Fat Pad Syndrome
Table of Contents
What is Fat Pad Syndrome?
Fat Pad Syndrome, also known as Hoffa’s Syndrome, is a painful condition caused by inflammation and irritation of the fat pad located under the kneecap. This can lead to knee pain and difficulty with normal activities.
- A prevalent cause of anterior knee pain, also known as Hoffa’s illness, fat pad syndrome, or soffits, is an acute or chronic inflammation of the infrapatellar fat pad (IFP). Albert Hoffa made the first official diagnosis of fat pad syndrome in 1904.
Anatomy/Biomechanics
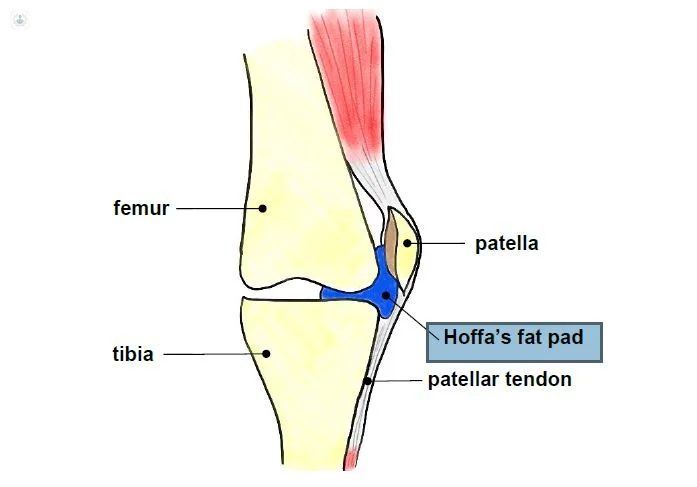
- The IFP is a mass of adipose tissue located in the anterior knee compartment that is extra synovial but lays intracapsular. (extra-articular). The IFP promotes patellar stability, distributes pressure across the patellofemoral joint, and allows for flexible deformation of the knee joint. The IFP’s relatively high nerve density suggests that it may also function as a mechanoreceptor/proprioceptor.
Boundaries
- superiorly by the patella’s inferior pole and the alar folds.
- the anterior tibia, intermeniscal ligament, meniscal horns, and infrapatellar bursa on the inferior side.
- The patellar tendon, patellar ligament, and joint capsule are located anteriorly.
- by the synovial membrane, intercondylar notch, and femoral condyles posteriorly.
Attachments
- the ligamentum mucosal, the anterior horns of the menisci, and the intercondylar notch
- the patella tendon’s proximal end
- the patella’s inferior pole
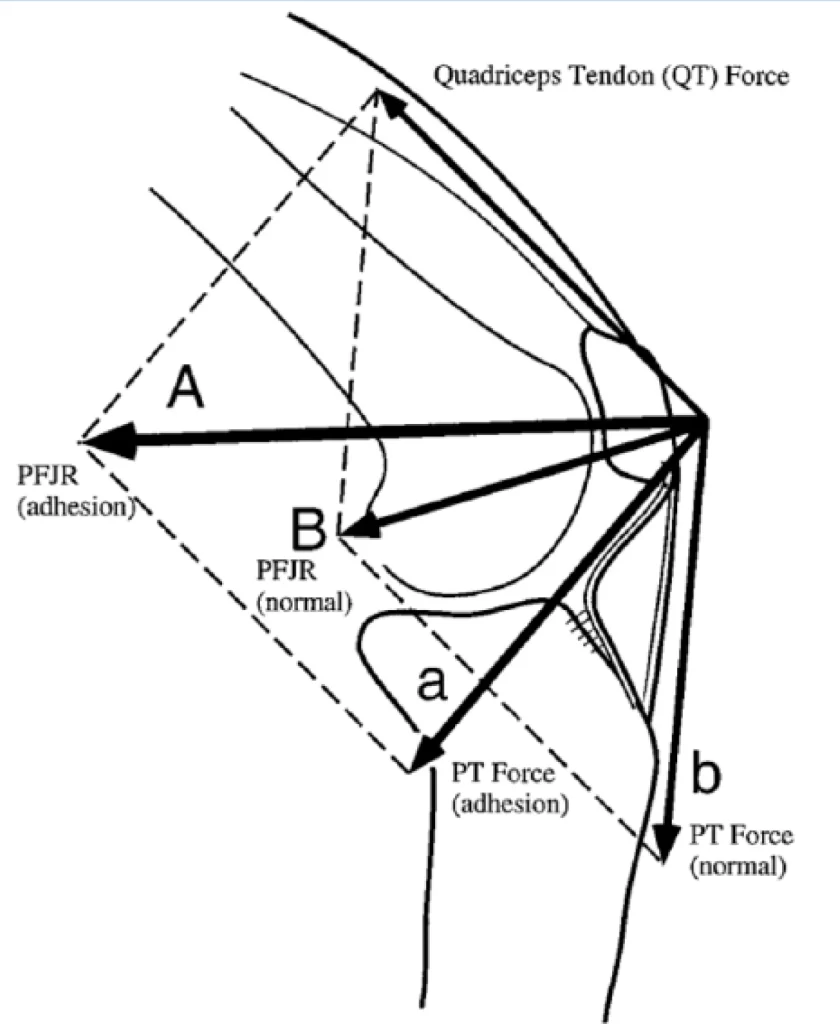
- Photo of the Infrapatellar Fat Pad Biomechanics
- The IFP, which is mostly innervated by the posterior tibial nerve, can cause both localized and excruciating knee pain. This may be explained by the presence of type Via nerve terminals, which may be stimulated by chemical pain mediators or mechanical deformation. When the infrapatellar fat pad is inflamed, substance P-nerve fibers are also present in people with anterior knee pain. Some authors thought the fat pad to be a crucial feature in patellar retinopathy and osteoarthritis as a potential cause of inflammation and pain.
- dynamic structure, the IFP. Throughout the knee ROM, it changes the location, pressure, and volume. The supernatural region of the fat pad relaxes, expands freely, and slides posteriorly as the knee bends. The IFP is situated in extension between the quadriceps tendon and lateral patella facet. As a result, extension is linked to the symptoms that are most frequently reported. But it can also be observed in knee flexion, where the entrapped IFP between the patella tendon and anterior femur causes pain.
- Gliding between the femoral condyles and the joint capsule is made easier by IFP. When there is adhesion in the fat pad, the patella and patellar tendon’s location can vary, changing the knee’s mechanics. As a result, the extensor mechanism’s efficiency is compromised, decreasing the effective moment arm and increasing the demand on the quadriceps to generate the same amount of knee extension force. Patellar mobility is impacted by reduced patellar tendon length, which also provides resistance to lateral translation at full extension.
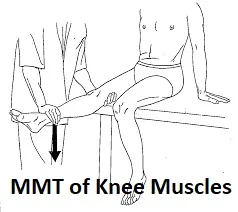
- A study found that anterior knee discomfort was associated with decreased medial and lateral vastus muscle motor unit coordination. Another study found that after injecting the fat pad with painful, hypertonic saline, the quadriceps activated substantially later and contracted at a lower amplitude. The fat pad’s inhibition led to a rise in patellofemoral loading and a decrease in quadriceps activation. Further research is necessary to determine the precise relationship between fat pads and knee biomechanics.
Metabolic influence of the Infrapatellar fat pad
- Early research suggested that the fat pad was a lubricant structure that aided synovial fluid flow within the joint. The IFP’s intricate neurovascular has since made it evident that it produces more complicated functions.
- Many inflammatory mediating chemicals linked to OA are thought to be produced by the IFP. IFP is primarily an adipose tissue, which is renowned for its pro-inflammatory effects on fatty acids. Immune cells, another possible source of inflammatory mediators, are also stored in adipose tissue. Additionally, a study revealed that IFP secretes IL-6 and its soluble receptor, sIL-6R, actively and at considerably higher levels than other adipose tissues.
- There is evidence that IFP releases mesenchymal stem cells.
- IFP has been discovered to release mesenchymal stem cells with increased chondrogenic activity, however, more research is needed to confirm this discovery.
- It has also been suggested that IFP regulates the release of collagen and pro-inflammatory cytokines linked to higher BMI as well as glycosaminoglycan, a source of reparative cells.
- In a study by Duran et al, it was discovered that a patellar cartilage lesion results in a decreased IFP volume.
Physiology/Clinical Illustration
- About the progression of fat pad syndrome, little is known. IFP is subject to mechanical load because of its anatomical position, especially during extension. Hypertrophy results from overuse or recurrent micro-injuries from accidents or sports. If the fat pad doesn’t heal, it may develop a persistent inflammation that, if left untreated, could lead to fibrosis and ossification.
- Jumping sports and ligamentous laxity is also thought to be risk factors for Hoffa’s illness, which primarily affects young women.
Diagnostic and physical examination
- The inflammatory fat pad is frequently greater in size and is firm, puffy, and easily felt. You can perform the Hoffa test. To avoid provoking discomfort in surrounding structures and the development of false findings, Krumar et al. suggested modifying Hoffa’s test. This position merely intensifies pain in the inflamed fat pad.
- It is necessary to glide the patella in all four directions to detect adhesion or mobility restriction during knee movement, especially in hyperextension. (medially, laterally, superiorly, and inferiorly). Pain during hyperextension is a major indicator of an inflamed IFP.
- The goal of the examination should also be to rule out any further radiating diseases, especially from the hip and spine.
Imaging
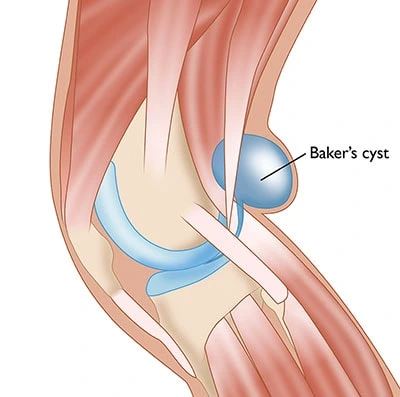
- MRI
- Edema of the superior/posterior fat pad
- Inflamed infrapatellar bursa
- History of trauma
- Dynamic sonographic assessment
Treatment
- The use of tape, physical therapy, non-steroidal anti-inflammatory medicines, injections of local anesthetics, and/or corticosteroids are among the conservative treatments that have been reported to reduce symptoms. Surgery can be the next course of action if these therapies are ineffective.
- Local anesthetic and steroid injections performed for diagnostic and therapeutic purposes into the fat pad immediately reduced pain and restored movement.
- Arthroscopic removal Improvements in the Lysholm knee score and Cincinnati rating system were seen in two investigations.
- Following House and Connel’s ultrasound-guided alcohol ablation, VAS scores improved on average by 4.83.
Acute Fat Pad Syndrome Treatment
- This typically happens during knee surgeries due to arthroscopic equipment, falls, or direct knee damage.
- To relieve immediate discomfort, ice massage is highly helpful. Taping could then be applied to relieve pressure on the fat pad.
- Avoid wearing flat shoes to reduce IFP loading.
- Encourage the patient to refrain from provocative behavior until the acute symptoms go away.
Chronic Fat Pad Syndrome Treatment
- Typically, there has been no prior trauma.
- To lessen the IFP burden, biomechanical anomalies like excessive hyperextension should be addressed.
- A somewhat raised shoe is recommended to treat hyperextension.
- In this phase, movement awareness and education are crucial.
- Do exercises to straighten your knees.
- Stretching the quadriceps and the anterior hip has been shown to reduce the symptoms of IFP restriction.
- High BMI and obesity have a strong effect on fat pad syndrome and knee OA. The impact of a weight loss program (exercise and/or nutrition) on the IFP was examined in an 18-month RCT. The study found that weight loss and changes in body fat %, usually attained by combining exercise and diet, resulted in a considerable reduction in the IFP volume.
FAQs
Which therapy works best to relieve fat pad impingement?
In most cases, ice — lots of ice — will help reduce the swelling caused by the impingement. The conventional recommendations include rest, over-the-counter anti-inflammatories, and strength- and flexibility-building activities. To prevent putting pressure on the fat pad, the area may occasionally be taped.
How long does it take for fat pad syndrome to recover?
Initial healing can take 8–12 weeks, while complete recovery can take 3–6 months. If neglected, symptoms may come back if you resume your regular activities before completing a suitable rehabilitation course.
Is heel fat pad syndrome avoidable?
Always put on shoes with sturdy soles and adequate cushioning.
Limit the amount of time you spend engaging in weight-bearing, high-impact activities (including running, basketball, and gymnastics) to give your heel pad time to recuperate.
keep a healthy weight.Why does fat pad syndrome occur?
One of the most typical reasons for heel discomfort in adults is heel fat pad syndrome, which is brought on by the gradual degradation of your heel pad over time. The tissue in your heels may wear down more quickly as a result of additional variables that put additional pressure on the fat pad in your heel.
What symptoms and signs are associated with fat pad syndrome?
Anterior knee pain, frequently retro patellar and infrapatellar, are signs of fat pad syndrome. Patellofemoral crepitus may be evident when the knee is loaded during activities including jogging, jumping, and negotiating stairs. With inflamed IFP, effusion and reduced ROM are frequently observed.