Lumbar Spine Fracture
Table of Contents
Introduction
A lumbar spine fracture refers to a fracture or break in one or more of the vertebrae in the lower back, specifically in the lumbar region of the spine. The lumbar spine consists of five vertebrae, labeled L1 to L5, which are located between the thoracic spine (mid-back) and the sacrum (pelvic region).
In the Denis system, it was acknowledged that trauma concentrated on the middle column was adequate to result in instability in the spine. The instability was also classified into three classes:
- First degree: regarded mechanical
- Second degree: neurological
- Third degree: combined mechanical or neurological
This system is even presently the preferred approach. The primary frustration with the Denis approach is that the inclusion of the middle column presented a “virtual landmark” that isn’t genuinely relevant for choosing an injury class due to it is not an anatomic entity. A recently developed system by Aebi incorporates the two-column approach, combined with the approach of injury, and instability which can cause neurological complications. This method function with grades of severity, rising from type A to type B and type C. Each type has another further division of grades 1 to 3, also going in increasing manner of severity. In this path, we have nine fundamental injury types which can be again also determined into 27 subgroups of spinal fracture. Unmistakably, the type of fractures is complex and continued.
Clinical Anatomy
Fractures of the lumbar spine, as the term indicates, are consistently situated in the lumbar spine. The lumbar spine is the portion of the spine situated in the most distal at the back and is a typical distressing place in physical therapy. It is located in between the thoracic and the sacral region of the spine and is represented by the term lordosis.
The lumbar spine possesses five vertebrae that are simultaneously strong and mainly flexible to provide the capability to move the body in various planes for example flexion-extension, rotation, and lateral flexion.
A lumbar vertebra possesses of;
- a considerable anterior body that takes most of the load that is put on the spine
- huge posterior vertebral arches which protect the neural structures (spinal cord) lying inside the vertebral foramen (space between the body and the arches)
- various kinds of procedures, on which various muscles and ligaments connect
- the pedicle and facet joints, which are other load-bearing structures
In between the vertebrae, there are intervertebral discs, which keep the load-bearing task of the vertebral bodies and serve as shock absorbers. Another role of these discs is that they join the vertebral bodies to each other.
Epidemiology
“Osteoporosis gave rise to more than two million fractures in 2005, including 547,000 vertebral fractures. Approximately, one-third, and one-third, respectively, of osteoporotic spinal injuries have thoracolumbar, lumbar, or thoracic origins. In addition, 75% of scoliosis-afflicted females older than 65 years also had at least one osteoporotic wedge fracture. The American Academy of Orthopaedic Surgeons’ online page lists fractures in an accessible way and according to the condition’s type:
The flexion type comprises compression fractures and axial burst-type fractures. The extension type comprises flexion or distraction (commonly known as a chance fracture). The rotation type includes a transverse process and fracture-dislocation.
On current days, fractures are separated into type A, B, or C fractures. These are truly identical to the ones explained above. Although adequately effective investigations regarding the epidemiology of fractures of the lumbar spine are lacking, many investigations recognize osteoporosis as the main reason for several fractures of the lumbar, especially in after-menopausal females.
Cooper et al. discovered an age-adjusted incidence rate of 117 per 100,000 in females that was nearly 2x that in males(73 per 100,000). Of all fractures, fourteen percent followed extreme trauma, 83 percent followed moderate or no trauma, and three percent were pathologic. Incidence rates for fractures next to moderate trauma were greater in females than in males. In contrast, males were more inclined to experience fractures close to severe trauma, and their incidence reduced with age. Keep in mind that the localization (cervical, thoracic, or lumbar) and type of fracture were not determined by this research.
Type A fractures- compression (flexion pattern):
- The defeat of the volar column to resist reduction.
- Burst fractures (Type A3) are the most regular and painful type of Type A fractures. They can be identified by an increase in interpedicular length and a decrease in vertebral body height.
- There are further A3.1 Incomplete, A3.2 Complete, and A3.3 Burst split fractures. The entire burst fracture concerns both endplates, the superior one as well as the inferior one.
- Compression fractures are a common reason for an axial load on the volar portion of the vertebrae. Because of this vertical force, this precise portion of the vertebrae will lose height and will become wedge-formed.
- Axial burst fractures are likewise caused by an axial load on the vertebrae, but unlike compression fractures, the vertebra is crushed in all directions so it expands out in every direction.
- This indicates that mainly because there is a danger of the bone borders damaging the spinal cord, this form of fracture is far more difficult than a compression fracture. These types of fractures are commonly found in road traffic accidents or fall from a distance.
- Burst fractures can consequence in a few retropulsions of the vertebra into the vertebral canal.
Type B fractures- distraction (extension pattern):
- Failure from the dorsal column to resist distraction
- B1-lesions are lesions in which the posterior ligament is disrupted but without the involvement of appropriate bony elements. The B2-lesions are fundamentally bony seat belt injuries also known as Chance fractures. B3-lesions are lesions that are to be located in the volar column, producing very distinct fractures.
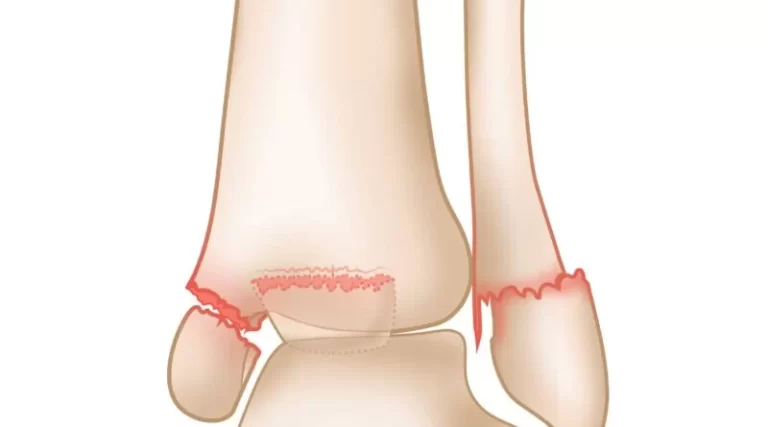
- A Chance fracture consequence from a flexion-distraction movement a sudden halt in traffic where the seat belt’s force forces the vertebrae apart. For this cause, chance fractures are also known as ‘seatbelt fractures’ and are usually connected with intra-abdominal impairments. Chance fractures affect all three spinal columns. The vertebral body suffers a flexion injury while the dorsal elements suffer a distraction-kind injury.
- If this kind of injury stays neglected, it can consequence in progressive kyphosis with pain and deformity.
Type C- rotation:
- Consequences in disrupted dorsal tension banding technique and a disruption of the volar column with a rotational dislocation.
- Transverse process (TP) fractures are not common and result from extreme sideways flexion. These do not commonly involve stability.
- The fracture-dislocation is a fracture in which bone and its concurrent soft tissue will move off a side-by-side vertebra. This kind of fracture is a not-stable and can outcome in painful spinal cord reduction.
- A C1 lesion is created when an anterior lesion and rotational damage come together. The C3 lesion is distinguished by multilayer and shear injuries with a range of appearances and some relatively rare forms, in contrast to the C2 lesion, which includes rotational damage and the particular lesion.
Basic features of the three damage kinds;
- Type A, compression damage of the volar column.
- Type B, two-column trauma with either volar or dorsal transverse disruption.
- Type C, two-column trauma with rotation.
Type A B C (according to M. Aebi, V. Arlet, J.K. Webb, in AO-Manual of Spine Surgery, Vol. I, 2008. Thieme Publisher, Stuttgart)
The estimation of a complete collective of trauma learned us that there is a dominance of trauma at the thoracolumbar junction with the most regular fractures at L1, second frequent at T12, third regular at L2, and fourth at regular at L3. trauma of the T10 and L4 vertebrae are of the identical commonness along with injuries of T5, 6, 7, and 8.
While the listed examples further imply trauma for a spinal fracture, osteoporosis and diseases for example osteogenesis imperfecta are generally implicated in vertebral fractures as well.
Causes of Lumbar Spine Fracture
Fractures of the thoracic spine can cause by high-impact injury, for example as a:
- A car collision or road traffic accident
- Fall from a significant distance
- Sports Injury
- Violent actions, for example, a gunshot wound
- Several times, these patients have more severe damages that need quick treatment. The spinal cord or nerves may also be damaged, relying on the severity of the fracture.
Spinal fractures may even be reason by bone deficiency. For example, individuals with osteoporosis, tumors, or other underlying pathology that weaken the bone can fracture a vertebra even during low-force events — for example reaching or twisting, or falling from a fixed height. These fractures may develop neglected over a period of time, with no symptoms or distress until a bone fracture.
Symptoms of Lumbar Spine Fracture
Lumbar spine fractures at the thoracolumbar junction are fairly not uncommon. Per the description, in compression kinds fractures the volar column is impacted, whereas in burst fractures, the anterior and central columns,s and sometimes the dorsal column, are involved. Compression-type fractures are predominately caused by indirect hyperflexion and flexing forces whereas burst-kind fractures cause by axial loading.
Greater than sixty percent of vertebral fractures can not reason recognizable symptoms and can be not diagnosed with radiographs. Patients may have neurologic complications, can have low back pain, movement can be affected, or a mix of all of them. When the spinal cord is even possessed, abnormal feelings like numbness, tingling, weakness, or bowel or bladder impairment may happen.
Upon examination of the spine, the patient examination has a kyphotic posture that can not be associated. The kyphosis is reasoned by the wedge form of the fractured vertebra; the fracture essentially turns the lateral conformation of the vertebra from a square to a triangle.
A valuable device for this type of thoracolumbar trauma is ‘the Thoraco-Lumbar Injury Classification and Severity(TLICS) type method’. Current studies have increased concerns about the reliability of both the Denis and the AO systems, which have been earlier mentioned. Because each system includes numerous subtypes, both systems demonstrate a reasonable level of inter- and intra-observer dependability. This indicates that the risen complicatedness of the type system usually leads to less reliability in the clinical setting.
The Spine Trauma Study Group (STSG) established the Thoraco-Lumbar Injury Classification and Severity (TLICS) scale, which utilizes three “primary axes”:
- Damage morphology
- Probity of the posterior ligamentous complex (PLC)
- Neurological situation.
The three primary axes are further broken down into a small number of readily identifiable categories, each of which additionally represents a distinct injury in order of least to highest efficiency.
The interpretation of the TLICS severity score is easy. Lower point values are assigned to the less painful or less critical injuries and greater point values are given to more painful or more critical injuries. Severity is typically used to estimate the degree of injury to the ligamentous and bony parts of the spine. The TLICS procedure has been demonstrated useful in conducting operative treatment. The scores of the three primary axes are added to yield a total severity score. This score can commonly indicate the necessity for operative intervention. Commonly speaking, a total score greater than five needs operative intervention whereas a score more than 3 can be managed non-surgically.
The reliability and facts have been examined broadly. Since the intro of the type system, it experienced a sequence of modifications. The most current version of the system has been demonstrated to be both accurate and reliable by various different investigations, Rampersaud et al. The TLISS establishes a consensus-based strategy for treating thoracolumbar injuries, based on a multi-center reliability study that concluded in 2006. Patel et al. (2007) also established the validity of the system in a prospective study. The primary purpose of this investigation was to evaluate the time-dependent changes in inter-observer reliability. They discovered that there was considerable progress in the second inspection, which means that the type system can be taught efficiently. There are even more studies analyzing the reliability and the fact and all show favorable outcomes. Thus we can complete this system can be incorporated into daily practice.
Differential Diagnosis
- Coccyx pain
- Lumbar Facet Arthropathy
- Mechanical Low Back Pain ( Non-Certain Low Back Pain)
- Lumbar Degenerative Disc Disease – a procedure in which the intervertebral discs of the lumbar region lose height and hydration.
- Lumbar Spondylolysis – a unilateral- or bilateral bony defect in the pars interarticularis or isthmus of the vertebra
- Golden measure: a combination of SPECT and (CT).
- MRI is a useful tool for diagnosing as well, as T1-weighted MR pictures have been demonstrated helpful in the earlier diagnosis of spondylolysis. In addition, MRI permits spondylolysis to be interpreted in the absence of ionizing radiation
- Lumbar Spondylolisthesis
- Osteoporosis – a condition described by a reduction in bone density (mass and quality)
Diagnostic Procedures
Plain radiography has been viewed as the gold standard for analyzing spine fractures, although spiral computed tomography (SCT) is now utilized more repeatedly. Computed Tomography is more susceptible than plain radiographs for assessing the Thoracolumbar spine next to the trauma. In extra, Computed Tomography can be achieved quickly. According to one investigation by Brown et al. SCT of the spine recognized more than ninety-nine percent of almost all fractures of the cervical, thoracic, and lumbar spine. Those skipped by the SCT needed minimal or no treatment. SCT is a susceptible diagnostic examination for the identification of spinal fractures.
A more current investigation by Ang concluded that 3-T Magnetic Resonance Imaging (MRI) with thin-slice 3D T1 VIBE is 100 percent correct in analyzing complete pars fractures and has excellent diagnostic ability in the detection and description of incomplete pars stress fractures compared to CT. MRI has the counted advantage of detecting bone marrow edema and does not employ ionizing radiation. One disadvantage is that MRI may be substantially more expensive than CT for some associations.
Outcome standards
To evaluate if the treatment is functioning or has been performed one can take an x-ray and assess the bone mineral density. Subjectively, a therapist sees advance with different tests that specify the range of motion and power. The measures can also be taken by other tests.
Clinical examination
While height loss is common with aging due to the intervertebral discs’ progressive compression as we get older, it can also be a sign of a spine fracture. Without radiographic imaging, it is difficult to determine whether a fracture exists. Therefore, radiographic imaging should be used to confirm a fracture with absolute certainty.
Due to the unpredictability of the quantity of damage, when a recent condition of a lumbar fracture occurs, the patient needs immediate medical attention. A physician must do a complete body assessment to make certain the fracture did not result in any other impairment.
It is of grave importance for the physician to do a neurological examination as well as imaging examinations. The neurological tests assess if the patient has experienced damage to the spinal cord or nerves that arise in the lumbar area. the examinations consist of moving, feeling, and feeling the extremity in different positions and testing the reflexes of the patient.
The imaging tests possess of X-rays, CT scans, and MRIs relying on the extent of the trauma that is suffered.
Radiologists must take a forceful role in assisting to analyze spinal fractures. The failure to diagnose vertebral fractures is a worldwide situation because of in part to the absence of fracture recognition by radiologists and the use of ambiguous terminology in radiology reports.
Physical therapists can even be more employed via a detailed assessment that contains:
- A thorough history
- A neurological assessment
- Palpation, mostly midline along the vertebrae
- Range of motion, STR, joint mobility, and muscle length examinations
- Cautious differential diagnosis
Treatment of Lumbar Spine Fracture
Medical Management (current best evidence)
Burst-type fractures patient is a kind of traumatic spinal trauma in which a vertebra fracture caused by a high-impact vertical axial load of the lumbar and thoracic spines must acquire individualized patient mensuration prior to the time of treatment can be determined. Considering fracture stability, the extent of canal compromise, and patient assessment become crucial when deciding whether to do operations or not. In neurologically unbroken patients with specified fractures, nonsurgical treatment can be successful in the practical rehabilitation of the patient.
Operative
When neurological dysfunction is current, operative approaches are commonly needed to repair or clear the area of damage. There are numerous additional strategies that depend on the level of compromise, the extent of the spinal fracture, and the patient’s prior health.
An approach known as ‘decompression’ is an example of one of these approaches. In this approach, a little portion of bone or disc material that compresses the nerve root is operatively released to provide the root more space.
Anterior or Posterior Approach: A surgeon might frequently employ an anterior or posterior approach to the patient’s spine in order to stabilize it, in accordance with the degree of the compromise or level of damage. Rods, screws, and other mechanical instruments are inserted via the remaining structures to fuse the involved vertebra(e). The anterior approach dominates upper lumbar (L1, L2) fractures because of involvement with the crura of the diaphragm while lower lumbar fractures (L5) are stabilized via a posterior approach method.
Kyphoplasty: A mini-invasive percutaneous approach that lessens fracture of vertebral pain via the heat released during bone cement coagulation. The cement likewise solidifies to additional stabilize the area of damage. During the process, a cannula is introduced into the vertebral body observed by a bone expander to recover some vertebral height. In terms of favorable outcomes, kyphoplasty has been reported to be equivalent to vertebroplasty, but with greater healing of vertebral height.
An investigation by Wardlaw et al. suggests that Balloon Kyphoplasty (a minimally invasive method for the management of hurting vertebral fractures) is an effective and secure approach for patients with acute vertebral fractures.
Vertebroplasty: Vertebroplasty, an effective way of treating vertebral compression fractures, involves injecting bone cement composed of polymethylmethacrylate (PMMA) into the damaged vertebral body.
R. Takemasa investigated this method’s effect on osteoporotic vertebral compression fractures and found no discernible clinically significant benefits over a sham surgery performed.
Non-operative
Patients not needing an operation to acquire treatments that main pain ease with bracing and rehabilitation therapy. Those with compression-kind and burst-kind fractures affecting the volar and central column have been represented as the most suitable candidates for non-surgical management.
Compression Fractures
In accordance with an investigation by Stadhouder, brace treatment along with extra physiotherapy is an effective alternative for people who have compression fractures of the thoracic and lumbar vertebrae.
Burst Fractures
Surgical treatment of patients with a regular thoracolumbar burst fracture and normal conclusions on a neurological examination delivers no important long-term advantage corresponding with nonsurgical treatment.
A coming investigation by Shen et al. corresponding to the surgical and non-surgical treatment of thoracolumbar burst fractures without neurological deficit accepts the initial pain relief and partial kyphosis correction delivered by surgical short-segment posterior fixation. Still, the functional output at two years is identical to that of non-surgical treatment.
Orthoses
A thoracic-lumbar-sacral orthosis (TLSO) is the recent brace alternative for this kind of condition. Regardless, patients will also like to move into mobility as their pain and recovery process advances. Therefore permitting them to move into load-bearing exercises to avoid future osteoporosis and extension exercises.
Non-surgical alternatives are increasingly becoming the choice procedure of fracture management as bracing and therapy approaches are demonstrated to be as clinically effective, yet much more cost-efficient than operative alternatives.
Orthoses have shown remarkable improvements in muscle power, posture, and height of the body. The brace makes complete confidence that muscles along the vertebrae get less fatigued and decreased muscle spasms. In fractures of the lumbar, an orthosis is open but can only determine sagittal plane motion in the upper lumbar spine (L1-3). Motion between the distal segments has been proven to be improved while wearing an orthosis brace (L4-S1).
Pharmaceutical
Medicines options from Tylenol and NSAIDs to opioids can be carried to modulate pain of the lumbar spine fracture. Spinal nerve obstructions at the L2 site have also been found to be effective in front of recent low back pain from fractures.
Physical Therapy Treatment
The goal of physiotherapy the chances of fractures in future management in patients with fractures of the lumbar spine is to decrease pain, and improve mobility, and control. While mobility is necessary, back extensor and abdominal (core) strength have been demonstrated as practical therapeutic interventions for those with lumbar problems correlated with osteoporosis.
In certain, the multifidus, quadratus lumborum, and transverse abdominals assist keep the spine. So much so that improving strength not just relieves pain and symptoms from those patients with fractures but even can act as a preventative to reduce the chances of fractures in the future. Physiotherapy protocols that encourage exercise targeting dysfunction in intrinsic back power have been shown to enhance the function and quality of life in those with osteoporotic fractures of the vertebra. Several recommended exercises can be seen below.
Take special attention to hip bridging, reverse curl-ups, especially transverse abdominal control.
- Concentrate on strengthening transverse abdominals.
- Stabilization is improved through multifidus, transverse abdominal, and oblique contraction. This exercise functions both the core and back muscles, hitting the TA, multifidus, and quadratus lumborum.
Thoracolumbar fracture therapy proof closely parallels that of the lumbar spine and other exercises can be found here Thoracic_Spine_Fracture.
Considering the availability of essential nutrients, the stimulus to the osteoblasts outcome in a total gain in bone mass. Exercise is a structure of repetitive loading that encourages osteoblastic activity, thereby assisting in keeping a positive balance between bone formation and bone resorption.
Even a very moderate amount of exercise that is suggested for overall wellness (a minimum of thirty minutes on most days) is valuable in controlling osteoporosis and strengthening bone density.
General, physiotherapy has been demonstrated to have no clinically important difference in outcomes when correspond to operation for proper spinal fracture patients. Not only does physiotherapy help reduce pain and disability as well as operation, but the general price to the patient is significantly lowered.
Complications of Lumbar Spine Fracture
Complications co-related to fractures of the thoracic and lumbar spine contain :
- Blood clots in the pelvis and legs—these may form during prolonged times of bed rest or immobility
- Pulmonary embolism—a blood clot that dislodged free and moves to the lungs
- Pneumonia
- Pressure sores or\ bed sores
There are also detailed complications associated with spinal operations. These possess:
- Bleeding
- Infection
- Spinal fluid leaks
- Instrument flop
- Nonunion
- Wound complications
Your physician will chat with you regarding these threats and take precise measures to prevent possible problems. These measures may contain:
- Early treatment
- Mechanical techniques (for example lower leg compression stockings) and medicines to protect in front of blood clots
- Appropriate surgical technique
- Postoperative protocol
FAQs
The prevalence of fractures recovers with pain medicine, reduction in movement, medicines to stabilize bone density, and a suitable back brace to prevent unnecessary movement during the recovery process. Many individuals return to their regular activities. Some can require additional treatment, such as an operation.
Small fractures of the spine can be recovered with immobilized and painkillers, however, more hurting fractures may require operator intervention to realign the bones. If remain not treated, spinal fractures can result in permanent spinal cord damage, nerve impairment, and paralysis.
Unfortunately, there’s no other method to reverse injury to the spinal cord. But investigators are constantly functioning on new treatments, including prostheses and medicines, that might facilitate nerve cell regeneration or enhance the function of the nerves that stay after spinal cord damage.
Over the period, multiple fractures can result in the central part of the vertebrae (the bones that built up the spine) collapsing, resulting in a wonderful deal of pain and even changing the form of your spine. Chronic discomfort brought on by spinal compression fractures might gradually reduce mobility in older persons.
Recent (short-term) back pain stays for some days to a few weeks. It commonly resolves with medical treatment, physical therapy treatment, and exercise for a few days with self-care. Regular back pain is pain that persists for twelve weeks or longer, even after an early injury or underlying reason for back pain has been requiring proper medical treatment.
The L4-L5 movement component may result in referred pain from the joints or muscles or radicular symptoms that cross via nerves. Referred pain from L4-L5 commonly remains within the lower back and is commonly regarded as a dull ache. The back can also feel stiff.
Try drinking a sip of cherry juice on a day-to-day basis and see if it has favorable results in relieving your back pain. You can also try infused-herbal glasses, for example, ginger-green tea, which includes the pain-relieving advantages of both green tea and ginger.