Metacarpal Fracture
Table of Contents
Introduction
A metacarpal fracture is a type of bone fracture that occurs in one or more of the metacarpal bones in the hand. The metacarpals are the long bones that make up the middle part of the hand, connecting the wrist bones (carpals) to the bones of the fingers (phalanges).
Fractures of the metacarpal bones can be caused by various factors, including direct trauma to the hand, such as a punch or a fall, or indirect trauma, such as twisting or crushing injuries. Sports-related injuries, motor vehicle accidents, and occupational accidents are common causes of metacarpal fractures.
The severity of a metacarpal fracture can vary depending on the location and type of fracture. The metacarpals are numbered from one to five, starting with the thumb (first metacarpal) and ending with the little finger (fifth metacarpal). Fractures can occur anywhere along the length of the bone, including the head, neck, shaft, or base.
Hand fractures are expected in the overall population with a comparative tendency noticed in contact-sport athletes (For example, boxers, and football players) and manual laborers
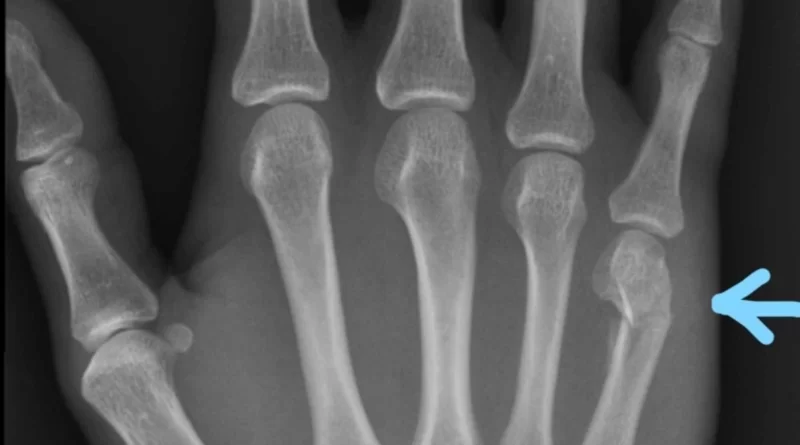
A metacarpal fracture
- Is a fracture of one of either hand’s five metacarpal bones.
- Are the same in nature type as already-existing fractures of the head, neck, shaft, and base (thereby beginning at the metacarpal phalangeal joint and working their way proximally)
- Boxer fracture is another term for a fracture of the fourth or fifth metacarpal, one of the most typical metacarpal fractures.
- The means of this trauma range from axial loading forces to direct hit to the posterior hand
Clinical Anatomy
The metacarpals are a group of long, thin bones that are located between the phalanges of the fingers and the wrist’s carpal bones.
- Individually is formed of a base, shaft, and head.
- Carpal bones are articulate with the proximal bases of the metacarpals
- The lower heads of the metacarpals communicate with the proximal phalanges and construct the knuckles
- The shortest and thickest of these bones is the first metacarpal.
- The third metacarpal is determined by a styloid process on the outer aspect of its base.
- Soft tissues normally concerned with fractures possess cartilage, joint capsule, ligaments, fascia, and posterior hood fibers.
- With intense polytrauma conditions, the tendons and nerves neighboring the fracture may likewise be damaged.
Metacarpal fractures commonly happen secondary to a direct hit or slip straight onto the extended hand.
Causes of Metacarpal Fracture
- These fractures typically happen during athletic activities, especially in contact sports. Practically one-fourth of patients happen during athletic moments.
- Sporting damage is continually the main reason among more youthful patients
- Work-related damages are frequently the reason in middle-aged patients
- Falls are generally the reason for the geriatric.
- Fifth metacarpal fractures usually happen secondary to hitting a wall or different solid thing(because of this the eponym, “boxer’s fracture”)
Hand Fractures
- Makeup almost forty percent of all critical hand trauma
- Comprise approximately twenty percent of almost all fractures happening below the elbow
Metacarpal Fractures
- Normally happens in patients aged ten to forty years
- Males are more probable to be involved than female
- Young males maintain metacarpal fractures secondary to a hitting cause or a direct hit to the hand
- Aged women maintain these damages secondary to a low-impact fall.
- From the ulnar to the radial aspect of every finger’s metacarpal bone, there is a rise in the average number of fractures.
- Second metacarpal fracture rates are lower compared to rates for fifth metacarpal fractures.
- Bennett fracture is the most common fracture concerning the base of the thumb. This fracture was determined to be an intra-articular fracture that divides the palmar ulnar side of the first metacarpal base from the left first metacarpal.
The fractures of the metacarpals can be separated into three pieces.
- The first, neck fractures, happen frequently when an individual hits another individual or object like a wall. In the majority of conditions, operative management is not necessary to manage this circumstance.
- The metacarpal shaft fractures are usually created by longitudinal compression, torsion, or direct hit. They are characterized by the formation of their individual fracture type and can be separated into transverse, oblique, spiral, and comminuted.
- Metacarpal base fractures are very uncommon and have minimal results due to the movement of the joint being little. More familiar are the fractures of the base of the fifth digit and are the consequence of a longitudinally directed force
Symptoms of Metacarpal Fracture
Patients with metacarpal fractures commonly have complaints of the following below:
- Pain
- Swelling
- Ecchymosis (bruise)
- Restriction of motion
- Deformity – Knuckle asymmetry can be followed, and the knuckle may seem to be neglected.
- Finger misalignment can also be mentioned.
- Axial compression of the extended finger is associated with a head of the metacarpal fracture and causes excruciating pain.
- In a fracture of the metacarpal base, motion of the wrist or longitudinal compression exacerbates the pain.
- Any fracture of the metacarpal angulation may produce a pseudo-claw deformity.
Evaluation
The assessment possesses:
- Traditional radiographs of the hand (anteroposterior, lateral, and diagonal). In the extensive prevalence of circumstances, this will be sufficient to ensure the diagnosis and form a treatment protocol. Certain points of view, among which are the Brewerton (metacarpal heads), Roberts, and Betts (thumb) hypotheses, might provide confirmation of only relatively small losses.
- CT is occasionally required for the base of metacarpal fractures to inspect for any intra-articular displacement and decide if there is a requirement for operation
Outcome Measures
- Strength of the grip: counted with a dynamometer
- Range of movement
- Patient-Specific Functional Scale
- DASH
- Michigan Hand Outcome Questionnaire (MHO): In this questionnaire, they set six standards for individuals with a hand disorder: general hand performance, activities of daily living (ADL), pain, work arrangement, aesthetics, and patient satisfaction with hand performance.
Treatment of Metacarpal Fracture
Treatment for metacarpal fractures depends on various factors, such as the location and severity of the fracture, as well as the individual patient’s age, overall health, and lifestyle. In some cases, non-surgical treatments such as splinting or casting may be sufficient, while in others, surgery may be necessary to realign and stabilize the fractured bone with wires, pins, plates, or screws.
Medical Treatment of Metacarpal Fracture
The purpose of treatment is the rehabilitation of anatomy and its role.
- Antibiotics and tetanus prevention are options for open-type fractures as per standardized approaches.
- The modality of management will range relying on skin integrity (open against closed fracture), the number of fingers or metacarpals fractured, the strength of the specific, degree of comminution, displacement, or rotational malalignment
- Overall, rising degrees of displacement, comminution, and rotational malalignment are essential elements in evaluating the fracture patterns’ possibility for stability and reduction keeping with non-surgical treatment.
- The GP or Specialist later to estimating the fracture will achieve delicate examinations and imaging to work out if the operation is required.
- If the operation is not required a physiotherapist will make a condition-specific splint, which will sustain the recovery fracture.
Physical Therapy Treatment
Maximum power and range of movement are the main purposes of rehabilitation.
Under the physical therapist’s instructions
- Exercises of the hand with less resistance, for example, their bands or compression of the balls can assist if there is scarring or extensor lag develops.
- Soft tissue healing can be more difficult than a bony one.
- Rest and raising are vital, and so is the quality of splinting – inadequate splinting can result in stiffness, bed sores, or sometimes compartment syndrome also
Physical therapists utilized a variety of methods to recover movement in the hand, wrist, and digits, possessing:
- Swelling control with massage and compression garments
- Soft tissue massage to assist with muscle tension and pain
- Supplying patients with a home exercise protocol of certain movements and strengthening exercises.
More detailed Advice
These are the measures to be observed in a stable fracture:
One or other of the below-stabilizing approaches can be employed:-
- Buddy strapping the injured fingers to another digit is utilized as a non-surgical technique. This is operated with or without the application of differing degrees of splint. The ‘buddy’ decreases the chance of rotational deformity.
- The fracture has to be splinted at 20 degrees of wrist extension, between sixty and seventy degrees of MCP joint flexion, and extension from the IP joint.
- Earlier movement is typically believed appropriate when there are stable fractures or rigid fractures.
- Typically, active range of motion (AROM) movements without resistance can start two to three weeks later to surgical management in not involved or bordering or neighboring joints.
- Active Motion: In case when the fracture is internally fixed, the active range of motion can begin earlier. The vast majority of fractures are treated by immobilization, yet after three weeks of therapy, active mobility is possible beginning with the joints that were not cracked during the previous immobilization. This stage commonly lasts three to six weeks.
- Distinct tendon gliding must be contained in the active motion.
- Tendon gliding is necessary to avoid adhesions, improved blood circulation around the fracture area, and reduced edema and compression at the fracture area.
Exercises For Tendon Gliding
- Claw posture to acquire extensor digitorum communis tendon glide on the bone of metacarpal
- Intrinsic plus posture to acquire central slip. Lateral bands glide on proximal phalanx 1
- Flexor Digitorum Profundus (FDP) stopping exercises to glide the FDP tendon over the phalanx
- Hook fist posture to promote particular FDP tendon glide
- Flexor Digitorum Superficialis (Sublimis) stopping exercise to glide FDS tendon over the center phalanx
- Sublimis fist posture to promote particular FDS tendon glide
Passive Motion
- Passive movement can be started after adequate clinical recovery at about five to six weeks of therapy.
- The timing of initiation of joint mobilization relies on the structures affected by the trauma. If the structures resisting the force are not involved in the trauma, joint mobilization can begin at the same period as an active movement. Compression on the fracture can consequence in contracture, angulation, or rotational mal-alignment of the bone.
- Traditional passive range of motion purpose to help in articular cartilage recovery and decrease swelling, and stiffness.
Resistive Motion:
- Most metacarpal fractures that are treated with immobilization can be achieved four weeks after the trauma with light resistance. The active movement must only be restarted if recovery has not been created.
- Resistive exercise must even be postponed when a fracture is set by pinning until these pins are terminated, to confirm the strength of the fracture. Light resistive exercise benefits scar remodeling and enhanced movement. There are various kinds of resistive exercises for example the load-well exercises. This type of exercise strengthens the finger flexors (FDP and FDS muscles).
- Functional activities and work simulation must be contained in the resistive exercises as soon as conceivable.
Conclusion
Main matters on metacarpal fractures:
- Standard hand trauma
- Need detailed examination consisting of the history taking, assessment, and radiological investigations
- The primary distinction between them is whether they are open or closed, intra-articular or extra-articular in status, and dependent upon where on the bone itself (head, neck, shaft, base).
- May have conservative or surgical management
- Can have prolonged-term sequelae needing additional management
- Rehabilitation objectives are to produce maximum power and range of movement. The importance of rest, elevation, and splint quality cannot be overstated; inadequate splinting can lead to stiffness, bedsores, or even compartment syndrome.
- Physiotherapy is a crucial component in the restoration of adequate hand performance
FAQ
After a metacarpal fracture of the hand, most of the recovery happens between three to four weeks. It’s expected to have aches and discomfort above this. This usually happens when you try activities you last performed a while ago. It’s also typical for the site to be more susceptible for many months after the trauma.
If your fracture is minor and your bones have not shifted significantly from their natural positions (if it is undisplaced), a splint or cast may be all that is needed. Several individuals who participate in a metacarpal fracture require immobilization for three to six weeks. You will require follow-up X-rays to construct certain your bones are healing accurately.
Under regional anesthesia, it is possible to manage a metacarpal fracture or dislocation without surgery by realigning the fractured bones along with tracking digit movement. The broken hand is covered with forearm-based splints or a cast to immobilize the bone to encourage natural recovery.
The Bennett fracture is the most typical fracture affecting the base of the thumb. This fracture is an intraarticular rupture that separates the left first metacarpal from the base of the first metacarpal with respect to the palmar side.
Metacarpal fractures commonly happen secondary to a direct hit or fall directly onto the extended hand. These fractures generally happen during athletic activities, especially in contact sports. Almost one-fourth of issues happen during athletic events.
Their hand will be very hurting, maximally so over the typical metacarpal bone that is fractured. There will represent swelling, usually a significant portion, as well as injury straight over the injury. They may have problems moving their fingers because of the quantity of pain from the fracture.