Systemic Disease
Table of Contents
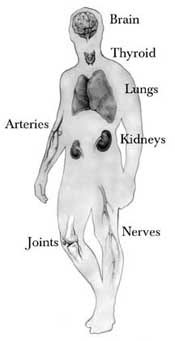
What is systemic disease?
A systemic disease is one that harms a number of organs and tissues or harms the body as a whole. Systemic diseases harm the entire body.
The hands, being composed of many types of tissue, including blood vessels, nerves, skin and skin-related tissues, bones, and muscles/tendons/ligaments, may look changes that reflect a disease that affects other areas of, or even the whole body (systemic disease). The hands may look changes noticed by the patient or his/her hand surgeon even previous the systemic disease is detected.
Under are a number of examples.
Examples of Systemic Diseases
Arthritic Swelling
- Arthritic swelling of the middle joint of a finger is known as a Bouchard’s node. The swellings at the little finger joints are known as Heberden’s nodes.
Buerger’s Disease
- This is one type of occlusive vascular disease that may harm the fingers (see Vascular Disorders). It is due to an inflammatory disease known as vasculitis and is typically associated with smoking. This disease affects the medium and small arteries, so it sometimes affects the fingers and toes. The disease may present as a painful and badly healing wound or ulcer/gangrene at the fingertip. The involvement of multiple fingers is common. The primary treatment is to quit smoking. Amputation is sometimes necessary.
Dactylitis
- This case of dactylitis was connected with psoriatic arthritis. In this photo, the swelling extends from the palm to include the ring finger out to the little joint. Stiffness is common. There also may be pain. This swelling may be increased with medicines for the problem causing it.
Mucous Cyst
- This type of cyst is known as a mucous cyst. If the skin becomes thin, the cyst may break resulting in the drainage of clear sticky fluid. The outcoming break in the skin may allow bacteria to reach the nearby joint, causing a joint or bone infection.
Red Dots
- The small red dots seen above are in the thin area of the skin around the nail. They may also happen in the thicker pink part. This has been look in dermatomyositis, systemic lupus, and scleroderma.
Leukonychia
- Leukonychia can be looked at by viral infections, intestinal and kidney diseases, poisoning, and medicines. The nail may come loose from the nail bed because of fungal infections or another cause.
Red Streaks
- Red streaks look in the fingernail area can be due to hemorrhage (bleeding). These are known as splinter hemorrhages and have been seen in endocarditis (heart infection), although also reported in psoriasis, and trichinosis.
Psoriasis
- Psoriasis usually affects the nail and nail bed. Pits in the nail, loosening, blood streaks beneath the nail, and other changes may happen. A psoriasis skin patch is look in the middle.
“Pincer” Nail
- This “Pincer” nail with an abnormal side-to-side shape curve can be looked at as birth or simply due to aging. However, it can be caused by changes in the bone beneath because of disease (gout in this case).
Pyogenic Granuloma
- This is a fleshy, moist, easily bleeding mass/lump that can harm the fingers, although it has been reported in many other body areas. In the fingers, it is usually found after trauma to the skin. If there are multiple or recurring lumps, it may be because of the effects of medications or pregnancy. The most effective treatment is surgery to remove the lump, yet if it is due to medication, stopping the use of the medication can help.
Terry’s Nails
- Fingernails will appear milky white/opaque, except for a little band of pink/red at the end of the nail bed. This appearance was 1st reported to be associated with liver disease and has also been reported with congestive heart failure, type II diabetes, and aging.
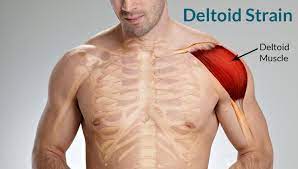
Physical Therapy Management
- Exercise is beneficial for patients with SD because it decreases their muscle weakness while simultaneously improving their muscle endurance. Physical therapists can play a main role for patients with SD during and between exacerbations. The patient’s requirements for physical therapy will vary greatly depending on the systems involved.
- Education: It is essential for patients with skin lesions to have appropriate education on a good way to care for their skin and to ensure they do not experience additional skin breakdown.
- Aerobic Exercise: One of the most common impairments that patients with SD experience are generalized fatigue which can limit their activities throughout the day. Graded aerobic exercise programs are more successful than relaxation techniques in reducing the fatigue levels of patients with SD. Aerobic activity causes many with SD to feel much good. The aerobic exercise program may consist of 30-50 minutes of aerobic activity (walking/swimming/cycling) with a heart rate corresponding to 60% of the patient’s peak oxygen consumption. Both aerobic exercise and range of motion (ROM)/muscle strengthening exercises can increase the energy level, cardiovascular fitness, functional status, and muscle strength in patients with SD (aerobic exercise for 20-30 minutes at 70-80% of their maximum heart rate,3 times a week for 50 minutes sessions).
- Energy Conservation: Physical therapists can educate patients on appropriate energy conservation techniques and the best ways to protect joints that are susceptible to harm.
- Additionally, physical therapists and patients with SD should be aware of signs and symptoms that suggest a progression of SD involving those associated with avascular necrosis, kidney involvement, and neurological involvement.
FAQs
Systemic disorders can have gastrointestinal (GI) manifestations which are characterized by nausea, vomiting, diarrhea, constipation, abdominal pain, jaundice, and abnormal liver function tests. These gastrointestinal symptoms can be signs of various immunologic, infectious, and endocrine diseases.
Sarcoidosis.
Neoplasm.
Serositis.
Metastatic Carcinoma.
Lesion.
Protein.
Rheumatoid Arthritis.
Systemic Lupus Erythematosus.
A severe systemic disorder that is already life-threatening, is not always correctable by the operation (examples include coma, acute myocardial infarction, respiratory failure requiring ventilatory support, renal failure requiring urgent dialysis, bacterial sepsis with hemodynamic instability).
adjective [usually ADJECTIVE noun] A systemic problem affects the whole of an organization or place, not just some parts of it.
Systemic diagnosis is a way of understanding a problematic situation by evaluating various systemic levels and their interaction.
The diagnosis of an underlying disease is confirmed through laboratory testing and physical examination. Rather than ordering a broad spectrum of unnecessary tests, the clinician must correlate the patient’s history with symptoms and physical signs to tailor laboratory testing to the individual.
Systemic treatments are drug therapies that work throughout the whole body. They can be given as an injection, infusion, or oral medication. They include chemotherapy, hormonal treatment, targeted therapy, or immunotherapy.
Diabetes Mellitus is a multi-systemic disorder influencing the regulation of blood glucose.
(sis-TEH-mik) Affecting the entire body.