Cervical Injury
Table of Contents
What is Cervical Injury?
Cervical injury refers to damage to the cervical spine, which is part of the spine that includes the seven vertebrae in the neck. The cervical spine is responsible for supporting the head, protecting the spinal cord, and allowing for movement of the head and neck. Cervical injuries can be caused by a variety of traumatic events, such as falls, car accidents, or sports injuries, and can range from mild to severe.
- Cervical spine injuries, although uncommon, can lead to significant and long-term disability.
- The cervical spine encompasses seven vertebrae and provides protection for the spinal cord.
- The division of the spine very susceptible to damage is the cervical spine based on its anatomy and flexibility.
- This activity analysis the etiology, evaluation, presentation, and management of many cervical spine injuries and reviews the part of the interprofessional team in evaluating, diagnosing, and managing the condition.
Objectives:
- The multiple types of cervical spine injuries and the pathophysiology attending each type.
- Summarize the relevant way of achieving an examination and assessment of cervical spine injuries, involving any indicated diagnostic imaging.
- Describe the many more treatment modalities based on etiology for cervical spine injuries.
- Describe collaborative team strategies for enhancing communication and care coordination with cervical spine injuries caused by a variety of etiological factors.
- The mechanism of damage is important in associating the type of injury for which the case is at-risk.
- Trauma is the very common cause of cervical injury, and this can involve motor vehicle accidents, falls, penetrating or blunt trauma, and sports-related or diving injuries.
- Nontraumatic causes can involve compression fractures from osteoporosis, arthritis, and inflammation of the spinal cord.
- Cervical injury so more common in males than females, with the highest prevalence in ages 14 to 35 and older than 60 years.
- The very common mechanisms in children younger than 14 years are motor vehicle accidents, falls, and sports-related injuries.
- The very common areas of damage are in the regions of C2, C5, C6, and C7.
Levels of Injury
Vertebrae are grouped into sections. The higher the injury on the spinal cord, the further dysfunction can do.
High-Cervical Nerves (C1 – C4)
- Most severe the spinal cord injury levels
- Paralysis in arms, hands, trunk, and legs
- The patient might not be good to breathe on their own, cough, or control bowel or bladder movements.
- The ability to speak is sometimes reduced.
- When four limbs are affected, this is called tetraplegia (quadriplegia).
- Requires complete assistance with activities of day-to-day living, like eating, dressing, bathing, and getting in or out of bed
- May be good to use powered wheelchairs with special controls to move around on their own
- Will not be good to drive a car on their own
- Requires 24-hour-a-day personal care
Low-Cervical Nerves (C5 – C8)
- Corresponding nerves control arms and hands.
- A person with this position of injury might be good to breathe on their own and speak normally.
C5 injury
- The person can lift their arms and bend elbows.
- Likely to have some paralysis of wrists, hands, trunk, and legs
- Can speak and apply the diaphragm, but breathing will be increased
- Will need assistance with most activities of day-to-day living, but once in a power wheelchair, can move from one place to another independently
C6 injury
- Nerves affect wrist extension.
- Paralysis in hands, trunk, and legs, typically
- Should be good to bend your wrists back
- Can speak and apply the diaphragm, but breathing will be increased
- Can transfer in and out of wheelchair and bed with beneficial equipment
- May also be good to drive an adapted vehicle
- Little voluntary control of the bowel or bladder, but might be good to manage on their own with unique equipment
C7 injury
- Nerves control elbow extension and further finger extension.
- Most can straighten their arm and have routine movement of their shoulders.
- Can do most activities of day-to-day living by themselves, but might need assistance with further difficult tasks
- May also be good to drive an adapted vehicle
- Little voluntary control of the bowel or bladder, but might be good to manage on their own with unique equipment
C8 injury
- Nerves control some hand movement.
- Should be good to grasp and release objects
- Can do most activities of day-to-day living by themselves, but might need assistance with further difficult tasks
- May also be good to drive an adapted vehicle
- Little voluntary control of the bowel or bladder, but might be good to manage on their own with unique equipment
Thoracic Nerves (T1 – T5)
- Corresponding nerves affect muscles, mid-back, upper chest, and abdominal muscles
- Arm and hand functions are commonly normal
- Cervical Injuries commonly affect the trunk and legs(also known as paraplegia)
- Most likely use a manual wheelchair
- Can learn to drive a modified car
- Can stand in a standing frame, while others might walk with braces
Thoracic Nerves (T6 – T12)
- Nerves affect the muscles of the trunk depending on the level of injury
- Normally results in paraplegia
- Normal upper-body movement
- Fair to good capability to control and balance trunk while in the seated position
- Should be good to cough productively (if abdominal muscles are intact)
- Little voluntary control of bowel or bladder, but might be good to manage on his/her own with unique equipment
- Most likely use a manual wheelchair
- Can learn to drive a modified car
- Further can stand in a standing frame, while others might walk with braces
Lumbar Nerves (L1 – L5)
- Injuries generally result in further loss of function in the hips and legs
- Little voluntary control of the bowel or bladder, but might be good to manage on their own with unique equipment
- Depending on strength in the legs, might need a wheelchair and might also walk with braces
Sacral Nerves (S1 – S5)
- Injuries generally result in further loss of function in the hips and legs
- Little voluntary control of bowel or bladder, but may be good to manage on their own with unique equipment
- Most likely will be good to walk
Common injuries of cervical injury
- Cervical Spinal Cord Injury
- Sports-related Neck Injury
Cervical Spinal Cord Injury
What Is a Cervical Spinal Cord Injury?
- The cervical division of the spine involves the top division of the spinal cord, including seven vertebrae (C-1 to C-7) in the neck.
- Being closer to the brain and affecting a larger portion of the body, cervical spinal cord injuries are generally a very severe cause of paralysis. However, it’ll result in tetraplegia, meaning there’s limited or absent feeling or movement below the shoulders or neck, If there’s an injury in the cervical area.
General Effects of Cervical Spinal Cord Injuries
- Cervical spinal cord injuries oft involve permanent complete or incomplete loss of sensory function and many more associated complications. As is the case with all injuries of the spinal cord, injuries located higher on the spine will be further severe, with high cervical spinal cord injury being fatal.
Types and Levels of Spinal Cord Injuries
- The spinal cord is allowed to transfer messages between the rest of the body and the brain. When one experiences a spinal cord injury, the body might lose many necessary functions if the nerves can’t transfer to the brain. Since there are multiple types of spinal cord injuries, it’s best to accept how they differ and what symptoms are associated with each level.
Types of Spinal Cord Injury
- Since most spinal cord injuries are trauma-based, there are different ways and types of spinal cord injuries occur. A further the most common causes of spinal cord injury include anyone vehicle accidents, falls, gunshot wounds, sports injuries, or surgical difficulties. Very cases can be divided into two types of spinal cord injury complete spinal cord injury vs. incomplete spinal cord injury:
- A complete spinal cord injury causes permanent injury to the area of the spinal cord that is affected. Paraplegia or tetraplegia is the outcome of total spinal cord injuries.
- An incomplete spinal cord injury refers to a partial injury to the spinal cord. The capability to move and the amount of feeling based on the area of the spine injured and the severity of the injury. Results are based on a patient’s health and medical history.
Levels of Spinal Cord Injury
- Four divisions of the spinal cord impact the level of spinal cord injury: cervical, thoracic, lumbar, and sacral. Each spine portion preserves individual groups of nerves that control the body. The types and severity of spinal cord injuries can be based on the portions of the spine that are damaged. Learn about the divisions of the spine, the four levels of spinal cord injury, and possible recovery results.
Spinal Cord Injury Diagnosis
- To determine the severity of a spinal cord injury, doctors achieve a series of diagnostic tests, involving checking the patient’s strength and sensation in their arms and legs. Utilizing complete imaging assessment tools, doctors screen the body to identify spine fractures. Learn others about the tools used during a spinal cord injury conclusion test.
Cervical Spinal Cord Injury Recovery and Prognosis
- Spinal cord injury prognosis varies depending on the inflexibility of the injury. After reducing swelling in the spinal cord and further needed surgery is completed, patients can stable and initiate the recovery process.
- Recovery will focus on the stabilization of the injured area of the spinal cord, but most injuries are permanent.
- Steroid and anti-inflammatory medicine administered shortly after injury, like methylprednisolone, can help in reducing swelling, which is a very common cause of secondary damage at the time of injury.
- Rehabilitation will focus on learning to use the non-paralyzed division of the body to recover different levels of autonomy.
- Cervical spinal cord injury patients will need continuous, care for the rest of their lives.
Sports-related Neck Injury
- Playing sports can give neck injuries of individual phases of severity ranging from relatively minor injuries like muscle strains to severe life-threatening conditions like neck fractures and cervical spinal cord injuries.
- A neck fracture can occasionally direct to a complete spinal cord injury, which will result in further degrees of paralysis or even death.
Cervical injuries from participation in sports can be divided into the following clinical syndromes:
- Cervical fractures and dislocations
- Nerve root or brachial plexus injuries
- Intervertebral disc lesions
- Cervical stenosis
- Acute cervical sprains/strains including whiplash injury
- Transient quadriplegia
Signs and Symptoms
- Localized neck pain, which might or might not be severe
- Neck stiffness
- Pain radiating from the neck down to the shoulders and arms
- Swelling and bruising
- Tenderness
- Decrease in sensation in the arms, legs, and body
- Muscle weakness or paralysis of the legs and/or arms
- Difficulty breathing
Spinal Concussions
- A spinal concussion can do which might also be complete or incomplete. In such cases, the spinal cord dysfunction is transient, normally decide within one or two days. Football players are unusually open to spinal concussions and spinal cord contusions. The latter might produce neurological symptoms like numbness, tingling, electric shock-like sensations, and burning in the extremities.
Signs and Symptoms:
- Extreme pain in the neck, head, and back
- Tingling or loss of sensation in the hand, fingers, feet, and toes
- Partial or complete loss of control over any portion of the body
- Urinary or bowel urgency, incontinence, and retention
- Difficulty with balance and walking
- Abnormal band-like sensations in the abdomen: pain, pressure
- Impaired breathing after injury
- Unusual lumps on the head and spine
Sports-related Spinal Cord Injury by age at the time of injury
- Ages 0-15: 24.1%
- Ages 16-30: 14.2%
- Ages 31-45: 7.3%
- Ages 46-60: 4.5%
- Ages 61-75: 2.8%
- Ages 76-98: 0.9%
Testing and Diagnosis
- Any sports-related neck injury must be managed with a high degree of suspicion for acute conditions, like neck fractures. A spinal cord injury(SCI) or neck fracture is a medical emergency. An athlete should not return to the sport or activity through medically cleared and their strength has returned to pre-injury levels. The patient should experience a total neurological test as immediately as possible to assess for instability and a spinal cord injury.
A specialized physician’s diagnosis based on a physical examination, symptoms, and results of radiological tests, involves one or more of the following:
- Computed tomography scan (CT or CAT scan): A diagnostic picture created after a computer reads X-rays; can show the size and shape of the spinal canal, its contents, and the structures around it.
- Magnetic resonance imaging (MRI): A individual test that produces three-dimensional images of body structures using powerful magnets and computer technology; can show the nerve roots, spinal cord, and surrounding areas, as well as tumors, degeneration, and enlargement.
- X-ray: The application of radiation to produce a film or image of a part of the body can show the structure and alignment of the vertebrae and the outline of the joints.
Treatment
The treatment options are based on the following factors:
- The severity of the fracture
- If there is an associated instability or dislocation
- Which cervical bones are fractured
- Whether there is spinal cord injury, muscle weakness, or paralysis
A compression fracture is oft treated with a cervical collar or brace worn for 4 to 7 weeks through the bone heals on its own. When treating an acute or complex fracture, surgery or traction may be required, including spinal instrumentation or fusion with or without surgical decompression.
Prevention Tips
Bicycling
- While many cycling injuries are head injuries, the proper usage of SNELL, approved helmets can also help prevent Spinal Cord Injury.
- The helmet must fit properly, and the helmet strap is tightened and closed so that it does not come off while riding or in a fall.
Other Spinal Cord Injury cycling prevention tips include:
- Keep children less than 1 to 2 years old off the bicycle.
- Cycle a minimum of 2 to 3 feet away from parked cars.
- Do not wear headphones.
- Local traffic regulations at all times.
- Never hold on to a moving vehicle.
- Use “hand signs” to propose the direction of turns.
Football
- Football players collect acceptable preconditioning and strengthening of the head and neck muscles.
- Trainers and officials discourage players from operating the top of her/his football helmets as assaulting force when blocking, hitting, attacking, and ball carrying.
- Trainers, physicians, and coaches ensure players’ equipment is properly fitted, mainly the helmet, and that straps are in the lock position.
- Trainers prepared for a possible catastrophic spinal cord injury. All staff must know what to do in such a case. Being set and well-informed might make all the difference in preventing permanent disability.
- Enforcement of rules enjoining spearing in practice and games.
- Ball carriers are instructed to not lower their heads when making attachments with the tackler to avoid helmet-to-helmet collisions.
Skateboarding and In-line Skating
- Inspect the skateboard or skates for any damaged parts.
- Always wear a helmet, attached securely to the head.
- Check the area for rocks, debris, cracks in the pavement, or irregular surfaces.
- Wear well-fitted clothing, knee and elbow pads, wrist braces, and gloves.
Swimming/Diving
- Do not dive in water less than 10 to 12 feet deep or in aboveground pools. Confirm the depth and check for debris in the water before diving.
- Follow all rules and warning signs at water premises, swimming pools, and public beaches.
- The first time in a body of water, walking to the water.
- Noway push or shove anyone into the water and do not allow children to do so.
General Sports
- Supervise younger children at all times, and do not allow the use of sporting equipment or play sports infelicitous for their age. Do not allow the use of playgrounds with tough surface grounds.
- Do not participate in sports when ill or actually tired.
- Reject and replace damaged sporting equipment or protective gear.
- Noway slides headfirst when stealing a base.
Common Neck Injuries
- When your neck is sore whether it’s from a poor night’s sleep or a sudden injury.
- Moving your head when vehicle driving, lifting objects, or totally playing a favorite sport can get painful and uncomfortable.
Types and Causes of Common Neck Injuries
The most common neck injuries include:
- Neck sprain or strain:– A sprain can be when ligaments in the neck are torn. A strain mentioned to a torn tendon or muscle. This can do as a result of sudden damage during physical activity or even a minor car accident.
- Stiff muscles and tendons:– Normally called a spasm in the neck, stiffness can be caused by activity awkwardly or keeping the neck in the same position for a long period of time like sleeping overnight.
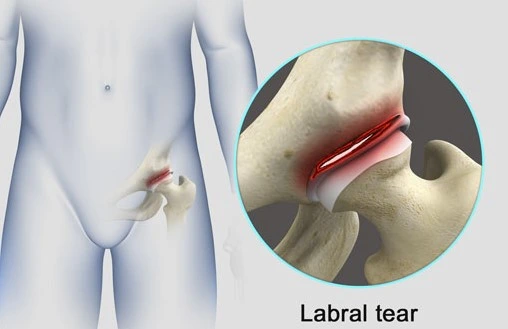
- Herniated disc:– A herniated disc occurs when a spinal disc becomes torn and the soft jellylike inside leaks or bulges out of the disc. Generally a result of wear and tear, herniated discs can also be caused by a sudden injury, involving a fall.
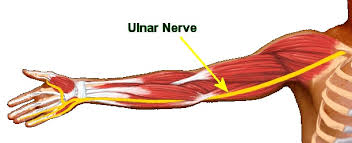
- Pinched nerve:– Due to cervical injury, Bone, tissue, or tendons can compress nerves, which causes referred pain in arms. This can happen as a result of a cervical muscle sprain or cervical strain.
- Fractured cervical spine:– However rare, a broken(fractured) cervical spine is a most serious condition that requires immediate medical attention.
Common neck injury symptoms
Your symptoms will depend on the type and severity of your injury, but the very common symptoms include:
- Difficulty turning the neck
- Headaches
- Muscle spasms in the neck and shoulders
- Neck pain
- Stiffness in the neck
- Weakness in the legs, arms, hands, or fingers
Common neck injury treatment
Your treatment will be depending on the cause of your neck injury. Treatment might involve:
- Physical therapy:- A physical therapist will teach you exercises to reduce pain, improve flexibility and strengthen muscles in the neck.
- Medicine:– Over-the-counter and prescription medications can help relieve pain, reduce inflammation, and support you find comfort.
- Injections:– Corticosteroid injections, middle branch blocks, and other injections can support reducing inflammation and support relieve pain caused by several different injuries to the neck.
- Acupuncture:– Thin needles are fitted into specific spots along the spine to trigger the release of certain chemicals into the body, helping reduce pain. Acupuncture, applied with traditional treatment, like pain management or physical therapy can support.
- Massage:- Medical massage therapy can support reducing inflammation, ease pain, and provide relief from certain back conditions. Your doctor might recommend massage therapy along with other treatments.
- Anti-inflammatory Diet:– A diet that supports boost your body’s natural ability to fight inflammation might support reduced symptoms when combined with other treatment plans.
Our team will work nearly with you to manage your pain before recommending surgery. If you continue to experience pain and cervical spine surgery, loss of motion might be recommended. These involve:
- Mazor X:- A robotic-guided spine surgery, Mazor X uses 3D imaging to allow your surgeon to customize the surgery to your individual anatomy and needs. This leads to better results and faster recovery.
- Cervical discectomy and fusion:- A injured cervical disc can be removed and replaced with an artificial disc. You might also need fusion surgery, which helps fuse two or further discs with hardware to stabilize and support the cervical spine (neck).
- Laminectomy:– A laminectomy removes part or all of the back of vertebrae and thickened tissue around the vertebrae to allow further room for the spinal cord. This helps relieve force on the affected nerve.
Common neck injury risk factors
Common risk factors contribute to a neck injury. These involve:
- Genetics:- A family record of neck pain or neck arthritis
- Tobacco usage:- If you are a smoker
- Repetitive neck movement:– If you have a position that needs repetitive neck movement or overhead work
- Trauma or injury to the neck:- Either through an accident, sports or indeed sleeping wrong
Common neck injury prevention
It might be not possible to completely prevent an injury to the neck, but you can take ways to reduce your risk and preserve your spine health:
- Maintain a healthy weight
- Exercise regularly
- Strengthen back and core muscles
- Eat healthily
- Look for ergonomic pillows, chairpersons, and other materials to help correctly position your spine
- Use good posture when standing and sitting
- Use caution when lifting, twisting, and turning
Medical Management
- General Management
- Medical Management
General Management
Immediate Management Goal
- Resuscitation according to ATLS guidelines
- Determination of neurological injury
- Prevention of Neurological Deterioration
- Prevention of complications
- Ongoing ID & Tx of assoc injuries
- Initiation of definitive management for vertebral column injury or spinal cord injury
The aim is to prevent the extension of primary injury reduce secondary injury and treat complications.
Follow ATLS principles:
- Airway; protect the spine
- Breathing
- Circulation
- Disability, Dx, and Rx Shok
- Expose patient
- Treat secondary survey
Medical Management
- Medical treatment of spinal disorders has improved significantly over the years of the many conservative non-surgical treatments that are currently available, a few of the most commonly practiced treatments are;
- Epidural steroid injection
- Intradiscal thermoplastic(IDET)
- Nucleoplasty
- Facet injections, and Medical branch blockade
- Radiofrequency Rhizotomy or Denervation
Surgical Management
- Depending on the conditions, when surgery is required.
- Surgery might be considered if the spinal cord is compressed and when the spine requires stabilization.
- The surgeon resolves the procedure that will provide the greatest benefit for the patient.
The common procedures which we perform are:
- Surgical decompression
- Surgical stabilization:- Spinal fusion, Fixation of the vertebra, and Fixation of the spine
- Discectomy, foraminotomy and laminectomy(sometimes needed)
- Artificial disc implantation
Surgical decompression and fusion
- Decompression of the neural spinal cord or nerves
- Stabilization of the bony spine
Emergent
- Incomplete lesions with progressive
- Neurologic deficit
Elective
- Complete lesions(3-7 days post-injury)
- Central cord syndrome(2-3 weeks post-injury)
Physiotherapy Treatment
- The acute care and rehabilitation of the spinal cord injury depend on the level and type of injury to the spinal cord. Individuals with a spinal cord injury generally demand initial treatment in an acute care unit. The rehabilitation process normally starts in the acute care setting, followed by extended treatment in a specialized Spinal Injury Unit. Inpatient care can last from 8 – 24 weeks, with follow-up inpatient rehabilitation from 4 – 12 months, usually followed by yearly medical and functional reviews.
- The management of an individual with spinal cord injury is complex and lifelong taking a multidisciplinary approach. A functional, goal-oriented, interdisciplinary, rehabilitation program should allow the individual with a spinal cord injury to live as full and self-dependent a life as possible.
- Physiotherapy, occupational therapy, language and speech therapy, rehabilitation nurses, social workers, psychologists, and different health and social care professionals work as a team under the coordination of a Rehabilitation Physician to resolve goals with the individual and develop a plan of discharge that is applicable for the individualities level of injury and circumstances.
Five key ways in the management of individuals with spinal cord injury are;
- Assessing impairments, activity limitations, and participation restrictions
- Setting goals applicable to activity limitations and participation restrictions
- Associating key impairments that are limiting the achievement of goals
- Associating and administering physiotherapy treatments like strengthening, joint mobility, motor skill development, cardiovascular fitness, respiratory functioning, and pain care.
- Measuring the outcome of treatments
The management of things with a Spinal Cord Injury can be divided into 3 Phases;
- Acute,
- Sub-acute (Rehabilitation), and
- Chronic (Long Term)
- During the acute and subacute phases of treatment, rehabilitation strategies concentrate more on the prevention of secondary complications, promoting neuro recovery, addressing supporting impairments, and maximizing function. In the chronic phase, compensatory or assistive ways are oft used.
Acute Phase
- The prevention of complications that occur from spinal unstable or neurological compromise involves all members of the multi-disciplinary team. In this early phase post-injury, physiotherapy care is mostly included in the prevention and management of respiratory and circulatory complications, as well as minimizing the impact of immobilization on the independent e.g. pressure ulcer – and contracture development.
Treatment objectives in the acute phase involve:
- o institute a prophylactic respiratory regimen to manage respiratory conditions and any complications as a result of the spinal cord injury e.g. enhance clearance of secretions, decrease incidence atelectasis
- to achieve a self-sufficient respiratory status where possible
- to maintain the full range of motion of all joints within the limitations determined by the stability of the fracture
- to monitor and manage the neurological status
- to maintain and strengthen all muscle groups
- to facilitate functional patterns of activity
- to help and educate the patient, carers, family, and staff
Respiratory Function
- Common secondary complications involve hypoventilation, atelectasis, secretion retention, and pneumonia.
- The respiratory function is affected due to disruption in the spinal cord applicable to the neurological level of the spinal cord injury.
- Situations of innervations are; C3-5 Diaphragm, C3-8 Scalenes, C5-T1 Pectoralis, T1-11 Intercostalis, and T6-12 Abdominals.
- Individuals with C1-3 tetraplegia require mechanical ventilation, while most individuals with C4 tetraplegia will be good to breathe independently. Although individuals with spinal cord injury C4 to T12 can breathe independently, they might quite have reduced vital capacity and difficulty in increasing intra-abdominal pressure for an effective cough or other forced-expiratory techniques.
- Physiotherapy rehabilitation should always involve secretion clearance and increased ventilatory techniques. Secretion clearance techniques involve percussions, vibrations, shaking, additionally postural drainage and suctioning. Treatment to improve ventilation involves abdominal binders, positioning, deep breathing exercises, incentive spirometry, and inspiratory muscle training. Other medical outfits used to improve ventilation are continuous positive airway pressure and bi-level positive airway pressure.
Range of motion of all joints
- Reduced range of motion might lead to contractures due to immobility and poor positioning, additionally increased tone and spasticity.
- Treatment techniques should involve passive stretches, positioning in the lengthened position, and other common hypertonic treatment techniques like compression, heat, and sustained deep pressure.
Prevention of Pressure Ulcers
- Areas prone to pressure ulcers involve; the occiput, scapulas, sacrum, and heels when lying supine. While the greater trochanter and malleoli are further prone to side-lying.
- Rehabilitation in the acute period includes passive pressure treatment, such as frequent rolling and mobilizing routines, as well as proper skin moisturizing, diet, and monitoring.
- Later, in the sub-acute and long-term phases, individuals will be taught how to achieve frequent self-lift techniques to relieve pressure.
Maintaining and strengthening innervated muscles
- Progressive resistance training and functional strength training are clinically associated to achieve a favorable outcome in maintaining and strengthening innervated muscle groups.
Dosage for strengthening (progressive resistance training):
- one to three sets of 10-12 reps (rest 1-3mins between sets)
- load 60-70% of one-rep max
- 2-3x per week
- In order to target patience; reduce load and increase repetitions
Sub-acute (Rehabilitation) Phase
- The sub-acute phase requirements of individuals with a spinal cord injury are best at a specialized Spinal Cord Injury Unit, but often rehabilitation begins in the Acute or Trauma Hospital while the existent is waiting for transfer to a Spinal Injuries Unit. Rehabilitation requires consideration of the whole person; their physical, mental, vocational, and social background. The rehabilitation process is a goal-directed, and time-limited process aimed at facilitating the most independence and optimal reintegration back into the existent’s chosen community role and lifestyle.
- Following a spinal cord injury, physical therapy is a crucial part of the recovery process. It involves a variety of interventions that address many domains in the International Classification of Functioning, Disability, and Health (ICF) involving body function and structure, activity restriction, and participation, with many interventions directed at helping, rather than treating, impairments, activity restriction, and participation restrictions. The management’s primary goal has changed to Quality of Life, which includes community involvement, gainful employment, interpersonal relationships, and rest conditioning.
Treatment objectives of the rehabilitation phase involve:
- to establish an interdisciplinary process that is patient-focused, comprehensive, and coordinated
- to address physical motor functional activities with early intervention and management to help further complications
- to improve an existent’s independence in activities of day-to-day living, such as bathing, eating, dressing, grooming, and mobility
- to achieve functional independence, whether physical- or verbal outfit in order to facilitate this independence
- to achieve and maintain successful reintegration into the group.
- The range of therapy activities applied by physiotherapists during rehabilitation varies depending on the position and type of injury. For patients with high levels of quadriplegia, range of motion/stretching, strengthening, and transfers were the most common therapeutic activities; for patients with low levels of tetraplegia, transfers used up more time than strengthening. The most common physiotherapy procedures in people with paraplegia were transfers, then range-of-motion exercises, stretching, and strengthening.
- Beings with different cases of spinal cord injury achieve different motor tasks differently and it’s important for physiotherapists to understand which functions are available and applicable to the spinal cord injury level. All motor tasks should be divided into sub-tasks in setup to perform activities optimally. In order to perform motor tasks successfully individuals should have sufficient strength, balance, range of motion, and knowledge or skill regarding the specific motor task. All these phases can be secured through frequent progressive training.
Bed mobility and transfers
C6 and lower-level spinal cord injury have the capability to attain 5 motor skills;
- rolling (using momentum)
- mobilizing from supine to long-sitting
- unsupported sitting (short- & long sitting)
- lifting vertically
- transfers
C6 tetraplegia might have a few challenges, but these 5 motor skills are still possible with a few modifications. With rolling, C6 tetraplegia should swing their arms and externally rotate their shoulders across their body rather than overhead. C6 tetraplegia should lock elbows and externally rotate shoulders in extension while sitting unsupported to keep their balance. With hands placed anterior to the pelvis, C6 tetraplegic individuals can lift objects vertically by passively extending their elbows, lowering their shoulders, and externally rotating their shoulders.
Wheelchair (WC) mobility
- Individuals with C1-4 tetraplegia require a powered-Wheelchair. These wheelchairs might be controlled by chin movements, sip, puff, or head array.
- Individuals with C5 tetraplegia most commonly use a powered-Wheelchair controlled by hand movement.
- Most beings with C6-8 tetraplegia are able to independently mobilize with a manual Wheelchair, but still, may use a hand-controlled Wheelchair as an alternative.
- Individuals with spinal cord injuries lower than C8 will be good to independently mobilize with a Manual Wheelchair.
- Individuals with spinal cord injuries should be orientated to their new way of mobilization. Turning, opening, and closing doors, down inclines and going up, going around and over obstacles, additionally mobilizing indoors and outdoors are important activities to practice in order to ensure safe and independent mobility.
- The recent study concludes that participants with spinal cord injuries predict the importance of fall prevention initiatives that extend beyond the offered strategies, suggesting a need for the structure and content of future fall removal strategies for wheelchair users. Further research is needed to examine the efficacy of individual fall prevention initiatives by collecting assessments from community-dwelling wheelchair users with spinal cord injuries.
Gait and standing
- Gait training, strengthening, and balance exercises were the very common physiotherapy activities in individuals with an Asia impairment scale(AIS) spinal cord injury. General strengthening was the most common group therapy activity across all situations and types of spinal cord injury.
- The ability to walk is dependent on several factors still, standing has multiple benefits even if independent standing may noway be a possibility. Benefits affect emotional well-being, orthostatic hypotension, bone mineral density, spasticity, and bladder and bowel function. Standing can be attained by using assistive devices like; tilt tables, standing wheelchairs, and standing frames. Beings with paraplegia might be effective to stand in parallel bars applying knee-extension splints.
- Gait training is possible among individuals with full paraplegia to partially paralyzed lower extremities by using orthoses and walking aids such as; knee-ankle-foot and hip-knee-ankle-foot orthoses.
Long-Term Phase
- Coordinated community rehabilitation services and long-term assistance are required to satisfy the long-term and ongoing needs of people with spinal cord injuries in order to ensure successful long-term management. Best practices in long-term management involve active case management with case managers with the appropriate training, clinical expertise, and knowledge of services to coordinate care post-initial rehabilitation and ensure ongoing personalized case management for patients with ongoing needs. A prospective longitudinal study suggests the need for screening of the efficacy of patients and their family members to support and prevent personal and family adjustment problems as low self-efficacy of the patients appears to be a risk factor for adjustment problems in being with spinal cord injuries.
Treatment objectives of the long-term phase involve:
- to achieve high-level mobility aims needed for community participation
- to monitor the recovery of function
- to reinforce family and carer training
FAQ
Cervical spinal cord injuries are commonly the most severe type of spinal cord injuries. They might affect quadriplegia or tetraplegia with associated loss of muscle strength in all four extremities. Based on the extent of the injury, cervical spinal cord injuries can exist as complete or incomplete.
Trauma is the very common cause of cervical injury, and this can involve motor vehicle accidents, falls, penetrating or blunt trauma, and sports-related or diving injuries. Nontraumatic causes can involve compression fractures from osteoporosis, arthritis, or cancer and inflammation of the spinal cord.
Your symptoms will be based on the type and severity of your injury, but the very common symptoms involve Difficulty turning the neck. Headaches. Muscle spasms in neck and shoulders.
Normally, you don’t want treatment for a bruised cervix. But ibuprofen or naproxen can support the relief of pain and discomfort. You can so apply a heating pad to your back or abdomen. Try sitting on a pillow.
Lifestyle and home remedies
1. Alternate heat and cold. Reduce inflammation by applying cold, like an ice pack or ice wrapped in a towel, for up to 15 minutes several times a day during the first 48 hours. After that, use heat.
2. Home exercises. Keeping the neck moving is important.
Neck pain treatment and remedies
apply ice or heat, Stretch, prevent rapid movements, and take over-the-counter (OTC) pain medications. Check with a physical therapist (PT), Think about chiropractic care. Consider acupuncture, schedule a massage, and avoid strenuous exercise that irritates your neck.
The results are in line with the findings of a previous study showing that increasing daily walking reduced the risk of neck pain by 14% in those with sedentary jobs.
Side-to-Side Head Rotation
Lie on your back with your knees flexion/extension and feet flat on the floor.
Rotate your chin toward your right shoulder.
Hold for 20 seconds.
Rotate your chin toward your left shoulder.
Hold for 20 seconds.
Repeat 3 to 5 times on each side.
Cervical pain is widespread and most of us will have it at a few points in our lives. Usually, cervical pain results from holding your neck in the same position for too long. still, other things can also cause or contribute to neck pain, such as worry or stress.