Neuropraxia
Neuropraxia is a type of nerve injury characterized by temporary dysfunction or impairment of nerve conduction without any structural damage to the nerve fibers. It is the mildest form of nerve injury and usually resolves gradually with proper treatment.
The mildest type of peripheral nerve damage (PNI) is neurapraxia. Grades I to V make up the five main levels of PNIs. These levels differ from one another based on an increasing degree of nerve injury.
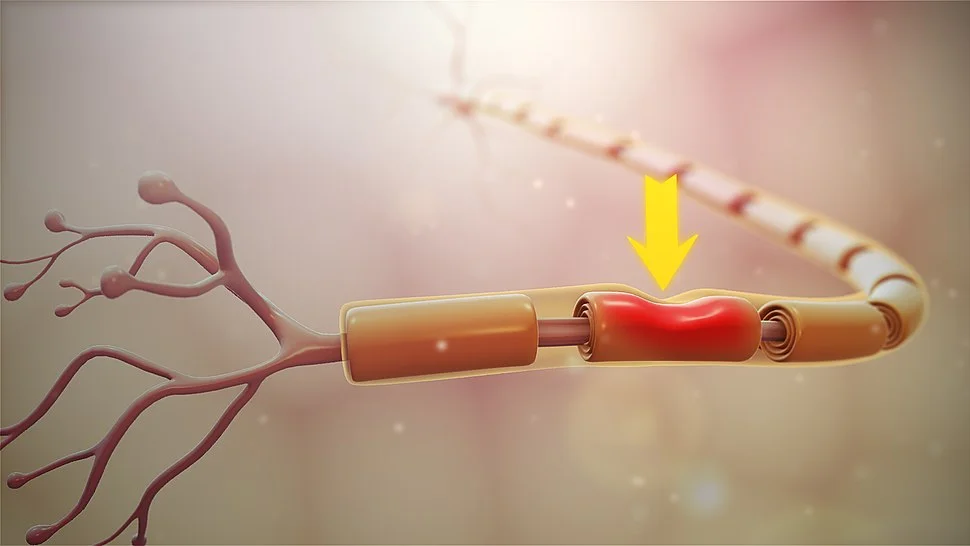
Neurapraxia is the name for PNIs in grade 1. In these situations, neither the actual nerve axon nor any of the connective tissue around it is harmed. The axon is the long portion of the cell that conveys electrical signals.
A block that builds along the nerve and prevents electrical signals from passing is what causes the symptoms of neurapraxia. The injured area cannot communicate with other areas of the nervous system until this block is removed.
The most typical type of nerve damage is called neuropraxia. Although PNIs are not well-reported, the rates are between 13 to 23 cases per 100,000 individuals each year.
Table of Contents
What is Neuropraxia?
The peripheral nerves are hurt when you are suffering from neuropraxia. Your brain and spinal cord send electrical messages (impulses) across these nerves to the rest of your body.
A peripheral nerve injury called neuropraxia affects the nerve conduction in the affected area and results in motor and sensory deficits. A grade 1 peripheral nerve damage called neuropraxia inhibits the affected nerve and stops electrical signals from being transmitted. Until the nerve block is removed and signal transmission resumes, the afflicted spot cannot communicate with the rest of the body. Any injury from accidents, sports, surgical trauma, etc., might result in the condition.
Usually, these minor peripheral injuries heal on their own, but if the pain is severe, treatment, including surgery, may be required. Therefore, one should take the required precautions to avoid such events and wear protective gear such as helmets, knee pads, elbow guards, and other equipment.
Neurapraxia is a transient disorder that causes brief damage to the myelin sheath but leaves the nerve unharmed; as a result, Wallerian degeneration does not take place. The Seddon classification system of peripheral nerve injury requires that, after nerve conduction has been restored, there be a complete and relatively rapid recovery of motor and sensory function; If not, the damage would be categorized as either axonotmesis or neurotmesis. Neurapraxia is the mildest kind of peripheral nerve injury as a result.
Neurapraxia is a disease of the peripheral nervous system that results in impeded nerve conduction and transient loss of motor and sensory function. The normal time frame for recuperation is six to eight weeks. The phrase neuropraxia, which implies “loss or impairment of the ability to execute complex coordinated movements without muscular or sensory impairment,” was coined from the word apraxia.
This syndrome is often brought on by repeated or protracted pressure building on a nerve due to a blunt neural injury brought on by external blows or shock-like injuries to muscle fibres and skeletal nerve fibres. This pressure causes ischemia and neurological damage, and the body’s natural response is oedema that spreads out in all directions from the pressure source. This lesion results in a reduction or loss of function in some neural connections downstream from the lesion, which leads to muscle weakness, and an action potential conduction block over a section of a nerve fiber.
Neurapraxia is a disorder that can and should be treated by a doctor and is particularly common in professional sports, especially American football players.
Anatomy:
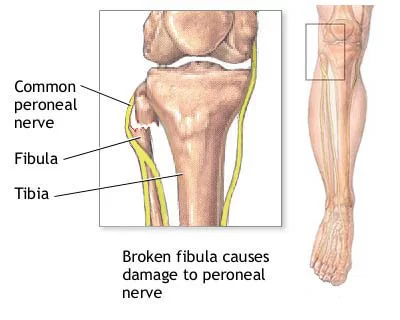
Neurapraxia commonly affects the sciatic and peroneal nerves in the lower body as well as the ulnar, median, and radial nerves in the upper body. Peripheral nerves are myelinated, rather large, spatially complicated cells that are generally more vulnerable to damage and impede their capacity for self-repair, yet this is not the case in neurapraxia. According to microscopic data, the axon is unharmed but the myelin sheath has been damaged. As a result, the myelin damage can be healed and distant nerve fibers do not age prematurely.
What do the peripheral nerves do?
From your brain and spinal cord (central nervous system) to the rest of your body, your peripheral nerves transmit signals. Electrical impulses carry these signals, instructing your muscles to contract and move to assist you use your senses.
Axons are the fibres found inside nerve cells (neurons). The nerve impulses are carried by these fibres. The axons are covered by a protective covering of protein and fat (myelin) that promotes fast impulse conduction.
Causes:
A neural injury that temporarily prevents nerve conduction without transection of the axon is the root cause of neurapraxia. A conduction block is defined as a 40% or 50% drop in action potential amplitude over a short or long distance on the nerve, respectively.
Numerous factors can contribute to neuropraxia. Crushed or compressed nerves are possible. They are unable to transmit electrical impulses when this occurs.
Compression and ischemia, or insufficient blood flow to the tissues, are the main causes of neuropraxia. Neurapraxia can also result from inflammation.
Although the exact mechanism by which nerves are stopped is unknown, neurapraxia is more likely to occur in nerves that run via small bodily passageways.
Injury mechanisms:
Mechanical lesions, ischemia, immunologic attacks, metabolic problems, toxic substances, and radiation exposure are a few of the factors that can cause nerve damage. Compression of the nerve, which results in reduced blood supply to the nerve and distortion of the nerve fibers, is the most frequent mechanism of injury.
Organizing pathology:
A common pattern of nerve injury can be seen in the order of pathology over the first 24 hours following injury. Focal swelling close to the injury site is the initial physical sign of the damage. Pressure applied to the nerve causes fragmentation of microtubules and neurofilaments in the cellular dimension. Axons swell at some spots and contract at others, giving the appearance of beads
There are many causes of neuropraxia, including:
- Complications following surgery
- Inadequate body supports’ cushioning.
- Poor placement of the body during operations.
- Complications from anaesthesia result in chemical nerve injury or a cutoff of blood flow due to artery constriction.
- Hip replacement procedures may also result in ACL (anterior cruciate ligament reconstruction)-related complications. Neurapraxia is more likely to occur after some procedures than others. For instance, all anterior cruciate ligament (ACL) repair surgeries carry a risk of neurapraxia of 75%, yet hip replacement surgeries carry a risk of less than 1%
Neuropraxia due to trauma:
- Dislocation.
- Broken bones.
- Tendon and ligament tears and injuries.
A typical surgical consequence is neuropraxia. It is frequently brought on during surgery by
- Improper surgical positioning of the Body
- Poor body support padding
- The use of tourniquets and specific additional surgical tools
- Anaesthesia-related complications, such as chemical nerve damage or blood vessel narrowing that results in a cutoff of your blood flow
Other factors:
- Birthing a baby.
- Extractions of teeth.
- Endodontic treatments.
- Anaesthetic injections
Outside of a medical situation, the following are additional potential causes of neurapraxia:
- Car crashes
- Athletic injuries
- Falls
- Bullet wounds
If the neurapraxia occurs outside of a medical setting, it’s crucial that you let your doctor know precisely when the accident occurred in relation to when you first felt the symptoms. They can use this to determine how the damage is developing and if blood loss or compression is more likely to be the causes.
Symptoms of neuropraxia:
When you have neuropraxia, you could develop neuropathy. Neuropathy symptoms might include:
Neurapraxia can affect a variety of nerve types, and as a result, the severity and intensity of the injury’s symptoms might vary. Neurapraxia commonly manifests as:
- Vasomotor and sudomotor paralysis in the vicinity of the damaged nerve or nerves, Aberrant nerve sensitivity at the site of injury.
- At the site of the damage, there is numbness, tingling, and burning feelings have been noted as subjective sensory complaints. In general, there aren’t many objective sensory indications of touch, pain, heat, or cold.
- Muscles that are innervated by the damaged nerve or nerves exhibit flaccid paralysis as signs of motor neuron neurapraxia. Immediately after an accident, symptoms frequently only appear briefly and disappear. However, symptoms of severe neurapraxia might last for several weeks or months.
Neuropraxia symptoms may not develop right away after the injury but may do so a few weeks later. It might be brought on by inflammation, which compresses the nerve and damages it. Neuropraxia symptoms brought on by blood loss are transient, whereas those brought on by compression are persistent and result in a neurological obstruction. The following are neuropraxia symptoms.
- Numbness.
- Pain.
- Weakness.
- Tingling.
- Burning.
- Stinging.
- Motor skills decline.
- A shocking loss.
- Sensitivity to touch.
Neurapraxia symptoms might not show up right away after the injury. It can possibly take weeks for symptoms to manifest. In this instance, inflammation is typically to blame for damaging the nerve by squeezing it.
Compared to neurapraxia brought on by blood loss, compression-related neurapraxia typically causes a neural blockage to form more slowly and exhibit symptoms for a longer period of time. When there has been blood loss, the blockage, and its accompanying symptoms appear and disappear more quickly.
Where will neuropraxia be felt?
Near the damaged site, you get neuropraxia-like symptoms. There are various forms of neuropraxia, such as:
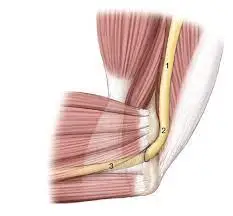
- Axillary neuropraxia: The nerve that sends impulses to your arm muscles and shoulder joint is injured. Your shoulder, arm, and hand could all experience symptoms.
- Brachial plexus neuropraxia: Your shoulder’s (brachial plexus) nerves are injured if you have brachial plexus neuropraxia. Your arms and hands receive impulses from your spinal cord thanks to these nerves. Symptoms are often felt in one arm.
- Radial nerve neuropraxia: The radial nerve, which transmits impulses from the back of the arm to the hand, is injured. Symptoms are often felt on the back of your hand or in your thumb, middle, and index fingers. The symptoms in the hand and back of the arm are brought on by radial nerve damage. The index and middle fingers, thumb, and back of the hand all exhibit signs of neuropraxia in these areas, which is caused by the radial nerve.
- Sural nerve neuropraxia: Your sural nerve is injured, which is referred to as neuropraxia. This nerve transmits electrical signals from your brain to your calf, heel, and foot. Symptoms are often felt in the foot and ankle.
Diagnosis:
Neurapraxia is challenging to diagnose, as are all severe peripheral nerve injuries. This indicates that incidents are frequently not reported.
The precise position of the block along a certain nerve can be determined by your doctor using nerve conduction tests. The tests gradually focus on a point along your nerve where the electrical signal can’t travel any farther.
Seddon classification:
There are three distinct categories and severity levels for nerve damage:
- Neurotmesis: The most severe type of nerve damage is called neurotmesis. Both the nerve and the nerve sheath are affected.
- Axonotmesis: It happens when the bulk of the nerve’s supporting components are still present yet there is still disruption of the nerve fibers. Wallerian degeneration frequently takes place close to the location of the damage.
- Neuropraxia: The least severe type of nerve injury is neuropraxia.
Neurapraxia can result from any of two types of mechanical nerve damage. Transient nerve damage frequently has a brief ischemia event or any kind of compression as its underlying causes. Demyelination and axonal constriction are two types of more severe nerve damage.
In some cases, it might be uncomfortable to diagnose neurapraxia due to the presence of significant neuropathic pain. The presence of neuropathic pain indicates that the nerve lesion is still active. Neurapraxia diagnosis is nearly often followed by a brief but thorough healing period.
To be sure that your symptoms aren’t being caused by even more serious nerve or tissue damage, imaging procedures like magnetic resonance imaging (MRI) may be required.
Consult your healthcare practitioner for a diagnosis if you were hurt or experience symptoms following surgery or trauma.
To check for nerve injury, your healthcare professional will do a physical examination. They could also request blood tests to:
- (CBC) Complete blood count.
- A kidney’s function.
- Liver performance.
- Thyroid activity.
What other exams are used by medical professionals to identify neuropraxia?
Nerve and muscle function tests, as well as imaging studies, may be prescribed by your healthcare physician. These examinations evaluate the degree of the injury and any nerve damage.
They may utilize:
- Electromyogram.
- MRI.
- Ultrasound of Peripheral nerve and muscle
- X-ray.
How Is Neuropraxia Diagnosis Conducted?
By physically examining the patient, the medical professional determines whether the patient has neuropraxia. The doctor may also suggest a number of laboratory blood tests, including those for thyroid function, erythrocyte sedimentation rate, complete blood count, kidney function, liver function, blood glucose, and vitamin B12 levels.
Additionally, the patient undergoes a routine needle EMG (electromyogram) study every six weeks that lasts from day two or three up to day six. The test helps identify nerve and muscle health during an injury and indicates any defects in nerve-to-muscle impulse transmission, nerve damage, or muscle dysfunction.
The test identifies any problems in nerve-to-muscle impulse transmission, nerve damage, or muscle dysfunction and aids in determining the health of the nerve and muscle during an injury.
Additionally, an ultrasound is used to check the continuity of peripheral nerves and muscles. Additionally, computed tomography (CT) scans aid in locating unreduced bone fractures that could obstruct the nerves and muscles in the affected body part.
In order to pinpoint the location of the nerve compression causing neuropathy, the doctor additionally suggests performing magnetic resonance imaging (MRI) of the pelvis and lumbar spine. MRIs are typically performed as soon as surgical and traumatic damage occurs.
Treatment of Neuropraxia
Responses to severe injury encompass the entire nerve. The degree of the nerve injury and the circumstances at the injury site determine how well the nerve will heal. Neurapraxia is one of the less severe types of peripheral nerve injury, hence recovery and therapy are not lengthy. Lesions in the nerve quickly recover once the cause of neurapraxia has been found and treated.
Neuropraxia is typically treated by a clinician utilizing conservative procedures. The doctor mostly advises limb support, physical therapy, splints, refraining from physical activity, and avoiding neuropathic pain drugs including antidepressants, analgesics, corticosteroids, anticonvulsants, etc.
Typically, neuropraxia cures on its own. Your healthcare provider can assist with pain management. They might advise:
Casts, splints, and braces.
RICE implies rest, ice, compression, and elevation.
Your doctor could advise physiotherapy for neuropraxia, such as range-of-motion exercises. Additionally, acupuncture and massage treatments might be beneficial, but only if your doctor suggests them.
Medical treatment:
Your doctor might advise you to take particular medications to treat your symptoms, such as:
- Antidepressants.
- Corticosteroids.
- NSAIDs, or non-steroidal anti-inflammatory medications.
Non-surgical therapy:
Non-operative methods are frequently used to treat and cure neuropraxia. The major objectives of treatment are to continually preserve joint mobility, prevent antagonistic contraction of the paralyzed muscles, and maintain the normal nourishment of the paralyzed muscles.
Because it can keep the paralyzed muscle in a relaxed condition, a splint is frequently utilized in neurapraxia patients. The splint guards against the paralyzed muscle being overextended by non-paralyzed antagonists or the gravitational pull.
The joints must constantly engage in passive motion during the neurapraxia recovery period in order to maintain adequate mobility. The limb has the highest chance of benefiting from the recovery of nerve function if joints are kept flexible.
Non-steroidal anti-inflammatory drugs can also aid in lowering swelling at the site of the injury.
It is recommended that the muscles affected by neurapraxia be kept warm at all times in addition to these non-operative treatments. Heat is used to promote circulation in the limb.
Active exercises prolong rehabilitation and treatment after the muscle has regained its ability to move on its own. During these initial stages of the return to active mobility, physical therapy and occupational therapy are frequently used as treatment options. Neurapraxia can be totally treated non-operatively in almost all patients.
Field treatment of cervical cord neurapraxia:
Medical experts claim that after an athlete experiences an episode of cervical spinal cord neurapraxia, the head and neck should be stabilized before a complete neurological examination. Injured individuals should be transported to a hospital for evaluation if the injury is considered severe. Athletes who experience severe neurapraxia episodes are advised to speak with a spinal or orthopaedic doctor. The athlete is able to leave the playing field in cases of mild neurapraxia. The athlete is still encouraged to contact a doctor, though.
Surgical treatment:
Hematoma nerve compressions are instantly released, however, surgical decompression is required in the case of compressions brought on by trauma or fractures.
Fasciotomy might also be necessary if compartment syndrome exists.
After three to six months, if the patient has not recovered, surgical intervention may be necessary to treat the scar tissue that may be impeding the healing. In order to treat the patient, the doctor performs nerve decompression and transposition.
By controlling pain and giving the patient psychological support, physical rehabilitation is accomplished. In cases of peripheral nerve injury, pain management is exceedingly difficult since burning and dysesthesia are created along the nerve distribution. Anticonvulsants, tricyclic antidepressants, and baclofen, as well as some short-term treatment with NSAIDs (nonsteroidal anti-inflammatory medications), opioids, and Tramadol, may be prescribed in such circumstances by the doctor.
The doctor also suggests that patients take care to prevent repetitive injury.
Complications:
Most neuropraxic patients make a full recovery. However, some people experience issues like:
- Inflammation.
- Persistent numbness, weakness, or discomfort in the nerves.
- Tissue scarring close to the injury site.
- If scar tissue forms, surgery might be necessary. In order for your nerve to heal, surgeons must remove any scar tissue or nerve compression.
- Mental health problems.
- Neuropathic pain, apathy, and weakness that lasts a long time.
- Muscle wasting is brought on by a flawed diagnosis.
- Financial losses.
- Tissue scars at the areas of damage.
Most of the time, neurapraxia won’t require any particular care. If the nerve damage is ignored for a few days to a few weeks, it will recover on its own.
Differential Diagnosis:
The nerve disorder known as neuropraxia can resemble a number of diseases of the muscles and nerves. As a result, the doctor should be cautious while making the diagnosis. These alternative diagnoses consist of:
- Axonotmesis.
- Inflammation of the nerves.
- Myelopathy.
- Muscle ailments.
- Diabetic nerve damage.
- Neuropathy is caused by paraneoplastic disease.
- Illness of the upper nervous system.
- Radiculopathy.
- Neurotmesis.
- Spine-cord injury.
- Leprosy is one example of infectious neuropathy.
Prognosis for neuropraxia:
Neurapraxia recovery rates are excellent. Within 1-4 weeks, the nerves ought to be able to recover on their own. You will have fully restored all sensations and bodily functions by this point.
Inform your doctor regularly about how your neurapraxia is improving. They’ll want to make sure you quickly regain all of your motor and sensory abilities.
Summary
Neuropraxia is a mild form of nerve injury where there is temporary dysfunction without structural damage to the nerve fibers. It is typically caused by trauma or compression to the nerves and can result in symptoms like weakness, numbness, and tingling.
Neuropraxia often resolves on its own within a few weeks to months, and treatment involves rest, immobilization, and physical therapy. If symptoms persist or worsen, medical attention should be sought for further evaluation and management.
FAQs:
Transient functional loss without a corresponding loss of nerve continuity is seen in neurapraxia. In axonotmesis, the perineurium and epineurium are preserved while the nerve axon and surrounding myelin are completely disrupted.
Neurapraxia is a transient disorder that causes brief damage to the myelin sheath but leaves the nerve unharmed; as a result, Wallerian degeneration does not take place.
Neurapraxia is challenging to diagnose, as are all severe peripheral nerve injuries. This indicates that incidents are frequently not reported. The precise position of the block along a certain nerve can be determined by your doctor using nerve conduction tests.
Your nerve should heal over the course of 6 to 12 weeks if it has been traumatized or bruised but not cut. After around 4 weeks of’rest’ following your injury, a cut nerve will grow at a rate of 1mm each day. Some people report ongoing progress over several months.
Although they can grow back and repair at a rate of roughly an inch per month, nerve cells usually experience delayed and incomplete recovery. The nerve sheath and underlying neurons are completely cut in this type of total nerve damage.





One Comment