Perthes disease
Perthes disease is a rare childhood condition that affects the hip. It occurs when the blood supply to the rounded head of the femur (thighbone) is temporarily disrupted. Without an adequate blood supply, the bone cells die, a process called avasculaAlthough the term “disease” is still used, Perthes is really a complex process of stages that can last several years. As the condition progresses, the weakened bone of the head of the femur (the “ball” of the “ball-and-socket” joint of the hip) gradually begins to break apart. Over time, the blood supply to the head of the femur returns and the bone begins to grow back.
Treatment for Perthes focuses on helping the bone grow back into a more rounded shape that still fits into the socket of the hip joint. This will help the hip joint move normally and prevent hip problems in adulthood.

The long-term prognosis for children with Perthes is good in most cases. After 18 months to 2 years of treatment, most children return to daily activities without major limitations.
Table of Contents
Description
Perthes disease — also known as Legg-Calve-Perthes, named for the three individual doctors who first described the condition — typically occurs in children who are between 4 and 10 years old. It is five times more common in boys than in girls, however, it is more likely to cause extensive damage to the bone in girls. In 10% to 15% of all cases, both hips are affected.
There are four stages in Perthes disease:
Initial / necrosis. In this stage of the disease, the blood supply to the femoral head is disrupted and bone cells die. The area becomes intensely inflamed and irritated and your child may begin to show signs of the disease, such as a limp or different way of walking. This initial stage may last for several months.
Fragmentation. Over a period of 1 to 2 years, the body removes the dead bone and quickly replaces it with an initial, softer bone (“woven bone”). It is during this phase that the bone is in a weaker state and the head of the femur is more likely to break apart and collapse.
Reossification. New, stronger bone develops and begins to take shape in the head of the femur. The reossification stage is often the longest stage of the disease and can last a few years.
Healed. In this stage, the bone regrowth is complete and the femoral head has reached its final shape. How close the shape is to round will depend on several factors, including the extent of damage that took place during the fragmentation phase, as well as the child’s age at the onset of disease, which affects the potential for bone regrowth.
Pathology
Over time, healing occurs by new blood vessels infiltrating the dead bone and removing the necrotic bone which leads to a loss of bone mass and a weakening of the femoral head. The bone loss leads to some degree of collapse and deformity of the femoral head and sometimes secondary changes to the shape of the hip socket.

It is also referred to as idiopathic avascular osteonecrosis of the capital femoral epiphysis of the femoral head since the cause of the interruption of the blood supply of the head of the femur in the hip joint is unknown.
Perthes can produce a permanent deformity of the femoral head, which increases the risk of developing osteoarthritis in adults. Perthes is a form of osteochondritis that only affects the hip, although other forms of osteochondritis can affect elbows, knees, ankles, and feet. Bilateral Perthes, which means both hips are affected, should always be investigated thoroughly to rule out multiple epiphyseal dysplasia.
Cause
The cause of Perthes disease is not known. Some recent studies indicate that there may be a genetic link to the development of Perthes, but more research needs to be conducted.
Symptoms
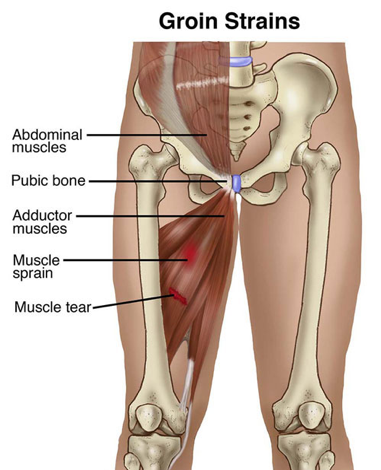
One of the earliest signs of Perthes is a change in the way your child walks and runs. This is often most apparent during sports activities. Your child may limp, have limited motion, or develop a peculiar running style. Other common symptoms include:
Pain in the hip or groin, or in other parts of the leg, such as the thigh or knee (called “referred pain.”).
Pain that worsens with activity and is relieved with rest.
Painful muscle spasms may be caused by irritation around the hip.
Depending upon your child’s activity level, symptoms may come and go over a period of weeks or even months before a doctor visit is considered.
an occasional limp in the earlier stages.
stiffness and reduced range of movement in the hip joint.
pain in the knee, thigh, or groin when putting weight on the affected leg or moving the hip joint.
thinner thigh muscles on the affected leg.
shortening of the affected leg, leading to uneven leg length.
worsening pain and limping as time goes by.
Doctor Examination
After discussing your child’s symptoms and medical history, your doctor will conduct a thorough physical examination.
Physical examination tests
Your doctor will assess your child’s range of motion in the hip. Perthes typically limits the ability to move the leg away from the body (abduction), and twist the leg toward the inside of the body (internal rotation).
X-rays. These scans create pictures of dense structures like bone, and are required to confirm a diagnosis of Perthes. X-rays will show the condition of the bone in the femoral head and help your doctor determine the stage of the disease.
A child with Perthes can expect to have several x-rays taken over the course of treatment, which may be 2 years or longer. As the condition progresses, x-rays often look worse before gradual improvement is seen.
Treatment
The goal of treatment is to relieve painful symptoms, protect the shape of the femoral head, and restore normal hip movement. If left untreated, the femoral head can deform and not fit well within the acetabulum, which can lead to further hip problems in adulthood, such as the early onset of arthritis.
There are many treatment options for Perthes disease. Your doctor will consider several factors when developing a treatment plan for your child, including:
Your child’s age. Younger children (age 6 and below) have a greater potential for developing new, healthy bones.
The degree of damage to the femoral head. If more than 50% of the femoral head has been affected by necrosis, the potential for regrowth without deformity is lower.
The stage of disease at the time your child is diagnosed. How far along your child is in the disease process affects which treatment options your doctor will recommend.
Nonsurgical Treatment
Observation. For very young children (those 2 to 6 years old) who show few changes in the femoral head on their initial x-rays, the recommended treatment is usually simple observation. Your doctor will regularly monitor your child using x-rays to make sure the regrowth of the femoral head is on track as the disease runs its course.
Anti-inflammatory medications. Painful symptoms are caused by inflammation of the hip joint. Anti-inflammatory medicines, such as ibuprofen, are used to reduce inflammation, and your doctor may recommend them for several months. As your child progresses through the disease stages, your doctor will adjust or discontinue dosages.
Limiting activity. Avoiding high-impact activities, such as running and jumping, will help relieve pain and protect the femoral head. Your doctor may also recommend crutches or a walker to prevent your child from putting too much weight on the joint.
Physiotherapy exercises
Hip stiffness is common in children with Perthes disease and physiotherapy exercises are recommended to help restore the hip joint range of motion. These exercises often focus on hip abduction and internal rotation. Parents or other caregivers are often needed to help the child complete the exercises.
Hip abduction. The child lies on his or her back, keeping knees bent and feet flat. He or she will push the knees out and then squeeze the knees together. Parents should place their hands on the child’s knees to assist with reaching a greater range of motion.

Hip rotation. With the child on his or her back and legs extended out straight, parents should roll the entire leg inward and outward.
Casting and bracing. If a range of motion becomes limited or if x-rays or other image scans indicate that a deformity is developing, a cast or brace may be used to keep the head of the femur in its normal position within the acetabulum.
Petrie casts are two long-leg casts with a bar that hold the legs spread apart in a position similar to the letter “A.” Your doctor will most likely apply the initial Petrie cast in an operating room in order to have access to specific equipment.
Arthrogram. During the procedure, your doctor will take a series of special x-ray images called arthrograms to see the degree of deformity of the femoral head and to make sure he or she positions the head accurately. In an arthrogram, a small amount of dye is injected After the cast is removed, usually, after 4 to 6 weeks, physical therapy exercises are resumed. Your doctor may recommend continued intermittent casting until the hip enters the final stage of the healing process.
Advice and education on the condition and providing recommendations on relevant rest to assist with decreasing pain.
Stretching exercises for the hip.
Progressive strengthening exercises for the hip and leg.
Crutches to decrease weight-bearing if walking is particularly sore.
At times conservative treatment may also involve traction, where the hip is gently pulled out from the socket to help relieve pain; or casting to maintain femoral head alignment.
Surgery may be required in more severe cases. Surgery is aimed at improving joint alignment and the contour of the femoral head. Surgical methods range from releasing tight muscles around the hip to joint realignment. Post surgery, your physiotherapist can help to provide stretching and strengthening exercises to assist with recovery and a return to activity.




2 Comments