Spina Bifida
Table of Contents
What is a Spina Bifida?
Spina Bifida, in general, is identified as “a neural tube defect (NTD) that results when the inferior neuropore does not close, although it has also been recommended that a closed tube can reopen in few cases. Developing vertebrae do not close around a defective neural tube, resulting in a bony defect at the distal end of the tube.” The exact cause of spina bifida is unrevealed but there can be incorporate genetic, environmental, and dietary factors that may put at risk the development of the condition in some people.
The most commonly researched factor is the association of lower levels of maternal folic acid. Folic acid is a vitamin existing in so many foods and is frequently added to breakfast cereals. It may also be established as a supplement in the pharmacy. It is thought to be included in the development and formation of fetal cells and tissues, therefore, it is recommended that folic acid should be taken regularly in the upcoming months prior to conceiving and also at the time of pregnancy.
What are the different types of spina bifida?
There are two types of spina bifida:
Spina bifida cystica
- There is a fault in the spinal cord and the lining of the spinal cord is pushed out through the fault.
- Spinal cord tissue can also be pushed outside through the defect.
- The two types of spina bifida cystica are known as meningocele and myelomeningocele:
Meningocele
- Spina bifida meningocele is the infrequent type of spina bifida.
- The protective membranes (the meninges) nearby the spinal cord are pushed out in the middle of openings in the vertebrae.
- The meningocele is sometimes protected by a layer of skin.
- There are of course no spinal cord nerves in the protruding sac. The membranes may generally be detached by surgery. The symptoms may be very different.
- Sometimes there are fewer or no symptoms or problems.
- Others can have extreme weakness of the legs and also bladder and bowel problems.
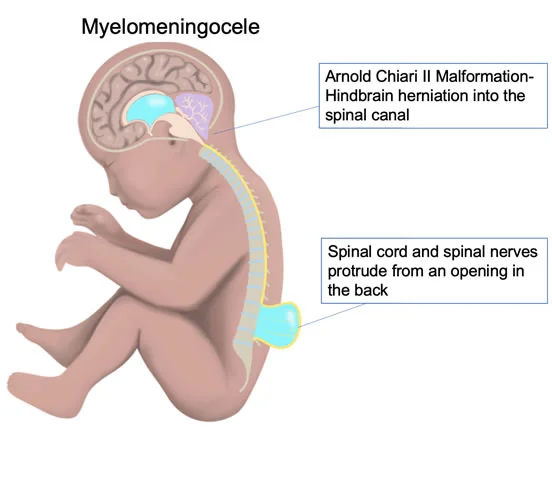
Myelomeningocele
- This is the most usual type of spina bifida. About one pregnancy in every 1,000 pregnancies is involved in the UK.
- The spinal column residue unlocks along the bones making up the spine.
- The membranes and spinal cord push out to build a sac on the baby’s back.
- This sometimes leaves the nervous system at risk of infections that can be some time life-threatening.
- In most cases of myelomeningocele, surgery may be performed to close the defect.
- However, harm to the nervous system will generally already have taken place.
- The nerve damage may cause a range of symptoms, incorporating weakness (paralysis) of the legs and loss of feeling in the skin of the legs.
- There can also be problems with passing urine and feces, stools, or motions.
Spina bifida occulta
- Spina bifida occulta occurs in about 1 in every 10 people and infrequently causes any symptoms or problems.
- Spina bifida occulta is the minimum severe type of spina bifida.
- The opening in the spine is very tiny, with one or more of the bones of the spine(vertebrae) not perfectly formed. The opening in the spine is protected with skin, so the gap is not noticeable from the outside.
- Spina bifida occulta does not normally cause any symptoms and most individuals are unaware they have the condition.
- In some cases, no treatment is needed.
- In other cases, there can be some symptoms, like bladder and bowel problems, or an abnormal curve of the spine (scoliosis).
Characteristics/Clinical Presentation
Spina Bifida Occulta represents with:
- Depression or dimple in the lower back
- A small patch of dark hair
- Soft fatty deposits
- Port-wine nevi (deep red-purple macular lesions).
Spina Bifida Meningocele represents with:
- A Saclike cyst that protrudes the outer side of the spine
- Spina Bifida Occulta and Meningocele generally do not exist with neurological deficits; although, bowel and bladder incontinence can exist depending on the level of the lesion.
Spine Bifida Myelomeningocelee produces more severe impairments:
- Flaccid or spastic paralysis
- Bladder incontinence
- Musculoskeletal deformities (Such as scoliosis, hip dysplasia, hip dislocation, club foot, and hip/knee contracture)
- Hydrocephalus, Solitary with Type I or II Arnold Chiari malformation
- Trunk hypotonia
- Delayed automatic postural reactions.
Signs and Symptoms of Spina Bifida
Spina bifida can cause both physical and cognitive limitations (problems) ranging from mild to severe. How severe these limitations relate on:
- The size and location of the inception in the spine.
- How much of the spinal cord and nerves are involved?
- Other problems are common with spina bifida.
- When the defect is higher in the spine, it generally causes more physical problems.
- Spina bifida in the lower levels of the spine and spinal cord is more usual.
- The Spina Bifida Association gives a helpful graphic showing the levels of function.
- Relate on the defect location, the areas affected may be the:
- The cervical section (neck area)-controls the arms and hands.
- Thoracic section (upper back area); command trunk and abdomen.
- Lumbar section (lower back area); controls legs.
- The sacral section (below the low back into the tailbone area); controls parts of the legs, as well as the bowel and bladder.
Below given are some common symptoms of spina bifida:
- Difficulty moving the legs for activities like crawling and walking.
- Problems with blood flow in the legs from restricted muscle use.
- This enlarges the risk of pressure sores and poor healing of wounds.
- Delicate bones and joints, or bones that are curved or misshapen.
- Weak or paralyzed legs from harm to the spinal cord and nerves.
- Reduced sensation or feeling.problems going to the bathroom, like trouble controlling both bowel and bladder functions.
- Problems with sexual function.Sensitive skin, including latex allergies.
Co-morbidities:
Osteopenia or Osteoporosis:
- Osteoporosis: Because of the reduced level of activity of many of these people this will ultimately cause a reduced bone density that will put them at risk for fractures.
Obesity:
- Because of reduced activity and a sedentary lifestyle.
Complications:
Tethered Cord Syndrome
- The spinal cord becomes fixated and starts to stretch which may cause further neurological deterioration.
Urinary Tract Infection
- Frequently individuals who have bowel and bladder incontinence will feel recurrent urinary tract infections.
Decubitis Ulcer
- These happen because of altered sensations an individual can experience from the neurological deficit.
Pathology
- The neural groove develops to create the neural tube around day 20 after conception.
- In usual development, the upper end is supposed to close on day 25 and the lower end is generally to close on day 27.
- Three opportunities could cause unusual closure of the neural tube.
- If the hyaluronic acid matrix or actin microfilaments have abnormalities prior on, the neural tube will not close.
- If an overgrowth takes place over the caudal end the neural tube will not close, but this happens later in development.
- The last chance for the tube not to close accurately happens when the glycoproteins that typically hold the cells together at the time of closure fail to adhere to the tube together.
- There is no perfect reason known for the cause of Spina Bifida, but there are a variety of environmental and genetic factors that can be potential risk factors.
Mother’s nutrition:
Folic acid- Minimum than 400 µg of folic acid per day.
Increased: Vitamin A, valproic acid, solvents, lead herbicides, glycol ether, clomiphene, carbamazepine, aminopterin, alcohol.
Genetic involvement:
- 3%-8% reappearance rate for parents who already conceived a child affected with spina bifida.
- The incidence rate maximizes 20x’s if the parents already have a child affected with a neural tube defect.
- In contrast to African-Americans, Caucasians usually have it, and Hispanics have a higher incidence rate than non-Hispanics.
Environmental Factors:
- Radiation and viruses can have an impact on developing fetuses.
Systemic Involvement
Occulta and Meningocele
- No neurological dysfunction is typically present.
Myelomeningocele
- Permanent neurological and musculoskeletal deficits are present.
Neurological
- Muscle weakness, bowel and bladder problems, seizures, paralysis, absent reflexes, sensory disfigurement.
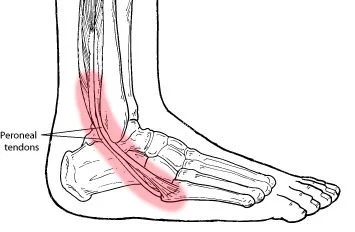
Musculoskeletal
- Hip dislocation, syringomyelia, scoliosis, foot and ankle deformities.
Diagnostic Tests/Lab Tests/Lab Values
Before Birth
- Alpha-fetoprotein blood test when 16-18 weeks pregnant.
- Amniocentesis can be done to further identify the cause of an increase in alpha-fetoprotein.
- Ultra-sound of the spine.
After Birth
- X-ray, MRI, CT scan.
- Meningocele and myelomeningocele are identified on the physical exam.
What are the complications of spina bifida?
Complications of spina bifida can differ from no problems to severe physical disabilities. Most individuals with spina bifida are of normal intelligence. The problems caused by spina bifida depend on the size and position of the defect in the spine, whether it is covered, and which spinal nerves are included.
All nerves situated below the defect will be involved to some extent. Therefore, the higher the defect takes place on the back, the greater the amount of nerve damage and loss of muscle power and sensation.
Hydrocephalus
- Most children with myelomeningocele will also develop an excess of fluid nearby the brain – this fluid is known as cerebrospinal fluid (CSF).
- This causes maximum pressure in the brain (hydrocephalus).
- Hydrocephalus needs to be treated as early as possible, as the pressure on the brain may cause brain damage.
- Hydrocephalus is frequently treated by an operation to insert a hollow tube (shunt) from the brain to the tummy (abdomen) to drain the excess fluid.
Chiari II malformation
- Myelomeningocele may also be connected with a serious condition called a Chiari malformation.
- This condition includes part of the brain being pushed down and out of the skull and into the spinal canal in the neck.
- This may lead to squashing (compression)of the spinal cord.
- This can cause a variety of symptoms incorporating difficulties with feeding, swallowing, breathing problems, and arm weakness.
- A Chiari malformation can also cause blockage of the CSF (hydrocephalus).
Meningitis
- Few newborn babies with myelomeningocele can develop meningitis, an infection in the lining of the brain and spinal cord(meninges).
- Meningitis can cause brain injury and may be life-threatening.
Other complications
Spina bifida can be connected with abnormal curvature (scoliosis) of the spine. A child with spina bifida can also have leg and foot abnormalities – such as abnormal hips, unequal leg length, or club foot.
Bladder problems
- Such as problems passing urine or loss of control passing urine (urinary incontinence).
Bowel problems
- Like, as passing hard poo (constipation), frequent watery loose poo (diarrhea), or loss of control of passing poo(incontinence).
Cognitive problems
- such as learning disabilities, incorporating difficulty paying attention, problems with language and reading, and trouble learning maths.
- However, most individuals with spina bifida have normal intelligence.
- Some children with myelomeningocele develop a condition called progressive tethering (tethered cord syndrome).
- The spinal cord becomes poked to the overlying membranes and bones (vertebrae).
- This causes the spinal cord to become stretched as the child grows.
- This may cause a loss of muscle power in the legs. It may also cause bowel and bladder problems.
- Early surgery on a tethered spinal cord can prevent more damage to the spinal cord.
Treatment of Spina bifida
Medical Management
In babies with myelomeningocele, irreparable nerve damage has likely already taken place and ongoing care from a multispecialty team of surgeons, physicians, and therapists is usually needed. Children with myelomeningocele can need more surgery for different variety of complications. Medical management for complications — like weak legs, bladder and bowel problems, or hydrocephalus — typically begins soon after birth.
Based on the severity of spina bifida and the complications, treatment options may include:
Walking and mobility aids-
- Some babies may initiate exercises to prepare their legs for walking with braces or crutches when they are older.
- Some babies may need walkers or a wheelchair.
- Mobility aids, along with regular physical therapy, may help a child become independent.
- Even babies who require a wheelchair can learn to function very well and become self-sufficient.
Bowel management
- It can include oral medications, suppositories, enemas, surgery, or a combination of these approaches.
Bladder management-
- It can include medications, using catheters to empty the bladder, surgery, or a combination of treatments.
Management of other complications-
- Special equipment like bath chairs, commode chairs, and standing frames may help with daily functioning.
- Whatever the issue — orthopedic complications, tethered spinal cord, GI issues, skin problems, or others — most spina bifida complications may be treated or at least managed to increase the quality of life.
Spina Bifida Physiotherapy Management
Physiotherapy might not be the initial treatment method you think of when it comes to spina bifida, but, in fact, physiotherapy management is a necessary healthcare partner for persons with spina bifida, as well as their family and carers. Physiotherapists may help children and adults with spina bifida by helping them gain and maintain mobility and overall, function at their best throughout each and every stage of life. Physiotherapists will also work alongside other healthcare providers like orthopedists and occupational therapists for a more holistic treatment plan that expands into every aspect of life.
What Is A Spina Bifida Physiotherapy Assessment?
When someone with spina bifida first starts working with a physiotherapist, an assessment might incorporate:
- Questioning about birth and developmental history to help get an understanding of where they might fall on a normal development progression
- When could they hold their head up, roll over, crawl, or walk?
- Asking about general health.
- Have they been sick or in the hospital? When was their last GP visit?
- Addressing parental concerns and what the parents hope to accomplish in the treatment plan.
- A physical examination to calculate their height and weight, observe movements, balance, and coordination, and complete a tactile test of muscle strength, flexibility, and tone.
- A motor skills examination to test motor development during sitting, crawling, walking, and hand use.
- The test might also look at vision, language skills, and some other developmental milestones.
Some physiotherapy spina bifida treatment plans include:
- Infant positioning needs
- Parent and family education during infancy.
- Early intervention is to give physiotherapy techniques to encourage the healthy development of strength, balance, and motor skills while teaching parents to incorporate these techniques into their daily lives.
- School-based physiotherapy to work with babies with spina bifida on school-related motor skills and tools to help with any neurological deficiencies.
- Giving the appropriate equipment to help children and adults with spina bifida incorporates braces, walkers, and wheelchairs.
- Prevention of other possible issues incorporating obesity through the encouragement of fitness-based activities to promote long-term health and well-being.
- Further, the physiotherapist will often work in tandem with other healthcare providers to take a holistic approach to spina Bifida treatment.
- And, just as crucial as working with the patient is educating the parents and carers as well — a necessary part of the process that physiotherapists may also give.
General Exercise
General Strength Training Guidelines and Safety Considerations–
Many people with spina bifida have a latex allergy. If this is the case, always check beforehand to be sure that the exercise instrument is not made of latex. Instrument manufacturers like Thera-band offer latex-free versions of their products.
Breathing
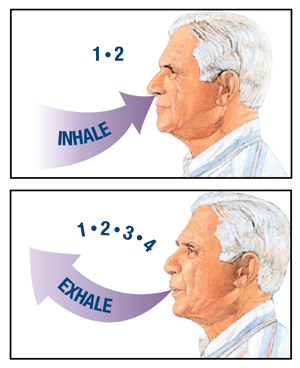
- Breathe normally while doing the exercises.
- Do not try holding your breath at any time.
- To make sure that the patient is not overdoing the exercise, you should be able to maintain a normal conversation throughout.
- If you are exercising solo, it is best to count out loud while doing the exercise.
- A useful technique is to slowly count 1-2 when doing the exercise activities, and count 1-4 when returning to the starting position.
Posture
- Sit up straight with both feet planted firmly on the floor.
Back Support
- To make sure that the lower back is supported, roll up a small towel and place it behind the back.
Rest
- Give the muscles a day’s rest between strength training sessions.
- The muscles can feel sore a day or two after you have started a new exercise.
- If the person is sore, wait until the soreness has diminished before going back to strength training.
- Consult with the doctor if the muscle soreness lasts longer than two days.
- Furthermore, if muscle soreness last 2-3 hours after exercise, you know you have done too much.
- During the next exercise session, reduce the number of repetitions, sets, or weights until you find the right settings for you.
Some Physical Activity Programs-
Take the current fitness and activity level into consideration to find a program that works for you, but this is an example of what a weekly plan could ultimately be visually like once you work up to doing some sort of activity on a daily basis. Include as much variety as possible.
- Monday: Walk for 30 minutes either outside, strength train using weights for 20 minutes, or stretch for 10 minutes.
- Tuesday: Ride a stationary bike at the local gym for 20 minutes and stretch for 5 minutes.
- Wednesday: Walk for 30 minutes around the local indoor mall, strength train using elastic bands for 20 minutes, and stretch for 10 minutes.
- Thursday: Perform a dance video at home for 30 minutes, and stretch for 10 minutes.
- Friday: Walk for 30 minutes on a treadmill at the local gym, strength train using weights or elastic bands for 20 minutes, and stretch for 10 minutes.
- On the weekends: Go hiking in a local park, swim at an indoor or outdoor pool, or ride an outdoor bike (three-wheeled bicycles are popular).
Range of motion and strengthening exercises
Neck Stretch
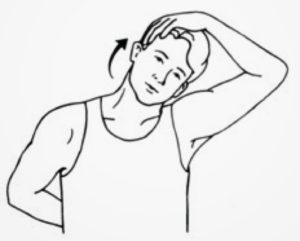
- A child with Spina Bifida is performing a neck stretch.
- Sit upright, maintaining a tall posture.
- Tilt the head to the side, moving the ear toward the shoulder.
- Hold for 20 seconds. Return the head to an upright position.
- Repeat on the other side.
- This stretches the side of the neck.
Wrist Flexion/Extension

- A child with Spina Bifida is performing Wrist Flexion/Extension exercises from a seated position.
- Extend the arm and hand forward with the palm facing outward.
- Bend the wrist back toward the body and assist the movement with the other hand.
- Hold for 10-30 seconds.
- Then straighten the wrist and assist the movement with the other hand.
- Hold for 20-30 seconds.
Overhead Stretch

- A child with Spina Bifida is performing an Overhead Stretch.
- Sit on a comfortable chair with back and neck straight and feet planted gently on the floor.
- Raise arms up overhead. Interlock fingers above the head, if possible, for a stronger stretch.
- Extend the arm with palms facing up toward the sky, straightening the elbow.
- Hold for 20-30 seconds.
- This stretches the muscles of the shoulder.
Upper Trunk Flexion

- A child with Spina Bifida is performing an Upper Trunk Flexion exercise.
- Sit with proper posture. Eyes looking forward, and feet planted firmly on the floor.
- Bring the chin to the chest and round the upper trunk keeping the head, neck, and shoulders relaxed.
- Hold for 20-30 seconds, keeping the bottom firmly on the seat.
- Gently straighten the back and then bring your head back to the neutral/starting position.
- Do it again.
Triceps Stretch

- The child with Spina Bifida is performing a Triceps Stretch from a seated position.
- Stand or sit with proper posture.
- Bring one arm across the body.
- Using the other hand, slowly pull the elbow farther across the body.
- Experience the stretch along the back of the shoulder.
- Hold for 20-30 seconds.
- Release the stretch and switch arms.
- Perform the stretch 2 times with each arm.
Butterfly Chest Stretch
- A child with Spina Bifida is performing a Butterfly Stretch from a seated position.
- Sit with proper posture and place the hands behind the neck.
- Slowly and gently bring the elbows backward, being careful not to pull on the neck.
- When the elbows are as far back as they will go, pause briefly.
- Experience the stretch in the shoulders and chest.
- Hold for 20-30 seconds.
- Relax and return to the starting position.
- Do it further.
Trunk Rotation

- The child with Spina Bifida is doing a Trunk Rotation exercise from a seated position.
- Stand upright and slowly rotate the trunk and shoulders to one side.
- Use the arms to help rotate.
- Repeat in opposite direction.
- You should feel a stretch in the trunk.
Hamstring Stretch

- A person with Spina Bifida is doing a Hamstring Stretch from a seated position.
- Sit in a chair and perform the extension of one leg forward.
- Keep your knee straight and slowly lean toward the toes, attempting to maintain a straight back.
- Hold for 20-30 seconds.
- Repeat on the other leg.
- The patient should feel a stretch in the hamstrings.
- Do not do this exercise if it increases leg pain.
Strengthening exercise
Seated Strengthening Exercises with Elastic Band. For seated strengthening exercises, sit up straight with both feet planted firmly on the floor. The patient can want to use a rolled-up towel to support the lower back. Begin with a few repetitions and progress to 12 as you maximize your strength.
Elbow Flexion
- Put the band across (left to right) on the seat of an arm-free chair or wheelchair.
- Correct the length of the band so that there is enough slack to give some resistance to the side of the arm you are working.
- Sit in the chair or wheelchair on edge of the band.
- Muffle the band around the hand with the palm facing upward.
- Tie the exerciser at knee level on the side of the chair or across the legs.
- Bend the elbow holding the band.
- Hold.
- Return to the beginning position and do the desired number of repetitions.
Elbow Extension
- A child with Spina Bifida is performing an Elbow Extension from a seated position.
- Place half of the band across (left to right) on the seat of an arm-free chair.
- Correct the length of the band so that there is enough slack on the side of the arm you are working.
- Sit on the band. Be sure that the band crosses diagonally across the back.
- Muffle the band around the hand with the elbow bent, and the palm facing downward.
- Straighten the elbow.
- Hold.
- Return to the initial position and do the desired number of repetitions.
Forward Reach
- A child with Spina Bifida is doing a Forward Reach exercise from a seated position.
- Begin with a band muffled around the upper back.
- Grip both ends of the band with elbows bent and palms facing inward.
- Push the band forward, extending the elbows out and keeping their shoulder height.
- Gently return to the initial position and do the desired number of repetitions.
Upright Row
- A child with Spina Bifida is doing an Upright Row exercise from a seated position.
- Place the center of the band under both feet and grip each end of the band with palms facing down.
- Pull the band upward toward the chin, lifting your elbows outward.
- Gently return to the initial position and do the desired number of repetitions.
Overhead Reach
- A child with Spina Bifida is doing an Overhead Reach exercise from a seated position.
- Place the center of the band under the feet and grasp each end of the band with palms facing forward.
- Lift arms upward toward the seeling, extending the elbows with palms facing forward.
- Do not lift above the shoulders if it causes pain.
- Gently return to the starting position.
Hip Flexion
- A child with Spina Bifida is doing a Hip Flexion exercise from a seated position.
- Sit on a comfortable surface, the exercise band around both thighs.
- Lift up the knee to the chest, keeping the opposite leg stationary.
- Hold.
- Return to the initial position and repeat the desired number of repetitions.
Hip Abduction
- A child with Spina Bifida is performing a Hip Abduction exercise from a seated position.
- Sit on a firm surface, the exercise band around both thighs, near the knees, or tied to the opposite side of the chair (as shown in the photo).
- Lift one leg gently and pull it away from the other leg.
- Hold.
- Return to the initial position and repeat the desired number of repetitions.
Leg Press
- The child with Spina Bifida is performing a Leg Press from a seated position.
- Loop the middle of the band around the foot twice with the knees bent.
- Hold both ends of the band at the waist.
- Keeping the ends of the band at the waist, extend the knee to straighten the leg.
- Gently return to the initial position and do the desired number of repetitions.
- Repeat on the opposite leg.
Neonatal physiotherapy:
prone lying facilitate
- Teach the mother to put the baby in a prone position during playtime, preferably on the floor.
- The passive movement must be given in the full range of motion possible to all joints starting with the toes, tarsal joints, ankle, knee, and hip.
- Mother must teach how to lift up the baby and move.
- Arm movement may be started as soon as possible as the baby responds to the exercise to strengthen the shoulder girdle.
Knowledge of developmental progress the milestone of a normal child then starts to roll over, sitting up.
Play therapy with using toys -facilitate mid-line activity, Bridging, knee to chest.
Ambulation
- When the child is ready to stand, an assessment needs to be made of the degree of support needed from orthosis.
- A degree of support is necessary according to the neurological level of affection.
Surgical management
Surgery before birth
- Nerve function in babies with spina bifida may worsen after birth if spina bifida is not treated.
- Prenatal surgery for spina bifida (fetal surgery) takes place prior to the 26th week of pregnancy.
- Surgeons open up the pregnant mother’s uterus surgically, open the uterus and repair the baby’s spinal cord.
- In select patients, this procedure may be performed less invasively with a special surgical tool (fetoscope) inserted into the uterus.
- Research suggests that children with spina bifida who had fetal surgery can have decreased disability and be less likely to need crutches or other walking devices.
- Fetal surgery can also decrease the risk of hydrocephalus.
- Ask the doctor whether this procedure can be appropriate for you.
- Discuss the potential benefits and risks, like possible premature delivery and other complications, for you and your baby.
Cesarean birth
- Too many babies with myelomeningocele tend to be in a feet-first (breech) position.
- If the baby is in this position or if the doctor has detected a large cyst or sac, cesarean birth can be a safer way to deliver the baby.
Surgery after birth
- Myelomeningocele needs surgery to enclose the opening in the baby’s back within 72 hours of birth.
- Doing the surgery as soon s possible may help to reduce the risk of infection connected with the exposed nerves.
- It may also help prevent the spinal cord from more trauma.
- At the time of the procedure, a neurosurgeon places the spinal cord and exposed tissue inside the baby’s body and covers them with muscle and skin.
- At the same time, the neurosurgeon can place a shunt in the baby’s brain to control hydrocephalus.
How can spina bifida be prevented?
- The best way to prevent the baby from having spina bifida is to take folic acid supplements both before and at the time of pregnancy.
- It is suggested that all women who might get pregnant should take a daily supplement of folic acid.
- Folic acid should be taken for the first twelve weeks of pregnancy due to this is when the baby’s spine is developing.
- If you have an improved risk of having a child with spina bifida you can need a higher dose of folic acid.
- For example, you are at improved risk if you have diabetes or you are taking medicines to treat epilepsy.
- It is also very necessary to eat food that is rich in folic acid.
- These foods involve dark green vegetables, egg yolks, and some fruits.
- Many foods have folic acids added – such as some breakfast cereals, some bread, flour, pasta, and brown rice.
FAQ
Many babies with spina bifida live into adulthood with the correct treatment and care. The approximate mean age for a person with spina bifida is 40 years.
weakness or total paralysis of the legs. Bowel incontinence and urinary incontinence. loss of skin sensation in the legs and around the bottom – the baby is not able to feel hot or cold, which may lead to accidental injury.
John Mellencamp, also known as John Cougar and John Cougar Mellencamp born on October 7, 1951. As a child in Seymour, IN, Mellencamp had suffered a number of setbacks, involving being born with a neural tube defect called spina bifida that necessitated a lengthy hospitalization as a baby.
Spina bifida is more usual among white people and Hispanics, and women are affected more often than males. Although doctors and researchers do not know for sure why spina bifida takes place, they have identified some risk factors: Folate deficiency.
In the early 1950s, most children born with spina bifida did not live long.





2 Comments