SPASTICITY IN HEMIPLEGIA :
Table of Contents
INTRODUCTION :
- Spastic hemiplegia is a neuromuscular condition of spasticity that results in the muscles on one side of the body being in a constant state of contraction.
- It falls under the mobility impairment umbrella of cerebral palsy.
Mechanism :

- Damage to the corticospinal tract leads to injury on the opposite side of the body.
- This happens because the motor fibers of the corticospinal tract, which take origin from the motor cortex in the brain, cross to the opposite side in the lower part of the medulla oblongata and then descend down in the spinal cord to supply their respective muscles.
Causes:
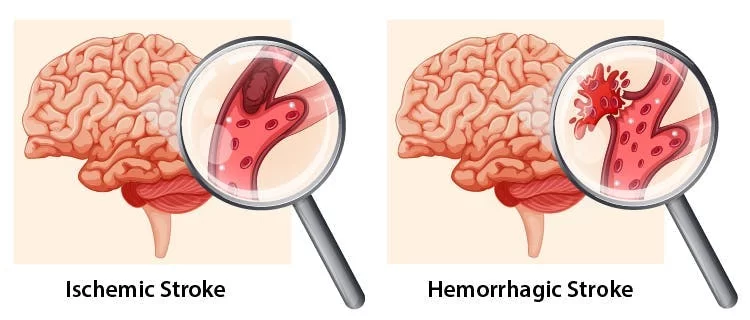
- Vascular – Cerebral hemorrhage, Stroke, Diabetic Neuropathy.
- Infective – Encephalitis, Meningitis, Brain abscess.
- Neoplastic – Glioma – meningioma
- Demyelination – Disseminated sclerosis, lesions to the Internal capsule.
- Traumatic – Cerebral lacerations, Subdural Hematoma. The rare cause of hemiplegia is due to local anesthesia injections given intra arterially rapidly, instead of given in a nerve branch.
- Congenital- Cerebral palsy
- Disseminated – Multiple Sclerosis
- Psychological – Parasomnia (Nocturnal hemiplegia )
Symptoms :
- Holding one hand in a fist.
- Balance and walking difficulties.
- Issues with fine motor skills and daily living tasks.
- Developmental milestone delays.
- Favoring one hand over the over.
- Muscle stiffness on one side of the body.
- Weakness on one side of the body.
- Problems with limbs positioning properly while walking.
Causes :
- Spastic hemiplegia occurs either at birth or in the womb. The cause can be all types of strokes, cerebral palsy head injuries, hereditary diseases, brain injuries, and infections.
- Malformations of the veins or arteries in any part of the body can lead to
- spastic hemiplegia.
Hemiplegia causes death :
Brain and Nervous System Infections :
- Infections, particularly encephalitis, and meningitis. Some serious infections, particularly sepsis, and abscesses in the neck, may spread to the brain if left untreated.
- This can not only cause hemiplegia, but it can also affect a person’s ability to think and even cause death.
DIFFERENTIAL DIAGNOSIS
Difference between hemiplegia and hemiparesis :
- Hemiparesis is a slight weakness — such as mild loss of strength — in a leg, arm, or face.
- It can also be paralysis on one side of the body.
- Hemiplegia is a severe or complete loss of strength or paralysis on one side of the body.
- Spastic hemiplegia means that movement on one side of the body is affected.
- spastic hemiparesis means that one-half of the body is afflicted with weakness, but is not paralyzed.
Difference between hemiplegia and stroke :
- The term “plegia” is from a Greek word that originally denoted a stroke. In modern medicine, the word is mostly used to refer to paralysis.
- Therefore, hemiplegia means paralysis in one half of the body, usually as a result of a stroke.
Hemiplegia affects the brain :
- Hemiplegia is caused by damage to some part of the brain that disrupts the connection between the brain and the muscles on the affected side.
- Damage to the right side of the brain affects the left side of the body, and damage to the left side of the brain affects the right side of the body.
Hemiplegia a form of cerebral palsy :

- Hemiplegia in infants and children is a type of Cerebral Palsy that results from damage to the part (hemisphere) of the brain that controls muscle movements.
- This damage may occur before, during, or shortly after birth. The term hemiplegia means that the paralysis is on one vertical half of the body.
Left hemiplegia :
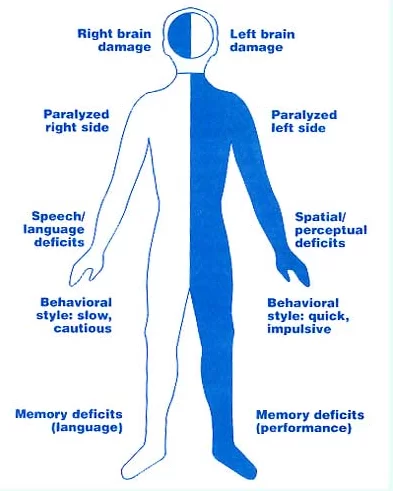
- Left hemiplegia is the paralysis of limbs on the left side of the body, while right hemiplegia indicates paralysis on the right side of the body.
- Like hemiparesis, right or left hemiplegia may be caused by damage to the nervous system.
- One common cause of left or right hemiplegia is an incomplete spinal cord injury.
History and examination :
- An accurate history profiling the timing of neurological events is obtained from the patient or from family members in the case of the unconscious or non-communicative patient.
- The most common, slowest in hours, wakes up in the morning with weakness, a history of TIA, and old age is typical with thrombosis.
- History of heart disease, younger age group, no progression.
- A history of prolonged hypertension, altered consciousness, convulsions, and vomiting is suggestive of hemorrhage.
- The patient’s past history, including episodes of TIAs or head trauma, presence of major or minor risk factors and medications, pertinent family history, and recent alterations in patient function is thoroughly investigated.
Physiotherapy examination :
- The patient includes an investigation of vital signs ( heart rate, respiratory rate, blood pressure, clubbing ), signs of cardiac decompensation, and function of the cerebral hemispheres, cerebellum, cranial nerves, eyes, and sensorimotor system.
General examination :
General appearance including posture, motor activity
Vital signs :
- Level of consciousness, pulse, BP, look for pupil size, conjugate deviations of eyes, Meningeal signs.
Neurocutaneous markers-
- Neurofibroma over the skin ( may have associated Tuberous sclerosis of the brain )
- Sebaceous adenoma
- Sturge Weber Syndrome – facial nerve (port wine stain ) involving one half of the face with upper eyelid – associated with atrophy and calcification of the ipsilateral cerebral hemisphere.
- Lymphadenopathy
- Cyanosis
- Clubbing
- Shortening of hemiplegic limb – indicates it is dating from early childhood
- Irregular pulse of atrial fibrillation
Higher examination :
- A. Consciousness – Check the level of altered sensorium. for this refer to Glasgow Coma Scale B. Orientation -In time, place, space, and person are tested.
- B. Orientation -In time, place, space, and person are tested.
- C. Memory-It includes Immediate memory, Recent memory, and Remote memory. Check with relatives or friends of the patient if he is correct
- D. Intelligence
- E. Speech- Speech disturbances APHASIA may occur
- F. Emotion – Anxious / depressed/elated / swings of mood.
- G. Judgment
- H. Behaviour
- I. Presence of hallucination/dellusion/illusion
Gait :
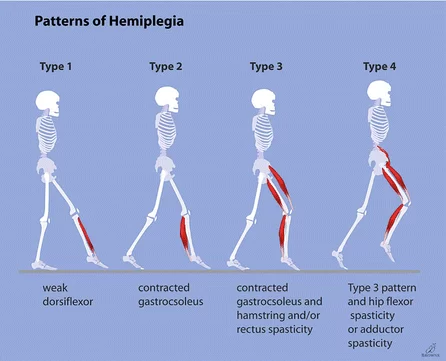
- In hemiplegic patients in whom all the paralysis is on the same side of the body, the lesion is of the contralateral upper motor neuron.
- In the alternating or crossed hemiplegias, CN paralysis is ipsilateral to the lesion, and body paralysis is contralateral.
- Therefore, paralysis of CN III on the right side and body paralysis on the left (Weber Syndrome) indicates a midbrain lesion,
- whereas a lesion of CN VII with crossed hemiplegia (Millard-Gubler Syndrome) indicates a pontine lesion, and CN XII paralysis with crossed hemiplegia (Jackson Syndrome) indicates a lower medullary lesion.
Cranial nerve integrity :

- The therapist examines for facial sensation (CN 5), facial movements (CN 5 and 7), and labyrinthine/auditory function (CN 8 ).
- The presence of swallowing and drooling necessitates an examination of the motor nuclei of the lower brainstem cranial nerves (CN 9, 10, and 12) affecting the muscles of the face, tongue, pharynx, and larynx. The visual system should be carefully investigated, including tests for visual field defects (CN 2, optic radiation, visual cortex ), acuity (CN 2 ), Pupillary reflexes (CN 2 and 3 ), and extraocular movements (CN 3, 4, and 6).
- investigated, including tests for visual field defects (CN 2, optic radiation, visual cortex ), acuity (CN 2 ), Pupillary reflexes (CN 2 and 3 ), and extraocular movements (CN 3, 4, and 6).
Cranial nerve Syndrome associated with hemiplegia :
Syndrome Site Tract Signs Usual cause
- 1.Weber’s Base of midbrain CorticospinalTract +3rd Nerve nucleus Ipsilateral 3rd nerve palsy + contralateral hemiplegia
Vascular, tumor
- Benedikt’s Midbrain CorticospinalTract , 3rd Nerve nucleus + Red nucleus Ipsilateral 3rd nerve palsy +contralateral hemiplegia + Tremors+ ataxia Vascular,tumor
- 3.Millard gubllar’s Pons CorticospinalTract + 6th and 7th Nerve nucleus Ipsilateral LMN 6th and 7th nerve palsy +
contralateral hemiplegia Vascular,tumor
- Medial medullary Syndrome Medial medulla CorticospinalTract + 12th Nerve nucleus Ipsilateral tongue paralysis +contralateral hemiplegia Vascular
Flexibility and joint integrity :
- An examination of joint flexibility should include passive ROM using a goniometer, joint hypermobility/hypomobility, and soft tissue changes (swelling, inflammation, or restriction).
- The shoulder and wrist should be examined closely because joint malalignment problems are common.
- Active ROM may be limited or impossible for the patient in early or middle recovery in the presence of paresis, spasticity, or obligatory synergies that can preclude isolated voluntary movements.
- Contractures can develop anywhere but are particularly apparent in the paretic limbs.
- In the UE, limitations in the shoulder motion of flexion, abduction, and external rotation are common.
- Contractures are likely in the elbow and finger flexors, and forearm pronators. In the LE, plantarflexion contractures are common.
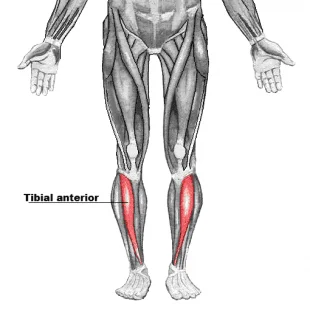
Tone :
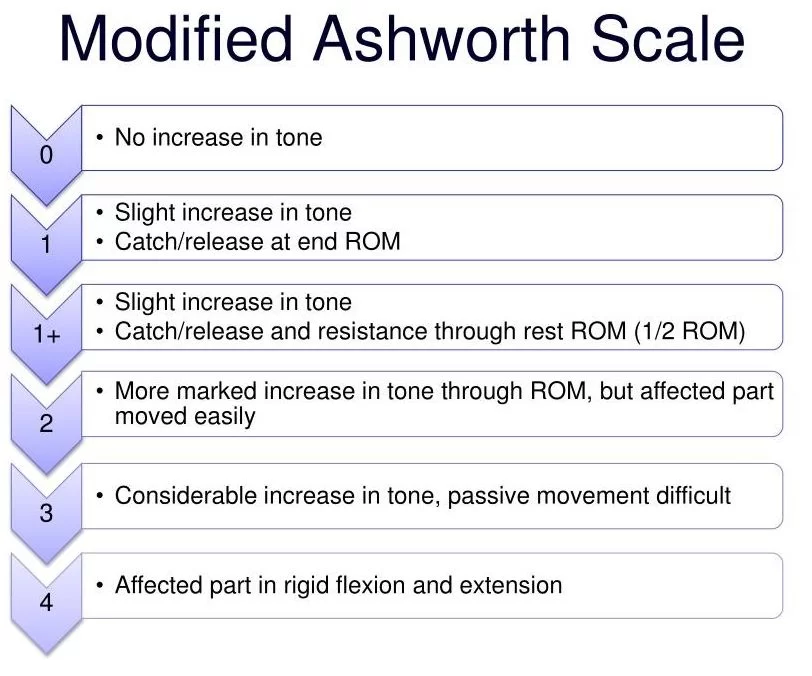
- An examination of tone is essential. Passive motion testing can be done to determine the presence of hypertonicity or spasticity.
- The severity of spasticity can be graded on the basis of resistance to passive stretch using the Modified Ashworth Scale.
Reflexes :
- Reflexes are altered and also vary according to the stage of recovery.
- When spasticity and synergy emerge, hyperreflexia is seen.
- Deep tendon reflexes are hyperactive and a patient may demonstrate clonus, clasp-knife response, and positive Babinski, all consistent findings of upper motor neuron Syndrome.
- In the upper limb clinically significant – if markedly active and asymmetrical are Hoffmann’s sign, and Wartenberg’s sign.
- Superficial reflexes in hemiplegia are loss of Abdominal reflex and cremasteric reflex which is a sign of UMN Lesion.
Voluntary movements :
- Thus the patient is unable to perform isolated movements of a single limb segment without producing movements in the remainder of the limb.
Two distinct abnormal synergy patterns have been described for each extremity: flexion and extension synergy.
- Flexion Synergy Components Extension Synergy Components
- Upper extremity Scapular retraction/elevation or hyperextension
- Shoulder abduction, external rotation
- Elbow flexion*
- Forearm supination
- Wrist and finger flexion
- Scapular protraction
- Shoulder adduction, internal rotation
- Elbow extension
- Forearm pronation
- Wrist and finger flexion
- Lower extremity Hip flexion,* abduction, external rotation
- Knee flexion
- Ankle dorsiflexion, inversion
- Toe dorsiflexion
- Hip extension, adduction,* internal rotation
- Knee extension*
- Ankle plantarflexion,* inversion
- Toe plantarflexion
TREATMENT :
General :
- In the acute (shock ) stage of hemiplegia and in the comatose patient.
- Treatment of the adult with Hemiplegia, following stroke starts from the very acute stage, when the patient is in the ICU or Hospital bed.
- Treatment should be based on an assessment by the relevant health professionals, including physiotherapists, Physicians, and occupational therapists.
- Muscles with severe motor impairment including weakness need these therapists to assist them with specific exercises.
Aims :
- 1) Prevent recurrent stroke
- 2) Monitor vital signs, dysphasia adequate nutrition, bladder & bowel function.
- 3) Prevent complications
- 4) Mobilize the patient
- 5) Encourage the resumption of self-care activities
- 6) Provide emotional support & education for patient & family
Spastic Hemiplegia Treatment
- Physiotherapy Treatment and Occupational Therapy.
- Medications.
- Sensory integration.
- Strength training.
- Surgery.
- Nutritional guidance.
- Oxygen therapy.
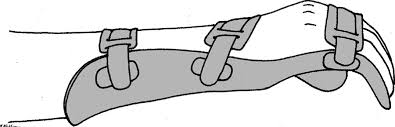
- Splinting and casting.
Weight-bearing help Reduce spasticity:
- Any weight bearing of the upper extremity either at the wall, table, or floor helps sends signals to the brain that reminds it the arm is still there.
- Strengthening can improve spasticity in two ways. Strengthening the antagonist (opposing) muscle, it can help inhibit the reaction of the spastic muscle.
Icing reduces spasticity :

- Efferent and afferent neurotransmission is reduced through prolonged use of ice,
- which is effective for the reduction of spasticity. In order to achieve this, the muscle spindles need to be cooled requiring that ice is applied until there is no longer an excessive reflex response to stretching.
Heat decrease spasticity :
- Sometimes heat or ice can be used to temporarily relax a spastic muscle.
- Warm baths or swimming pools can also help to relax a spastic muscles.
- Care of the skinICE
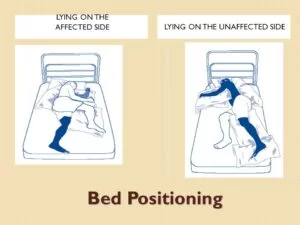
- Frequent changes of the patient’s position (every 2 hours) and of the bed sheets.
- Frequent wash of the skin of the back and pressure points with alcohol followed by talc powder.
2. Care of respiration
- Suction of nasal and pharyngeal secretions.
- Oxygen inhalation via catheter or mask especially in cases of coma.
- Tracheostomy in urgent cases.
- Breathing exercise
- Chest expansion exercise
- Huffing and coughing technique
- Postural drainage
3. Care of nutrition and fluid balance
- Tube feeding gives fruit juices, milk, and pureed food, besides I.V. Fluids, in comatosed patients.
4. Care of urinary bladder
- Foley’s self retaining catheter in case of retention or incontinence.
- Urinary antiseptics : Gentamycin 80 mg I.M . every 12 hours.
- Care of bowels : Daily enema.
5. Prevent from deconditioning
- Early mobilization in the bed (active turning, supine to sit, sit to supine, sitting, sit to stand)
- Pelvic bridging exercise
- Early propped up positioning, sitting & then later to standing
- Moving around the bed
- Facilitate movement of functioning limbs
Rehabilitation :
- Repetitive practice of functional tasks with the affected arm to stimulate motor pathways and improve upper limb function.
- Active and passive range of movement exercises to strengthen muscles in the arms leg and trunk and relieve pain and stiffness.
- Stroke rehabilitation begins almost immediately, preferably within 24-36 hours once a patient is found medically stable.
- The Physiotherapist focuses on joint range of motion and strength by performing exercises and re-learning functional tasks such as bed mobility, transferring, walking, and other gross motor functions.
- Physiotherapists can also work with patients to improve awareness and use of the hemiplegic side.
Physiotherapy Treatment protocol :
a. Conventional therapies (Therapeutic Exercises, Traditional Functional Retraining)
- Range Of Motion (ROM) Exercises
- Muscle Strengthening Exercises
- Mobilization activities
- Fitness training
- Compensatory Techniques
STRETCHING EXERCISE FOR SPASTIC HEMIPLEGIA :
b. Neurophysiological Approaches:
- Muscle Re-education Approach.
- Neurodevelopmental Approaches: Neurology Treatment Techniques
- Sensorimotor Approach (Roods)
- Movement Therapy Approach (Brunnstrom)
- NDT Approach (Bobath)
- PNF Approach (Knot and Voss)
Hese basic level exercises are a starting point to add flexibility and mobility to your affected arm after hemiplegia :

- Exercise #1 Inner Arm Stretch.
- Exercise #2 Wrist and Hand Stretch.
- Exercise #3 Elbow Stretch.
- Exercise #4 Crawling Stretch.
- Exercise #5 Wrist Motion.
- Exercise #6 Elbow Weight Training.
- Exercise #7 Finger Walk.
PROGRAM :
Duration :
- The overall duration of the session will be one hour. The total duration of the aerobic/cardiac exercise training should increase from 15 minutes (week one) to 40 minutes by week 12.
Intensity
The intensity of exercise should aim to be moderate as opposed to low. This effort level is required for all components but will be adjusted for each individual according to health status on a session-by-session basis.
Frequency
- The frequency of the session should be three times per week wherever possible.
Functional electrical stimulation (FES):
- FES is a modality that applied a short burst of electrical current to the hemiplegic muscle or nerve.
- In Hemiplegia Physical Therapy, FES has been demonstrated to be beneficial to restore motor control, spasticity, and reduction of hemiplegic shoulder pain and subluxation.
- It is concluded that FES can enhance the upper extremity motor recovery of acute stroke patient.
- FES could reduce spasticity in stroke patients. A recent meta-analysis of a randomized controlled trial study showed that FES improves motor strength.
- FES can significantly improve arm function, electromyographic activity of the posterior deltoid, range of motion, and reduction of severity of subluxation and pain of the hemiplegic shoulder.

Biofeedback:
Conventional gait training has focused on part-practice of components of gait in preparation for walking.
It includes
- Biofeedback is a modality that facilitates the cognizance of electromyographic activity in selected muscles or awareness of joint position sense via visual or auditory cues.
- In Hemiplegia Physical Therapy the result of studies in biofeedback is controversial.
- A meta-analysis of 8 randomized controlled trials of biofeedback therapy demonstrated that electromyographic biofeedback could improve motor function in hemiplegic patients.
- Another meta-analysis study on EMG has shown that EMG biofeedback is superior to conventional therapy alone for improving ankle dorsiflexion muscle strength and showed that biofeedback could improve earlier postural control to improve impaired sitting balance.

Conventional gait training:
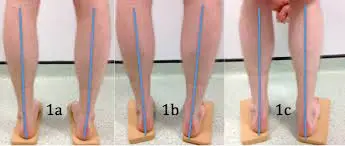
- Symetrical Weight bearing training
- Weight shifting
- Stepping training (swinging / clearance )
- Heel strike
- Single leg standing
- Push off / Calf rise.



Useful info, Spastic Hemiplegia is a very difficult to manage, required too much patience , stretching exercise is the best option.