel with your toes and elevating it.
Compress the towel with your toes while still in the contorted posture.
Release the pressure and extend the towel straight out with your feet.
Rep as many times as you can, aiming for at least 15 to 20 scrunches each time.
Ankle circles:
Simple ankle circles exercises are meant to improve ankle flexibility and mobility. They include circling your ankles, which can be beneficial for persons with foot and ankle diseases. Ankle circles increase ankle joint range of motion, maintain joint health, and reduce stiffness. This practice is carried out as follows:
While sitting comfortably on a chair or the floor, extend your legs out in front of you.
Raise one foot off the ground and point your toes ahead, keeping your knee straight.
Begin moving your foot clockwise while rotating your ankle joint.
Rotate your ankle 10 times clockwise in a calm, controlled manner.
After finishing the clockwise circles, go to the anticlockwise direction and construct 10-15 circles there.
Return your foot to the floor, then circle the ankles with the other foot.
Foot Arch Lifts:
Lifting your foot is a quick and efficient way to tone the muscles in your foot’s arch. It can help with foot stability, and balance, and prevent difficulties caused by weak arches. Foot arch lifts are carried out as follows:
Materials required: None
Instructions:

As you sit or stand in a comfortable position, place your feet flat on the ground.
Lift your foot arches to make space beneath the arch while maintaining your heels and toes on the ground.
While holding the lifted stance for a few seconds, concentrate on tightening the muscles in the arch of your foot.
Relax and return your foot to a flat position.
Foot arch lifts should be done 10 to 15 times.
Alphabet Toes (Toe Alphabet):
“Alphabet toes,” often known as “toe writing” or “the alphabet,” is a simple and entertaining foot exercise that can assist improve toe flexibility and dexterity. Throughout this workout, you will “write” the letters of the alphabet in the air using your toes. It’s an excellent way to strengthen the muscles in your toes, which will improve foot mobility and functioning. The directions for the alphabet toes exercise are as follows:
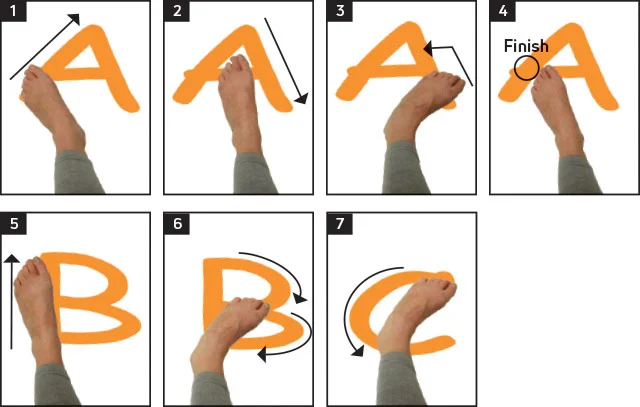
Sit on a chair or on the floor and stretch your legs in front of you.
Lift one foot off the ground while keeping your other foot firmly on the ground.
Begin “writing” the letters of the alphabet in the air with your big toe functioning as a pen.
Make each letter as huge and distinct as possible using only your toes.
Once you’ve finished the alphabet with one foot, turn to the other and repeat.
To ensure that the toe muscles are adequately stimulated, perform the exercise lightly and with control.
Toe Tapping:
Toe-tapping is a short and effective foot workout that can improve ankle mobility, increase blood flow, and engage the muscles in your lower leg and foot. It is a low-impact workout that does not require any particular equipment and can be done almost anywhere. Toe-tapping should be done as follows:
Instructions:
Place your feet flat on the ground while sitting comfortably on a chair.
Lift your toes off the ground while keeping your heel firm.
Begin tapping your toes on the ground as soon as possible.
Continue tapping your toes for 30-60 seconds.
After a short rest, repeat the toe-tapping exercise.
Toe Spreading or splay:

Instructions:
Sit or stand with your foot on the ground.
Allow your feet and toes to relax and return to their natural positions.
Begin the toe-spreading action by actively spreading your toes apart, as though you’re trying to leave as much space between them as possible.
Feel the muscles between your toes lengthen and contract as you maintain the wide position.
Let go of the spread and return your toes to their normal position.
Perform the toe-spreading movement many times.
Toe squeeze:
Take a comfortable seat on a chair or the floor, with your feet level on the ground and your back straight.
Place a stress ball-sized baseball or a folded towel between your feet.
Use your toes to gently squeeze the ball or cloth. Consider gripping or raising the object with your toes.
Hold the squeeze for a few seconds (around 5 to 10 seconds) while retaining hold of the target.
Uncurl your toes and let go of the strain.
Rep the workout 10 to 15 times more.
Figure Eight rotation:
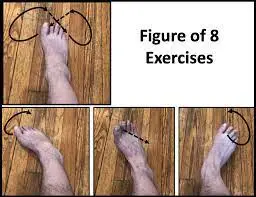
The toe movement exercise is similar to the figure-eight rotation exercise; however, with this exercise, you use your big toe to rotate your toes in a figure-eight pattern rather than a circular one. The increased flexibility of the foot’s toes and fingers is the main advantage of this workout.
For 2-3 sets, repeat 10 times for each toe. Exercises like the Figure-8 rotation are very basic and straightforward.
Foot-screw:
For the leg curl workout, you can squat on the ground. Onto the cushion or ball, let the knee descend outward. Then step up to the threshold.
Utilizing your hand, stabilize the heel. Pull the leg apart by a foot’s breadth by running your right hand down the calf’s threshold at this point.
Now, move your foot a little forward before spiraling to the inside of your foot’s resistance. Then return the leg to its initial position after a few times of screw-like movements. With the other leg, repeat this exercise.
This exercise, which is based on the “leg screw” exercise, works all the muscular groups that support and strengthen the foot muscles. Do three sets of repetitions each day, 15-20 times each.
Strengthening exercise:
Ankle Eversion with Resistance Band:

While seated on a chair, place your feet flat on the ground.
Loop one end of the resistance band around the ball of your foot and hold the other end in your hand.
While maintaining your heel on the ground, evert your foot (move your foot outward) against the resistance of the band.
Hold the position for 5-10 seconds before returning to the starting position.
Repeat the exercises for each foot 10 to 15 times.
Ankle inversion with Resistance Band:
Legs extended in front of you when seated on a chair or a flat surface.
The resistance band’s end should be wrapped around the ball of your foot.
To tighten the band, place the other end in your hand.
Maintain a relaxed gait while pointing your toes straight ahead.
Slowly and gradually shift your foot inside (inversion) against the resistance of the band.
Feel your ankle’s surrounding muscles tighten as you keep your stance inward.
Return your foot to the starting position slowly and steadily.
Move to the second foot after executing the exercise on one foot for the appropriate number of repetitions (for example, 10-15 reps).
Ankle Plantarflexion (Pointing) Resistance Exercise:
- Sit on a chair or a stable surface with your foot securely placed on the floor.
- Attach one end of the resistance band to a stable anchor point and the other end to the front of your foot.
- Keep your feet on the ground and your knee straight.
- Slowly push your foot down against the resistance band, pointing your toes away from your body.
- After one second of holding the contraction, slowly return to the beginning position.
- On each leg, complete 2-3 sets of 15 repetitions.
Ankle Dorsiflexion (Flexing) Resistance Exercise:
- Sit on a chair or a stable surface with your foot securely placed on the floor.
- Attach one end of the resistance band to a stable anchor point and the other end to the top of your foot.
- Keep your knee straight and your toes pointing upwards.
- Slowly pull your foot towards your shin against the resistance band, flexing your ankle.
- After one second of holding the contraction, slowly return to the beginning position.
- On each leg, complete 2-3 sets of 15 repetitions.
Resistance Band Arch Exercise:
Using resistance bands to build up the muscles in your foot’s arch helps improve stability and support. This workout focuses on the intrinsic foot muscles, which are crucial for maintaining appropriate foot alignment and preventing issues like flat feet or overpronation.
While seated on a chair or the floor, extend your legs in front of you.
Double-wrap the resistance band around the balls of your feet.
Tension must be maintained while holding the resistance band’s ends firmly in your palms.
Point your toes outward while extending the resistance band.
Next, buckle the band’s pull while extending your toes back towards you.
Repeat the motion of pointing and flexing.
Marble pick up:
For people who have plantar fasciitis or have had plantar fascia repair surgery, the activity known as “marble pick-up” might be therapeutic. It is a simple foot workout for increasing flexibility and foot muscle strength. This exercise may help improve foot functioning.
The marble pick-up exercise is performed as follows:
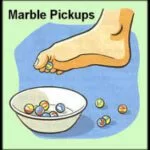
While seated in a chair, set a small bowl or container filled with marbles or other small balls on the floor in front of you.
Remove your shoes and socks to get a secure grip on the marbles when barefoot.
Pick up marbles: Place another bowl or container next to the one containing the marbles and pick up each marble one at a time with your toes.
Picking up and moving the marbles should be repeated for 5 to 10 minutes, or for as long as you feel comfortable.
After you’ve done your workout, stretch and rest your feet.
This exercise can help to strengthen the intrinsic muscles of the foot, which are important for maintaining good foot arches and support. It may also aid with control and coordination.
Doming:
Targeting these anterior foot muscles can be accomplished by doing a leg of the foot doming exercise.
You may do this by attempting to move the big toe toward the direction of the heel and forming the “dome” under the foot as demonstrated above.
It’s difficult to grip the dome while keeping your toes on the ground. This is similar to the test mentioned before in terms of generality. Try to maintain your ankles and feet in a neutral position and avoid moving your toes.
Depending on how ambitious you are, you may perform this exercise while sitting, standing, or standing on one leg before progressing to additional motions (quads and pull-ups).

Your toes get stronger with this stretch, and your arches raise (or “dome”). Place your feet on the floor and take a seat. With your toes, try to grasp the ground. Make sure you’re holding the object rather than merely curling your toes.
For between five and ten seconds, maintain the dome position. Do three sets of repetitions each day, 15-20 times each.
Heavy Resistance Training should be added as the period progresses:
Practitioners of progression frequently give patients a regulated, controlled amount of weight that is pretty low. Resistance band exercise has several advantages for patients since it strengthens the muscles in their feet. This progression exercise is an additional method to strengthen the muscles in your feet.
Eccentric Calf Raise (Heel Drop):
Exercise: Eccentric Calf Raise (Heel Drop)
A step or a sturdy elevated platform (such as a stair) is necessary.
Instructions:
While standing, keep your heels off the back of the step and the balls of your feet on the step. Your toes should be directed forward, and your feet should be hip-width apart.
Cling to a nearby wall or railing for support if required.
Lift both heels by leaning into the balls of your feet.
Then, gently lower your heels to the step’s level. It is critical to descend gently and cautiously.
Allow your heels to fall as much as they can without causing pain or discomfort. Your calf muscles should be stretched.
After lowering your heels as far as they will go, gently pull them back up to the starting position with the opposing foot.
Slowly and methodically do 10 to 15 repetitions of the eccentric lowering action.
Toe Raises:
Take a comfortable seat with your feet flat on the ground.
Keep your heels firmly anchored while raising your toes off the floor.
Before lowering your toes, hold for a short period of time.
Repeat a number of times.
Calf raises:
The calf muscles may be worked quickly and effectively with calf lifts. Calf lifts are performed as follows:
With a sturdy surface nearby for support, stand with your feet hip-width apart. Raise your heels as high as you can as you ascend onto the balls of your feet. Retract your heels gradually. Repetition sets should be done.
Tip-toe walking:
Set up a clear space for tip-toe walking or draw a straight line on the ground. On tiptoe, walk a straight line.
Toes and heels should come together. Select a location in front of you and concentrate on maintaining your balance as you go. Make a move.
Put the opposite foot’s toe directly behind the heel of the first foot. twenty times. If you feel insecure, perform this exercise next to a wall or ask a friend to assist you. The advantages of walking on these toes include calf muscle strengthening and stretching of the often contracted extensor muscles.
Sand walking:

Walking barefoot through the sand helps to stretch and strengthen your toes and feet while also giving your calves a terrific workout. Make sure to turn back before you tire since walking on sand is more exhausting than walking on concrete surfaces.
For instance, search for sand at a beach, desert, or volleyball court. It is important to remove your shoes and socks before beginning the walk. This enhances your body’s ability to move.
then go for a three to five-minute stroll. You may add walking for longer periods of time to the progression period over time.
Soft Tissue Mobilization:
Manual techniques such as massage, myofascial release, and trigger point therapy can help improve blood circulation, reduce muscle tension, and enhance tissue mobility in the foot and calf muscles.
Massage:
Ball massage:
Choose the ball that feels the most comfortable for you and the region you are targeting. For more intense pressure, use a smaller, denser ball, like a lacrosse ball. For lighter pressure, use a larger, softer ball, like a tennis ball.

Find the area: Identify the stiff, tight, or painful area of your body. For ball massages, the back, neck, shoulders, hips, glutes, and feet are frequent areas.
Apply pressure by positioning the ball where you want it and then gently pressing your weight on it. This may be accomplished by lying on the floor or resting against a wall.
Once the ball is in place, you may choose to roll it back and forth or hold it in a specific spot that feels particularly sensitive or stiff. Allow the pressure to enter the muscle for a few seconds.
As you apply pressure, take a deep breath and try to relax your muscles. Try not to hold your breath.
Reduce the pressure if too much body weight is being used to support the ball. If you need a bit more pressure, learn a little more about the ball.
Give each area between one and two minutes, gently rolling the ball to different areas to massage the entire area you desire.
Foot rolling with a frozen water bottle:
While sitting on a chair or the floor, your feet should be out in front of you.
Lay down a tennis ball or a frozen water bottle.
As you roll your foot over it, use your body weight to gently press the object. Move the item from the ball of your foot to the heel, as well as from side to side.
Pay special attention to any painful spots or unpleasant places, and spend extra time rubbing them to relieve stress.
Roll your feet for a minute or two on each foot.
You might also try twisting your entire foot, focusing on the arch and the area near your toes.
Extra pressure applied to a tight or sore spot can assist, but avoid using too much pressure or inflicting misery.
Repeat the foot rolling as needed to maintain foot health and relieve tension.
Heel-of-hand massage:
Place one foot up where your hand can reach it while sitting in a chair or on a bed.
From the heel to the toes of your opposite hand, press down on the bottom of your foot.
Begin with longer strokes with low pressure, then gradually lengthen and increase the pressure. Use your entire weight to provide more pressure while leaning in for the massage.
In order to release the fascia tissue, repeatedly cover the top of your foot.
This massage can also be performed with a lightly clenched fist.
Balance and Proprioception Training:
Balance and proprioception training are important components of a comprehensive rehabilitation program for managing plantar fascia discomfort and preventing injuries. Proprioception refers to the body’s ability to sense its position in space and its movements. Improving balance and proprioception can enhance stability, reduce the risk of falls, and promote better control of movement, ultimately benefiting foot and lower leg health.
Here are a few exercises are:
1. Single-Leg Balance:
- With your foot firmly placed on the ground and your knee slightly bent, stand on one leg.
- To keep your balance, contract your core muscles.
- After maintaining this posture for 20–30 seconds, move to the other leg.
- As you progress, try closing your eyes or standing on an uneven surface, such as a foam pad, to challenge your balance further.
2. Heel-to-Toe Walk:
- Walk in a straight line, placing the heel of your front foot directly in front of the toes of your back foot.
- This exercise mimics the tightrope walking movement and challenges your balance and proprioception.
3. Wobble Board or Balance Disc:
- Stand on a wobble board or balance disc with one or both feet.
- The unstable surface challenges your balance and engages the muscles that stabilize your ankles.
- Perform exercises like shifting your weight from side to side or in a circular motion.
4. Toe Taps:
- One knee should be slightly bent as you balance on it.
- Gently tap your other foot forward, to the side, and behind you while maintaining your balance.
- This exercise helps improve coordination and proprioception.
5. Tandem Stance:
- Stand with one foot, heel-to-toe.
- Maintain this stance for 20-30 seconds, then switch the position of your feet.
- Focus on engaging your core and using your ankle and foot muscles for stability.
6. Dynamic Balancing Exercises:
- Perform exercises like leg swings, hip circles, or ankle circles to challenge your balance and proprioception while in motion.
7. Eyes-Closed Balance:
- Perform any of the balance exercises with your eyes closed to rely solely on your proprioceptive senses.
Important Tips:
- Start with exercises that are appropriate for your present level of stability and balance.
- Perform these exercises on a safe surface and near sturdy support (such as a wall or chair) to grab onto if needed.
- Gradually increase the difficulty and duration of the exercises as your balance improves.
- Consistency is key. Include balance and proprioception training in your routine a few times a week.
- If you have an existing injury or medical condition, consult a doctor before starting any new exercise program.
Balance and proprioception training can not only aid in managing plantar fascia discomfort but also enhance overall lower limb function and reduce the risk of future injuries.
Gait training:
Gait training is a crucial aspect of rehabilitation for individuals recovering from plantar fascia discomfort or injuries. Proper gait (walking) mechanics can help alleviate strain on the plantar fascia, promote healing, and prevent the recurrence of issues. Working with a physical therapist is recommended for personalized gait training.
Heel-to-Toe Rocker:
People who have ankle sprains or plantar fascia injuries are sometimes advised to wear shoes with a heel-to-toe rocker sole. This kind of shoe construction can ease the strain and motion on the midfoot region, resulting in a more fluid and relaxing stride while facilitating healing.
Place your feet hip-width apart while standing straight. Move your weight first from your heels to your toes. Focus on fluidly rolling from your heel to your foot and then pushing off with your toes as you gradually transition to a forward walking motion.
Step-Ups:
Locate a low platform or step. Bring your damaged foot up to meet your uninjured foot first as you ascend. Put your injured foot back down first, then your healthy foot. The coordination and muscle needed to climb and descend stairs or curbs are improved by this workout.
Mini Lunges:
Step one: Stand with your feet hip-width apart. With the foot that wasn’t hurt, advance. Lower your body by bending both knees. Maintain an elevated front knee over your ankle. The back knee is protruding above the surface. To stand, push off your front foot. Then switch sides once again. Start by performing a few reps on each leg. This exercise encourages balance and optimum stride length.
Walking in Slow Motion:
Walking slowly might help you become more aware of your gait mechanics. Be sure to push off from your toes, roll through the foot, and land on your heel. You may intentionally improve your walking pattern by doing this practice.
Marching in Place:
While standing still, raise your knees high in a manner akin to a march. Instead of dragging your feet on the ground, concentrate on raising them from the midfoot region. Strength and flexibility in the foot area are improved by this workout.
Maintaining One Leg Balanced:
Lift your afflicted foot off the ground while standing on your healthy foot. Try to maintain your equilibrium for 30 to 60 seconds. Stability and proprioception are strengthened by this workout.
Tandem walking:
Put one foot in front of the other and go forward in a straight line as if you were walking a tightrope. Your balance and coordination will be put to the test throughout this exercise.
Walking backward:
Short distances of backward walking while rolling from heel to toe. This practice can assist reinforce the right foot mechanics and position.
Biofeedback and Neuromuscular Re-education:
These techniques involve using specialized equipment to provide feedback on muscle activity and movement patterns. They can help you learn to engage specific muscles properly and retrain movement patterns to reduce strain on the plantar fascia.

Taping or Strapping Techniques:
Kinesiology tape or athletic tape might be applied to the foot to provide support, reduce strain on the plantar fascia, and promote proper biomechanics. The therapist will use specific taping techniques to address your condition. Taping techniques can provide temporary support and relief for various foot conditions, including plantar fasciitis or minor plantar fascia discomfort. Below are two commonly used taping techniques that can help alleviate symptoms.
- Low-Dye Taping Technique 2. Arch Taping Technique
Gradual Return to Activities:
As you progress through physical therapy, your therapist will guide you in safely reintroducing activities that involve your feet, such as walking, running, and sports. They will ensure that you return to these activities gradually and with proper biomechanics to prevent re-injury.
How to prevent plantar fascia injury?
Preventing a plantar fascia injury involves adopting a combination of lifestyle habits, footwear choices, and proper self-care practices. There are some effective strategies to help prevent plantar fascia injuries:
1. Choose Supportive Footwear:
- Put on footwear with appropriate shock absorption, cushioning, and arch support
- Opt for footwear with a wide toe box to prevent crowding and pressure on the toes.
- Avoid wearing worn-out or unsupportive shoes, especially for activities that involve prolonged standing or walking.
2. Gradual Activity Progression:
- To give your body time to adjust, gradually increase your workouts’ duration, frequency, and intensity.
- Avoid sudden spikes in activity, which can put excessive strain on the plantar fascia.
3. Warm-Up and Stretching:
- Warm up your muscles with gentle exercises before engaging in more intense activities.
- Incorporate regular stretching into your routine, targeting the calf muscles, Achilles tendon, and plantar fascia.
4. Foot Strengthening Exercises:
- Perform exercises that target the muscles of the feet and lower legs to enhance their strength and stability.
- Toe scrunches, calf raises, and resistance band exercises can be helpful.
5. Maintain a Healthy Weight:
- Maintain a healthy weight through balanced nutrition and regular exercise to reduce strain on your feet.
- Excess body weight can contribute to overloading the plantar fascia.
6. Proper Foot Mechanics:
- Pay attention to your walking and running gait. Avoid overpronation (excessive inward rolling of the foot) or supination (excessive outward rolling).
- Use proper footwear and consult a podiatrist if you notice any abnormal gait patterns.
7. Cross-Training:
- Engage in a variety of physical activities to avoid overuse injuries and ensure balanced muscle development.
8. Supportive Inserts or Orthotics:
- If recommended by a healthcare professional, use orthotic inserts to provide additional arch support and cushioning.
- Custom orthotics can be tailored to your specific foot mechanics.
9. Adequate Rest and Recovery:
- Allow adequate time for rest and recovery between high-impact activities.
- Avoid pushing through pain by paying attention to your body.
10. Maintain Proper Hygiene:
- To avoid fungus, keep your feet dry and clean.
- Trim toenails regularly to prevent ingrown nails that can cause discomfort.
11. Avoid Hard Surfaces:
- Limit activities on hard surfaces, especially if you’re not accustomed to them.
- Gradually adapt to different surfaces to avoid sudden stress on the feet.
12. Avoid Excessive High Heels:
- Limit wearing high-heeled shoes, which can alter foot mechanics and strain the plantar fascia.
- Choose footwear with low heels and adequate arch support.
13. Flexibility and Mobility Training:
- Engage in activities that promote overall flexibility, such as yoga or Pilates.
- Maintain flexibility in your lower limbs to reduce the risk of overloading the plantar fascia.
14. Regular Foot Care:
- Pay attention to any changes in your feet, such as pain or discomfort.
- Address minor discomfort promptly to prevent it from escalating into a more serious injury.
By adopting these preventive measures and being attentive to your foot health, you can significantly reduce the risk of developing a plantar fascia injury. If you’re unsure about your risk factors or need guidance on specific prevention strategies, consider consulting a doctor, especially a podiatrist or physical therapist.
Home remedies:
While home remedies can provide relief for mild cases of plantar fascia discomfort, it’s needed to note that if you suspect a plantar fascia tear or experience severe pain, consulting your doctor is important for proper assessment & treatment. Here are some home remedies that might help alleviate plantar fascia discomfort:
1. Rest and Ice:
- Rest the affected foot to avoid further strain.
- Apply ice to the painful area for about 15-20 minutes every few hours to help reduce inflammation and pain.
2. Stretching Exercises:
- Gently stretch the calf muscles, Achilles tendon, and plantar fascia.
- Perform exercises like calf stretches against a wall and plantar fascia stretches to maintain flexibility.
3. Massage:
- Use a tennis ball, golf ball, or a frozen water bottle to roll your foot gently over it, applying pressure to the sore areas.
- This self-massage can help release tension in the muscles and fascia.
4. Arch Support Inserts:
- Over-the-counter arch support inserts or orthotics can provide extra cushioning and support for your feet.
- Choose inserts that match your arch type and foot mechanics.
5. Footwear:
- To lessen stress on the plantar fascia, use shoes with supportive arches and enough of padding.
- Avoid walking barefoot on hard surfaces.
6. Night Splints:
- Night splints can help keep your foot in a dorsiflexed position overnight, which can help alleviate morning pain.
- Consult a healthcare professional before using a night splint.
7. Taping or Strapping:
- Low-Dye taping techniques can provide temporary support and relief during activities.
- Consult a physical therapist for proper taping techniques.
8. Epsom Salt Soak:
- Soak your feet in warm water with Epsom salt for 15-20 minutes to help relax muscles and reduce discomfort.
9. Gentle Exercises:
- Perform low-impact exercises like swimming or cycling to maintain cardiovascular fitness without putting excessive strain on the feet.
10. Maintain a Healthy Weight:
- Excess body weight can contribute to strain on the plantar fascia.
- Pursue a healthy weight by eating a balanced diet and engaging in frequent exercise.
11. Avoid High-Impact Activities:
- Limit activities that involve high-impact movements, especially during the acute phase of discomfort.
12. Adequate Foot Care:
- Keep your feet clean, dry, and moisturized to prevent fungal infections or dry skin that can exacerbate discomfort.
13. Anti-Inflammatory Diet:
- Include foods rich in omega-3 fatty acids, antioxidants, and anti-inflammatory properties, such as fatty fish, nuts, fruits, and vegetables.
14. Foot Elevation:
- Elevate your feet when resting to help reduce swelling and promote blood circulation.
FAQs:
A plantar fascia tear refers to the partial or complete rupture of the plantar fascia, a thick band of connective tissue that runs along the bottom of the foot. It can result from overuse, injury, or other factors, leading to pain and discomfort in the heel and arch of the foot.
Common symptoms include sharp heel pain, especially with the first steps in the morning, pain that worsens with activity, swelling, tenderness, and difficulty walking or standing for extended periods.
Diagnosis involves a physical examination, medical history review, and possibly imaging tests such as X-rays or ultrasound. Special tests and clinical assessments can help confirm the diagnosis.
It is critical to maintain excellent foot health after recovery. This includes regular stretching, strengthening exercises, wearing appropriate footwear, and avoiding activities that could strain the plantar fascia excessively.
You can gradually reintroduce sports and exercise after getting clearance from your healthcare provider. However, it’s important to ease back into activities and pay attention to any signs of discomfort
A balanced diet rich in nutrients, especially those promoting bone and tissue health, can support the healing process. Nutrients like calcium, vitamin D, and protein are important for recovery.
Taping techniques, such as low-Dye taping, can provide temporary support and help alleviate pain during activity. Consult a physical therapist to learn proper taping techniques.
While alternative therapies like acupuncture or chiropractic care might provide relief, it’s important to consult a healthcare provider first and ensure that these therapies are used in conjunction with evidence-based treatments.
Minor tears might heal with rest, conservative treatments, and proper care. However, severe tears or those that don’t improve with nonsurgical methods may require medical intervention.
Treatment options include rest, ice, pain management, physical therapy, orthotics, taping, supportive footwear, and in some cases, surgery.
Surgery is typically considered when conservative treatments have not provided relief after a significant period. Surgical procedures aim to repair torn fascia and may involve releasing tension or removing damaged tissue.
Yes, physical therapy is highly important for healing. Therapeutic exercises, stretching, manual therapy, and modalities like ultrasound or soft tissue mobilization can aid healing, improve function, and prevent recurrence.
Recovery times vary according to the degree of the tear and the selected course of therapy. Mild tears might heal in a few weeks, while more severe cases could take several months.
Taking preventive measures such as wearing proper footwear, stretching before exercise, maintaining a healthy weight, and gradually increasing activity levels can reduce the risk of developing a plantar fascia tear.
It’s important to consult a healthcare provider before resuming exercise. Depending on the severity of the tear, certain activities may need to modify or avoided during the healing process.
Over-the-counter arch supports or orthotics can provide some relief, but it’s recommended to consult a healthcare professional for proper guidance. Custom orthotics might be more effective in addressing specific foot mechanics.
If you experience severe pain, or difficulty walking, or if conservative treatments aren’t helping after a few weeks, it’s advisable to seek medical attention for a proper diagnosis and treatment plan.
Avoiding actions that make the discomfort worse is crucial. While walking is usually possible, you might need to modify your gait or use crutches to reduce pressure on the affected foot. Consult a healthcare provider for guidance.
Plantar fascia stress can be decreased by wearing supportive shoes that have enough arch support and cushioning. Avoid flat or unsupportive footwear during your recovery.
Nonsteroidal anti-inflammatory medications (NSAIDs) over the counter can use to treat pain and inflammation. Consult your doctor before taking any drug, though.