Fibula Fracture
Table of Contents
Introduction
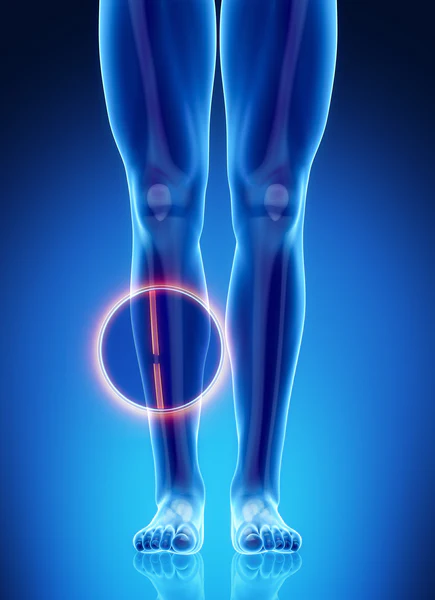
A fibula fracture is a type of bone fracture that affects the fibula bone, which is located in the lower leg. The fibula bone runs parallel to the tibia bone, and it plays an important role in stabilizing the ankle joint.
Fibular fractures can occur in isolation or as part of a more complex injury involving the ankle joint, such as an ankle sprain or dislocation. Common causes of fibular fractures include trauma from a fall, twisting injury, or direct blow to the lower leg.
Symptoms of a fibular fracture include pain, swelling, bruising, and difficulty bearing weight on the affected leg. Treatment typically involves immobilization of the leg with a cast or brace, and in some cases, surgical intervention may be necessary. Rehabilitation exercises are often prescribed to help restore strength and range of motion to the affected leg. With proper treatment and rehabilitation, most people with fibular fractures can expect to make a full recovery.
The Fractures of the tibia and fibula are most common in athletes, or non-athletes who suddenly increase their activity status. Various characteristics seem to contribute to the development of these fractures involving changes in athletic training, reduced bone density, and pathology.
Fractures of the fibula occasionally happen with severe ankle sprains. The fracture may happen anywhere along the fibula. The fibula only contributes 17 percent of the body weight so these fractures are not as intense as weight-bearing bone fractures.
Clinical Anatomy
The fibula is a non-weight-bearing bone that is situated slightly below the lateral tibial plateau and extends distally to create the lateral malleolus, which is part of the fibula distal to the superior articular surface of the talus. The lateral malleolus delivers essential stability in front of excessive eversion of the ankle and foot. Proximally, the fibular head is the region of attachment of the lateral collateral ligament of the knee and biceps femoris tendon.
Slightly below the fibular head, the common fibular nerve surrounds near the fibular neck priorly dividing the proximal fibula into deep and superficial branches. Upper and middle lateral boundary of the fibula, The peroneal longus, & peroneal brevis muscles originate and function as protection of soft tissue to the fibula from a direct hit. The fibrous attachment between the tibia and fibula, the tibiofibular syndesmosis, avoids displacement of the lateral malleolus.
The lower part of the syndesmosis has thickened fibers to form the distal tibiofibular ligament. The stability of this ligament permits the ankle to stay stable with external rotation and during the forceful cutting movements needed in multiple sports. Disturbance of the syndesmosis (syndesmotic or high ankle sprain) contributes to the instability of the tibiotalar joint.
Mechanism of Injury
The mechanism of injury for tibia-fibula fractures can be divided into 2 types:
- low-impact injuries for example ground level falls and sports trauma
- high-imact injuries for example road traffic accidents, pedestrians hit by motor vehicles, and gunstab wounds.
A person can inform a H/O of direct (motor cycle hit or axial loading) or indirect (twisting) trauma and may complain of pain, swelling, and difficulty transfer with a tibia fracture.
Cause
Fibular fractures can occur due to a variety of reasons, including traumatic injuries such as falls, sports injuries, or car accidents. They can also occur as a result of repetitive stress on the bone, such as in runners or dancers.
Distal fibular fractures describe the prevalence of ankle fractures. Fibular fractures in younger adults are frequently caused by trauma, still when corresponding to fibular fractures of the elderly that normally happen as a consequence of low-energy injuries, the severity of tissue damage is comparable. Isolated fibular fractures carry the prevalence of fractures of the ankle in more aged women, happening in about one to two of every thousand white females per year. Fibular fractures may also happen as the consequence of repetitive loading and in this case, they are defined as stress fractures.
Risk factors
Bone mass is the main threat factor for fractures of the fibular or tibial shaft in older adults. Factors that decrease bone mass had a greater impact than general health status or other danger factors for falling. Cigarette smoking is another significant threat factor for fibular fractures.
Fibular fractures are more typical in athletes or sports players that involve cutting, especially those associated to contact or collision, for example, in American football, soccer, and rugby. Participants in downhill winter sports have fairly high rates of fibular fractures. These are more specific in snowboarding than skiing and fracture patterns are different for each. In skiers, fractures of the proximal one third of the tibia and the fibula are common, while, snowboarders are more at risk of having isolated fractures of the lower third of the fibula.
Classification
The Danis-Weber type or Weber type is a convenient form for categorizing fractures of lateral ankle fractures and is dependent on X-ray standards. It carries into consideration the position of the lower fibular fracture in association with the syndesmosis of the ankle joint. There are three classifications depending on the site and kind of fracture.
Type A represents a fracture of the lateral malleolus lower to the syndesmosis (the association between the lower ends of the tibia and fibula). Typical characteristics:
- Lower the level of the tibial plafond (syndesmosis)
- Tibiofibular syndesmosis intact
- Deltoid ligament intact
- Occasional oblique or vertical medial malleolus fracture
Type B is defined as a fracture at the line of the tibial plafond (syndesmosis). Fracture of the fibula at the line of the syndesmosis. Irregular stability. Typical characteristics:
- At the line of the ankle joint, extending proximally in an oblique manner up the fibula
- A tibiofibular syndesmosis is not damaged or only partially torn, but no widening of the lower tibiofibular articulation
- The medial malleolus can be fractured or the deltoid ligament can be ripped
Type C – defines a fracture proximal to the line of the tibial plafond and is oftentimes corresponding to syndesmotic damage. Unstable requiring ORIF.Typical characteristics:
- Above the level of the ankle joint
- Tibiofibular syndesmosis damaged with the widening of the lower tibiofibular articulation
- Medial malleolus fracture or deltoid ligament damage can exist.
Symptom
A fractured fibula normally presents with the following signs and symptoms:
- the presence of pain, swelling, and tenderness;
- difficulty to bear weight on the involved leg;
- bleeding and bruising in the leg;
- visible deformity;
- abnormal feeling of numbness sensation and feeling of coldness in the foot
- tenderness to palpate.
Diagnostic Procedures
Early diagnosis and treatment are important for a successful recovery and to prevent long-term complications such as chronic pain, instability, and arthritis.
- Physical assessment: A detailed examination is performed involving assessment for any apparent deformities.
- X-Rays are used to identify the fracture and possible bone displacement.
- MRI Scans provide a more detailed scan and can generate detailed pictures of the interior bones and soft tissues.
- CT Scans, Bone scans, and other related examinations method help for more precise diagnosis and to check the severity of fracture of the fibula.
Differential Diagnosis
- Acute Compartment Syndrome
- Tibia Fracture
- Ankle Fracture
- Ankle Injury, Soft Tissue
- Child Abuse
- Knee Fracture
- Pediatric Limp
- Peripheral Vascular Injuries
- Soft Tissue Knee Injury
Treatment
The severity of a fibular fracture can vary widely depending on the location and extent of the fracture. Some fibular fractures may only require conservative treatment such as rest, immobilization, and physical therapy, while others may require surgery to realign and stabilize the bone.
Distal fibular fractures will mainly require open reduction internal fixation, regardless of stable minimally displaced fractures, conservative treatment can be followed with excellent results. If the fracture is open, additional management is warranted to minimize the threat of contamination and infection
Open fracture (compound fracture)
simple and compound fractures of the fibula are depending on whether the skin has been torn or the bone is exposed to the environment. In an open fracture, either the bone is exposed to the environment or deep damage exposes the bone through the skin. Open fractures are usually the consequence of a high-impact trauma or direct hit, for example, a fall or motorcycle crash. This type of fracture can likewise happen indirectly for example with a high-impact twisting kind of trauma. The force needed to cause these kinds of fractures suggests that patients will usually receive further damage. Several damages could be potentially life-threatening.
According to the American Academy of Orthopedic Surgeons, there is a forty to seventy percent rate of corresponding trauma elsewhere within the body. Physicians will treat open fibula fractures directly and examine for any other damages. Antibiotics will be assisted to avoid infection. A tetanus shot will also be provided if required. The wound will be cleaned simply, examined, stabilized, and then wrapped so that it can recover. An open reduction and internal fixation with plate and screws can be needed to stabilize the fracture. If the bones are not matching, a bone graft can be an option to facilitate healing.
Closed fracture (simple fracture)
In a closed fracture, the bone is cracked, but the skin stays unbroken. The purpose of treating closed fractures is to put the bone back in position, minimize the pain, provide the fracture time to recover, avoid complications, and restore normal function. Treatment starts with the raising of the leg. cryotherapy method is used to decrease pain and reduce swelling. If no surgery is required, crutches are utilized for mobility and a brace, cast, or walking boot is suggested while recovery carries place. Once the region has recovered, people can lengthen and strengthen weakened joints with the assistance of a physical therapist.
There are two main types of operation if a patient needs them:
- Closed reduction involves realigning the bone back to its original position without the necessity to make an incision at the fracture area
- Open reduction and internal fixation realign the fractured bone to its original position using hardware for example plates, screws, and rods
The ankle will be put into a cast or fracture boot until the recovery procedure is finished.
Physical therapy treatment
After having been in a cast or splint for many weeks, most individuals find that their leg is weak and their joints stiffness. A physiotherapist is executed after a personal examination of the patient. It is crucial to consider the following symptom given below:
- Pain and edema
- Range of motion (ROM)
- Muscle strength
- Surgical scar tissue
- Patient ambulation and weight bearing
Physical therapy usually initiates with strengthening and mobility exercises of the ankle. Once the patient is fit sufficiently to put a load on the affected site, walking and stepping exercises are standard. Balance is an essential component of recovering the capacity to walk independently. Wobble board activities are a wonderful way to work on balance.
According to ORIF fibula fracture post-operative protocol, there are 4 phases in the rehabilitation of fibular fracture:
Phase 1- Maximum protection for 0 to 6 week
- Cast or boot for 6 weeks
- Elevate the ankle above the heart
- Non-weight bearing x 6 weeks
- Multi-plane hip strengthening
- Core and upper extremity strengthening
Phase 2- Range of motion and initial strengthening for 6 to 8 week
- Full active and passive pain-free ROM on all planes
- Strong emphasis on restoring full dorsal flexion
- Isometric and early isotonic ankle exercises
- Foot intrinsic muscle strengthening
- Gradual progression to full weight bearing
- Restoration of normal gait mechanics
- Bilateral advancing to unilateral squatting, stepping, and matrix advancement
- Proprioception training
- Non-impact cardiovascular work
Phase 3- Progressive strengthening for 8 to 12 week
- Restoration of the full range of motion in all planes
- Advance ankle and foot intrinsic strengthening
- Pool running progressing to dry land
- Linear moving to lateral and rotational active motions
- Bilateral progressing to unilateral plyometric activity
Phase 4- Advanced strengthening for 12 to 16 weeks
- Advanced impact and functional progressing
- Sport-specific drills on the field or court with a functional brace
- Sport test at 3-4 months depending upon improvement
For long-term maintenance in charge to decrease a fracture threat it is significant to:
- Wear appropriate footwear;
- Follow a diet complete with calcium-rich meals for example milk, yogurt, and cheese to allow build bone strength;
- Do weight-bearing exercises to help strengthen bones.
FAQ
You should do the rest of your affected fibula fractured leg until your doctor allowed you to do exercise, or you can also take the advice of a Physiotherapist before starting any exercise. Typical physiotherapy exercises to anticipate next to a fibula fracture or any other broken ankle bone typically have Walking education. Physical therapists can assist patients to start putting a load on the involved leg and slowly progressing to the total weight. Gait training.
After an injury, it can carry up to 12-16 weeks to make a complete healing. Your physician will use X-rays to see how well your fracture is recovering. They’ll also examine to see when they can remove the screws if you have them.
Treatment. Occasionally, an isolated fibula fracture — a traditional”twisted ankle” — that does not affect the ankle joint can be treated with a brace or conservatively, with no operation needed. An injury to the internal part of the ankle, yet, can need an operation.
You have maintained a fracture to your outside ankle bone (fibula). This carries roughly six to eight weeks to recover, although pain and swelling can persist for three to six months. You can walk on foot as convenience permits although you may find it more comfortable to walk with crutches in the initial phases.
From active people to professional athletes, sleep plays a significant function in wound healing. Whether you’re facing a muscle strain, injured tendon, or bone damage, sleep is essential to getting your body back in the highest condition