Complex Regional Pain Syndrome (CRPS)
Table of Contents
What is complex regional pain syndrome (CRPS)?
- Complex regional pain syndrome (CRPS) is a condition that causes pain, changes in skin color, and other symptoms in a certain part of your body — commonly in your extremities. Your extremities involve your arm, leg, hand, or foot.
- The symptoms of Complex regional pain syndrome (CRPS) can greatly impact the function of your affected limb, sleep, daily activities, and your mental health.
- Experts believe that Complex regional pain syndrome (CRPS) happens as a result of dysfunction in your central or peripheral nervous systems. Your central nervous system (CNS) contains your brain & spinal cord. Your peripheral nervous system relays information from your brain & spinal cord to your organs, arms, legs, fingers, & toes. The abnormal functioning outcomes in an overreaction to pain signals that your nervous system can not shut off.
There are 2 subtypes of Complex regional pain syndrome (CRPS):
- Type I: This type happens without nerve damage. It happens after an illness or injury that did not directly damage a nerve. Type I was before called reflex sympathetic dystrophy.
- Type II: This type happens after known nerve damage. It was formerly called causalgia.
- Complex regional pain syndrome (CRPS) can either be acute (short-term) or chronic (lasting longer than six months). It is usually treatable.
How does Complex regional pain syndrome (CRPS) affect?
- Complex regional pain syndrome (CRPS) more commonly affects adults than children. The top onset is around 40 years of age. Complex regional pain syndrome (CRPS) affects people assigned to females at birth more often than people assigned to males at birth.
- About 66% to 80% of cases happen in people of European ancestry.
How common is Complex regional pain syndrome (CRPS)?
- Complex regional pain syndrome (CRPS) is relatively rare. It harms about 200,000 people every year in the United States (US).
Symptoms of CRPS
- How serious and how long symptoms of complex regional pain syndrome (CRPS) last varies from person to person.
- Symptoms of complex regional pain syndrome (CRPS) typically start within four to six weeks after an injury, fracture, or surgery, yet they can develop without a known cause.
- The most usual and prominent symptom of complex regional pain syndrome (CRPS) is pain. The pain is continuous or intermittent and is a burning, stinging, or tearing sensation. It is often deep inside your affected limb.
Sensory changes are also usual in the affected area and may include:
- Improved sensitivity to painful stimuli (a pinch may feel more painful than usual).
- Feeling the pain from stimuli that are commonly not painful (such as just touching your skin).
- Numbness.
Other symptoms of complex regional pain syndrome (CRPS) in the affected area include:
- Skin swelling: Swelling may come and go or remain continuous.
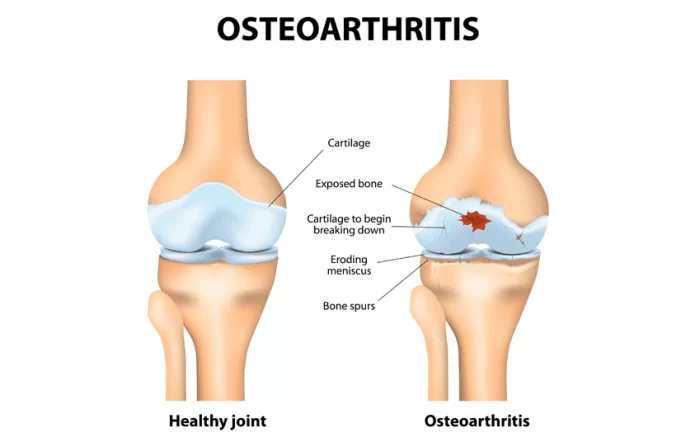
- Decreased function in your affected limb: You may experience a reduced ability to move your affected limb and/or increased stiffness. You may also have difficulty placing pressure on your harmed limb or joint.
- Changes in skin temperature: The skin on your limit may feel warmer or cooler compared to the opposite one.
- Changes in skin color: Your skin may look blotchy, pale, purple/bruised, or red.
- Changes in skin texture: Your skin may become shiny and thin or extremely sweaty.
- Changes in nail and hair growth: You may have quick hair or nail growth or no growth.
- Since the symptoms of complex regional pain syndrome (CRPS) usually improve over time, it is easiest for healthcare providers to diagnose it in the early stages. It is important to see a provider soon after you experience symptoms of complex regional pain syndrome (CRPS).
Causes CRPS
- Researchers are not sure why some people develop complex regional pain syndrome (CRPS) while others with similar injuries do not. They think it is due to an inflammatory or immune reaction in both your peripheral and central nervous systems.
- In more than 90% of cases, complex regional pain syndrome (CRPS) results from nerve trauma or injury to the affected limb that damages the thinnest sensory and autonomic nerve fibers. These little fibers transmit pain, itch, and temperature sensations. They also control the little blood vessels and the overall health of surrounding cells.
- The most common injury associated with developing complex regional pain syndrome (CRPS) is a bone fracture, especially a wrist fracture. A displaced or splintered bone or pressure from a tight cast can harm nerves.
Other common injuries that can lead to complex regional pain syndrome (CRPS) include:
- Surgery: A surgical incision, stitches, or scarring can cause nerve damage.
- Sprains or strains: When connective tissues are damaged, it can outcome in excessive movement of a joint, which over-stretches nearby nerves.
- Burns, bruises, or cuts: These are all noticeable signs of injuries that may also have harmed underlying nerves.
- CRPS can also develop without an obvious injury or due to periods of prolonged immobilization.
Certain factors that may increase your risk of developing CRPS include:
- Poor nerve health: Conditions such as diabetes can leave your nerves to decrease resilience and able to repair themselves. It may be hard for people with peripheral neuropathy to regrow their nerve cells from an injury that would not otherwise cause problems. Smoking and previous chemotherapy can also create it difficult for your nerves to regenerate.
- Immune system issues: Your immune system plays a big role in inflammation. Some people with complex regional pain syndrome (CRPS) have elevated levels of inflammatory chemicals called cytokines that contribute to certain symptoms of complex regional pain syndrome (CRPS). complex regional pain syndrome (CRPS) is also more common in people with other inflammatory and autoimmune diseases, such as asthma.
- Genetics: Your genes can harm your ability to recover from an injury. Researchers have discovered family clusters of complex regional pain syndrome (CRPS). Although this is rare, it suggests that there may be a genetic link to complex regional pain syndrome (CRPS).
How is complex regional pain syndrome (CRPS) diagnosed?
- Since complex regional pain syndrome (CRPS) is rare and healthcare providers do not totally understand it, it is often misdiagnosed.
- There is no personal test to diagnose CRPS. Healthcare providers (doctors) mainly diagnose it through a careful medical history, physical examination, and review of your symptoms. Your provider will ask you if you have had a recent injury or surgery.
They will look for:
- A change in the appearance, temperature, and texture of your skin in the affected part.
- A higher-than-expected amount of pain from harm.
- Any other disease or conditions that could cause your pain, changes in your skin, or another symptom.
- They may order imaging tests, like an ultrasound or magnetic resonance imaging (MRI), to look for underlying nerve damage. But it is not always possible to find nerve damage.
- Your provider (doctor) may also order other tests to rule out conditions that cause similar symptoms. For example, electromyography (EMG) may reveal other causes of neuropathy, which may result in certain similar pain scenarios.
What is the treatment for complex regional pain syndrome (CRPS)?
- The goal of treatment is to reduce your pain and other symptoms, restore function to the affected limb and maintain the quality of your life.
- It is important to start treatment early in the course of complex regional pain syndrome (CRPS). This is because CRPS can cause the affected limb to stiffen over time. In addition, the pain commonly worsens without treatment and movement becomes more and more difficult.
It is best to see healthcare providers who have experience in treating complex regional pain syndrome (CRPS), if possible. Treatment requires a combination of carefully managed approaches, involving:
- Physical therapy & occupational therapy,
- Lifestyle changes,
- Psychosocial & behavioral therapy,
- Medications,
- Alternative therapies for pain management.
- For young children with CRPS, psychosocial & rehabilitation therapies is the mainstay treatment. Healthcare providers commonly only suggest pain-reducing medical procedures for older adolescents who have symptoms that are not responding to other therapies.
Other aspects of physical therapy for CRPS include:
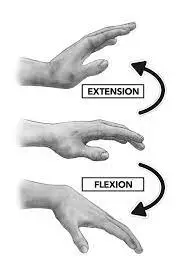
- Graded motor imagery: This is a set of treatments that assist reduce pain and improve the ability to move the affected part of your body. When one of your limbs is painful, it can become hard to touch, move or use. Your brain also has a memory or “map” of different body areas and how these feel, move, and function in daily activities. If you do not touch, move or use the affected limb, this map starts to change and can begin to disappear. However, you can exchange this map or re-established it with graded motor imagery.
- Mirror therapy: This treatment technique is 1 of the exercises of graded motor imagery. It includes looking at the reverse image of your non-painful limb in a mirror. The reflection in the mirror then appears as the harmed limb. This can “trick” your brain into thinking that the painful limb currently feels and moves as normal.
- Desensitization: This technique includes touching the affected area with materials of different textures and weights and placing the affected limb into the water of warmer and cooler temperatures. By exposing the affected area/limb to various sensations slowly over time, your brain adjusts to the sensations and pain begins to lessen.
Lifestyle changes
Removing certain barriers that can prevent your nerves from healing can help increase the chance of recovery and the speed of recovery, involving:
- Quitting smoking: Smoking very much interferes with nerve regeneration.
- Managing existing health conditions: Poor management of diabetes and other conditions that can harm circulation and nerves can make it difficult for your nerves to heal.
Other simple steps you can take at home to assist your symptoms include:
- Keeping your affected limb elevated when resting or sleeping can assist in excess fluid returning to your heart.
- Exercising every day is critical to increasing circulation to the damaged nerves. Talk to your provider or a physical therapist about an exercise plan that is appropriate for you.
- Wearing compression stockings or sleeves may assist limit swelling, particularly when standing. Tell your provider if this is an option for you.
Psychosocial and behavioral therapy
- Having complex regional pain syndrome (CRPS) is associated with worsening anxiety, depression, and stress, which can increase pain. Psychotherapy can assist. Psychotherapy, also known as talk therapy, is a term for a variety of treatment techniques that aim to assist a person to identify and change unhealthy emotions, thoughts & behaviors.
- If possible, it is best to see a pain management clinical psychologist with training in treating CRPS. During psychotherapy, you tell to the psychologist to learn ways to better cope with factors that contribute to your pain and another symptom.
Medications
- No medications are specifically approved for complex regional pain syndrome (CRPS) in the U.S. However, your healthcare provider (doctor) may recommend certain medications to manage your symptoms.
Medications that have pain-reducing effects involve:
- Nonsteroidal anti-inflammatory drugs (NSAIDs), like acetaminophen, ibuprofen, and naproxen.
- Topical analgesic creams and patches, like lidocaine.
- Certain antidepressants, like amitriptyline and duloxetine.
- Anti-seizure drugs, like gabapentin, pregabalin, and topiramate.
- Bisphosphonates, like alendronate.
- Botulinum toxin (Botox) injections.
Alternative therapies for pain management
Alternative therapies for pain management may involve:
- Biofeedback
- Acupuncture
- Hypnosis
- Reiki
- Chiropractic.
If your complex regional pain syndrome (CRPS) has not responded well to the therapies mentioned above or you have severe pain or ongoing complex regional pain syndrome (CRPS), your provider may recommend the following more invasive treatments:
- Trigger point/tender point injections: You may have trigger/tender points in the muscles in your shoulder girdle when complex regional pain syndrome (CRPS)0 is limited to your upper limb. Injection of each trigger/tender point with local anesthetics with or without glucocorticoids can help treat this type of complex regional pain syndrome (CRPS) in the early stage.
- Sympathetic nerve blocks: These blocks can provide significant pain relief for certain people. The lumbar sympathetic block includes injecting an anesthetic next to your spine in your lower back. This straight blocks the sympathetic chain that transmits the pain signal from your lower limbs to your spinal cord and brain. For upper limb complex regional pain syndrome (CRPS) pain, the block is known as stellate ganglion block, which involves injecting an anesthetic on the side of your neck.
- Spinal cord stimulation: This treatment includes surgically implanting a pulse generator device under your skin in your abdomen or buttock and wires (electrodes) near your spinal cord. The device, which is similar to a pacemaker, sends reduce-level electrical currents to your spinal cord. Electrical pulses interfere with and decrease the pain signal being sent to your brain.
- Dorsal root ganglia stimulation: This treatment is small to spinal cord stimulation except that the smaller wires are implanted right on the dorsal root ganglion, which is a cluster of sensory neurons at the junction where each and every segmental nerve exits your spinal cord. The dorsal root ganglion is a relay station of the pain signal being sent from the peripheral nervous system (PNS) (your limbs) to the central nervous system (CNS) (your spinal cord and brain). The stimulation could be a more targeted and efficient (requiring less stimulation) therapy, as it concentrates on these little relay stations.
- Peripheral nerve stimulation: This treatment places a stimulating wire near a major nerve in your limb that covers the painful part. It tasks by interfering with the pain signal conducted through the targeted nerve.
- IV ketamine infusion: This treatment uses an IV infusion of a decreased dose of ketamine for 3 to 5 days. Ketamine tasks by blocking a particular molecule (NMDA receptor) in your nervous system that can wind up and worsen your pain.
- Intrathecal drug pumps: This treatment includes using an implanted catheter to send pain-relieving drugs, such as ziconotide (Prialt), right into your spinal fluid.
Physical Therapy Treatment
- It is difficult to manage complex regional pain syndrome (CRPS) as there is a lack of understanding of the pathophysiologic abnormalities, a lack of specific diagnostic criteria, and very low-quality evidence to treat complex regional pain syndrome (CRPS). The important goals of treatment are a reduction in pain, preservation of limb function, and a return to work. Comorbidities such as depression, sleep disturbance, and anxiety also require to be addressed and treated concurrently in a patient-centered, multidisciplinary approach.
- A combination of physical and occupational therapy is effective in reducing pain and increasing function in patients who have had complex regional pain syndrome (CRPS) for less than 1 year. Physical therapy focuses on patient education about the condition & functional activities.
Physical therapy and occupational therapy
- Physical therapy is one of the most important methods of treatment for complex regional pain syndrome (CRPS).
- A physical therapist can assist improve blood flow to your affected limb as well as increase your flexibility, strength, muscle tone, and function with certain exercises. An occupational therapist can teach you current ways to accomplish everyday tasks.
Physical therapy intervention could involve any of the following:
- Transcutaneous Electrical nerve stimulation (TENS)
- Aquatic therapy allows activities to be performed with reduced weight bearing on the lower extremities
- Mirror therapy
- Desensitization
- Gradual weight bearing
- Stretching
- Fine motor control.
- It is important to recognize that complex regional pain syndrome (CRPS) typically follows blood vessel pathways, and therefore symptoms may not always follow neural patterns.
- As a result of the spread pattern, complex regional pain syndrome (CRPS) treatment should also be provided bilaterally, due to the contralateral connections present between the extremities.
- Treatment should be based on basic principles of pain management (pain and symptom relief, supportive care, rehabilitation) and due to the lack of evidence in the treatment of CRPS treatments are based on that of other neuropathic pain syndromes.
Acute Phase
- Immobilization & contralateral therapy. Intensive active therapy in the acute phase can conduct to deterioration.
Chronic Phase
- Passive physical therapy involves manipulation, manual therapy, massage, and mobilizations. Lymphatic drainage can be utilized to facilitate the regression of edema. Tender areas are recommended to be treated in the following order: more severe before decrease severe, more proximal and medial before more distally and laterally located points, and the part of the greatest accumulation of tender areas is treated first. When tender parts are located in a row, the middle is treated first.
- The therapeutic exercise involves isometric strengthening therapy followed by active isotonic training in combination with sensory desensitization programs. Strength training involves exercises for all four extremities and the trunk. Desensitization programs consist of giving stimuli of different fabrics, various pressures (light or deep), vibration, tapping, heat, or cold. The exercises can be stress-loading (i.e. walking, carrying weights), endurance training, & functional training. When complex regional pain syndrome (CRPS) occurs in the lower extremities, gait re-training is recommended.
- Mirror therapy or mirror visual feedback,
- Mirror therapy is where both hands are placed into a box with a mirror separating the 2 compartments and, whilst moving both hands, the patient watches the reflection of the unaffected hand in the mirror.
There is certainly evidence to suggest that mirror therapy has the effect of:
- Reducing pain intensity and improving function in post-stroke CRPS,
- A significant improvement in pain,
- Improving function (low-quality evidence, however),
- Graded motor imagery/learning is effective. However, further trials are needed GMI plus medical management is more effective than medical management plus physiotherapy GMI may reduce pain and increase function. Other therapies involve relaxation, cognitive-behavioral therapy, deep breathing exercises, and biofeedback.
Neuromodulation or Invasive Stimulation Techniques
- Neuromodulation accommodates peripheral nerve stimulation with implanted electrodes, epidural spinal cord stimulation, deep brain stimulation & electrotherapy.
- Electrotherapy involves transcutaneous electric nerve stimulation TENS, spinal cord stimulation (SCS), and non-invasive brain stimulation (repetitive transcranial magnetic stimulation). These techniques help to reduce pain, although further trials are needed.
- Other Treatments
- Whirlpool bath/ contrast baths
- Vocational and recreational rehabilitation
- Psychological therapies: cognitive-behavioral therapy (CBT), operant conditioning (OC), counseling, pain education, and relaxation techniques
- Acupuncture, electroacupuncture
- Tactile sensory discrimination training
- Weight-bearing
- Ultrasound therapy
- Kinesio taping.
Can I prevent complex regional pain syndrome (CRPS)?
- Since researchers do not know the exact cause of complex regional pain syndrome (CRPS), there is no conclusive way to prevent it. Certain studies have revealed that taking vitamin C before a future surgery might prevent complex regional pain syndrome (CRPS).
What can I expect if I have complex regional pain syndrome (CRPS)?
- Each person’s experience with complex regional pain syndrome (CRPS) is different. Complex regional pain syndrome (CRPS) mostly improves over time and eventually goes away (goes into remission) in most people.
- Severe or prolonged cases, which are rare, can greatly harm your life. In some people, complex regional pain syndrome (CRPS) gets worse and even spreads to other areas of their bodies. Experiencing increased psychological distress during the injury that led to complex regional pain syndrome (CRPS) may affect its severity and prognosis.
- complex regional pain syndrome (CRPS) recurs (happens again) in about 10% to 30% of people. Most recurrences are caused by unknown reasons.
- The most important goals are to relieve pain and restore movement and strength in the harmed limb. By achieving pain relief, you improve the odds of improving its function and quality of life. Carefully selected treatment plans allow some people with CRPS to successfully manage their pain and lead active lives.
When should I see my healthcare provider?
Because of the complexity of this condition and the fact that it is often misdiagnosed, seek out a pain management specialist or a specialty pain center with knowledge of complex regional pain syndrome (CRPS) if:
- You think you have symptoms of complex regional pain syndrome (CRPS).
- Your symptoms are getting worsen.
- Your condition has not responded to another treatment method.
FAQs
The three (3) clinical stages of type 1 complex regional pain syndrome (CRPS 1) are acute, subacute, and chronic. The acute form lasts approximately 3 months. Pain, often burning in nature, is one of the 1st symptoms that initially limits function.
Complex regional pain syndrome (CRPS) is a broad term describing excess and long-term pain and inflammation following an arm or leg injury. complex regional pain syndrome (CRPS) has acute (recent, short-term) and chronic (lasting greater than six months) forms. complex regional pain syndrome (CRPS) used to be known as reflex sympathetic dystrophy (RSD) and causalgia.
There is no known cure for complex regional pain syndrome (CRPS), but a combination of physical treatments, medicine, and psychological support can help manage the symptoms. It is estimated around 85% of people with complex regional pain syndrome (CRPS) slowly experience a reduction in their pain and some of their symptoms in the first 2 years.
complex regional pain syndrome (CRPS) is divided into two groups: Type 1: Also known as sympathetic dystrophy, which develops without known nerve damage. Type 2: Also known as causalgia, which is the result of specific nerve damage.
If left untreated, complex regional pain syndrome (CRPS) can lead to serious problems, such as Tissue wasting (atrophy). If you won’t move his harmed limb because of pain or stiffness, their skin, bones, and muscles will weaken. Muscle tightening (contracture).
The exact cause of complex regional pain syndrome is not well understood yet may involve abnormal inflammation or nerve dysfunction. The pain of this condition is higher than would be expected from the injury that causes it. Typically, complex regional pain syndrome (CRPS) is a permanent disability as there is no cure for it.
Complex regional pain syndrome (CRPS) is a debilitating chronic pain disorder that can negatively impact physical, mental, and social health. Depression, anxiety, trauma, insomnia, and substance use disorders might occur in harmed patients. The etiology of complex regional pain syndrome (CRPS) appears to be multifactorial; therefore, effective treatment should be multidisciplinary.
Despite their difficulties and the struggles they continue to face as sufferers of reflex sympathetic dystrophy (RSD) or causalgia, they have been able to live normal, and in some cases rather extraordinary, lives. The key to having a good prognosis with complex regional pain syndrome (CRPS) is to continue treatment and not give up.
Conclusions: MRI cannot distinguish between complex regional pain syndrome (CRPS) and non-CRPS patients. The role of MR imaging in patients with suspected complex regional pain syndrome (CRPS) is to exclude alternative diagnoses that would better explain patients’ symptoms.
In more than 90% of cases, complex regional pain syndrome (CRPS) results from nerve trauma or injury to the affected limb that damages the thinnest sensory and autonomic nerve fibers. These small fibers transmit pain, itch, and temperature sensations.
Flares can be mild or severe, short or long, and can occur because of many reasons, involving the following: Weather changes.
REST/MEDITATION/DEEP BREATHING. This method is useful, and it works.
MASSAGE/STRETCHING
PAIN SPRAY
TENS
DISTRACTION.
complex regional pain syndrome (CRPS) commonly presents with redness and swelling at the site of the injury. The site might be hot to the touch. In addition to the pain, patients might feel numbness, tingling, or a burning sensation.
Additionally, complex regional pain syndrome (CRPS)) patients often experience cognitive changes, anxiety, and depression. The supraspinal mechanisms linked to these complex regional pain syndrome (CRPS)-related comorbidities remain poorly understood.





2 Comments