Trancutaneous Electrical nerve stimulation (TENS)
Table of Contents
INTRODUCTION OF TENS
TENS is a method of electrical stimulation that primarily aims to provide a degree of symptomatic pain relief by exciting sensory nerves and thereby stimulating either the pain gate mechanism and/or the opioid system. The different methods of applying TENS relate to these different physiological mechanisms.
The effectiveness of TENS varies with the clinical pain being treated, but research would suggest that when used ‘well’ it provides significantly greater pain relief than a placebo intervention. There is an extensive research base for TENS in both the clinical and laboratory settings and whilst this summary does not provide a full review of the literature, the key papers are referenced.
It is worth noting that the term TENS could represent the use of ANY electrical stimulation using skin surface electrodes which has the intention of stimulating nerves. In the clinical context, it is most commonly assumed to refer to the use of electrical stimulation with the specific intention of providing symptomatic pain relief. If you do a literature search on the term TENS, do not be surprised if you come across a whole lot of ‘other’ types of stimulation that technically fall into this grouping.
MECHANISM OF ACTION OF TENS
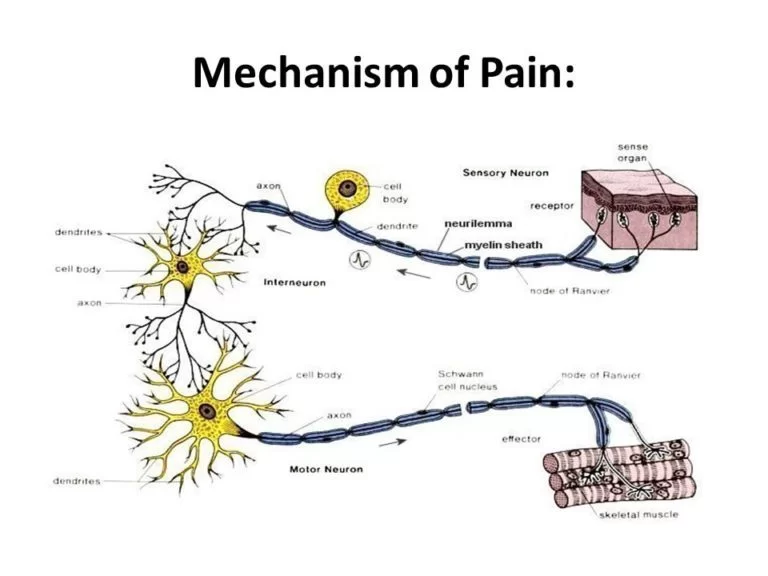
- The type of stimulation delivered by the TENS unit aims to excite (stimulate) the sensory nerves, and by so doing, activate specific natural pain relief mechanisms. For convenience, if one considers that there are two primary pain relief mechanisms that can be activated: the Pain Gate Mechanism and the Endogenous Opioid System, the variation in stimulation parameters used to activate these two systems will be briefly considered.
- Pain relief by means of the pain gate mechanism involves activation (excitation) of the A beta (Aß) sensory fibres, and by doing so, reduces the transmission of the noxious stimulus from the ‘c’ fibres, through the spinal cord and hence on to the higher centres. The Aß fibres appear to appreciate being stimulated at a relatively high rate (in the order of 90 – 130 Hz or pps). It is difficult to find support for the concept that there is a single frequency that works best for every patient, but this range appears to cover the majority of individuals. Clinically it is important to enable the patient to find their optimal treatment frequency – which will almost certainly vary between individuals. Setting the machine and telling the patient that this is the ‘right’ setting is almost certainly not going to be the maximally effective treatment, though of course, some pain relief may well be achieved.
- An alternative approach is to stimulate the A delta (Ad) fibres which respond preferentially to a much lower rate of stimulation (in the order of 2 – 5 Hz), which will activate the opioid mechanisms, and provide pain relief by causing the release of an endogenous opiate (encephalin) in the spinal cord which will reduce the activation of the noxious sensory pathways. In a similar way to the pain gate physiology, it is unlikely that there is a single (magic) frequency in this range that works best for everybody – patients should be encouraged to explore the options where possible.
- A third possibility is to stimulate both nerve types at the same time by employing a burst mode stimulation. In this instance, the higher frequency stimulation output (typically at about 100Hz) is interrupted (or burst) at the rate of about 2 – 3 bursts per second. When the machine is ‘on’, it will deliver pulses at the 100Hz rate, thereby activating the Aß fibres and the pain gate mechanism, but by virtue of the rate of the burst, each burst will produce excitation in the Ad fibres, therefore stimulating the opioid mechanisms. For some patients, this is by far the most effective approach to pain relief, though as a sensation, numerous patients find it less acceptable than some other forms of TENS as there is more of a ‘grabbing’, ‘clawing’ type sensation and usually more by way of muscle twitching than with the high or low-frequency modes.
- TENS as a treatment technique is non-invasive and has few side effects when compared with drug therapy. The most common complaint is an allergic type skin reaction (about 2-3% of patients) and this is almost always due to the material of the electrodes, the conductive gel, or the tape employed to hold the electrodes in place. Most TENS applications are now made using self-adhesive, pre-gelled electrodes which have several advantages including reduced cross-infection risk, ease of application, lower allergy incidence rates, and lower overall cost. Digital TENS machines are becoming more widely available and extra features (like automated frequency sweeps and more complex stimulation patterns) are emerging, though there remains little clinical evidence for enhanced efficacy at the present time. Some of these devices do offer pre-programmed and/or automated treatment settings.
TENS Modes
1 Traditional TENS (Hi TENS, Normal TENS)
2 Acupuncture TENS (Lo TENS, AcuTENS)
3 Brief Intense TENS
4 Burst Mode TENS
5 Modulation Mode TENS
CONTRAINDICATIONS OF TENS
- Patients who do not comprehend the physiotherapist’s instructions or who are unable to co-operate
It has been widely cited that application of the electrodes over the trunk, abdomen or pelvis during pregnancy is contraindicated BUT a recent review suggests that although not an ideal (first line) treatment option, application of TENS around the trunk during pregnancy can be safely applied, and no detrimental effects have been reported in the literature. - TENS during labour for pain relief is both safe and effective
- Patients with a Pacemaker should not be routinely treated with TENS though under carefully controlled conditions it can be safely applied. It is suggested that routine application of TENS for a patient with a pacemaker or any other implanted electronic device should be considered a contraindication.
- Patients who have an allergic response to the electrodes, gel, or tape
- Electrode placement over dermatological lesions e.g. dermatitis, eczema
- Application over the anterior aspect of the neck or carotid sinus
PRECAUTIONS IN TENS
- If there is abnormal skin sensation, the electrodes should preferably be positioned elsewhere to ensure effective stimulation
Electrodes should not be placed over the eyes - Patients who have epilepsy should be treated at the discretion of the therapist in consultation with the appropriate medical practitioner as there have been anecdotal reports of adverse outcomes, most especially (but not exclusively) associated with treatments to the neck and upper thoracic areas
- Avoid active epiphyseal regions in children (though there is no direct evidence of adverse effect)
- The use of abdominal electrodes during labour may interfere with foetal monitoring equipment and is, therefore, best avoided.
USES OF TENS
- Transcutaneous electrical nerve stimulation (TENS) is a therapy that uses low-voltage electrical current for pain relief. You do TENS with a small, battery-powered machine about the size of a pocket radio. Usually, you connect two electrodes (wires that conduct electrical current) from the machine to your skin. The electrodes are often placed on the area of pain or at a pressure point, creating a circuit of electrical impulses that travels along nerve fibers. When the current is delivered, some people experience less pain. This may be because the electricity from the electrodes stimulates the nerves in an affected area and sends signals to the brain that block or “scramble” normal pain signals. Another theory is that the electrical stimulation of the nerves may help the body to produce natural painkillers called endorphins, which may block the perception of pain.
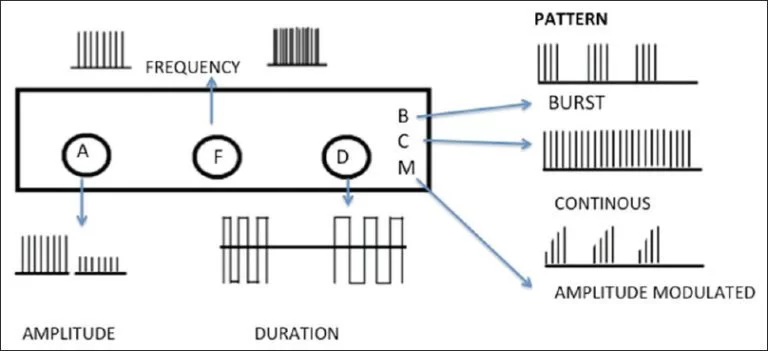
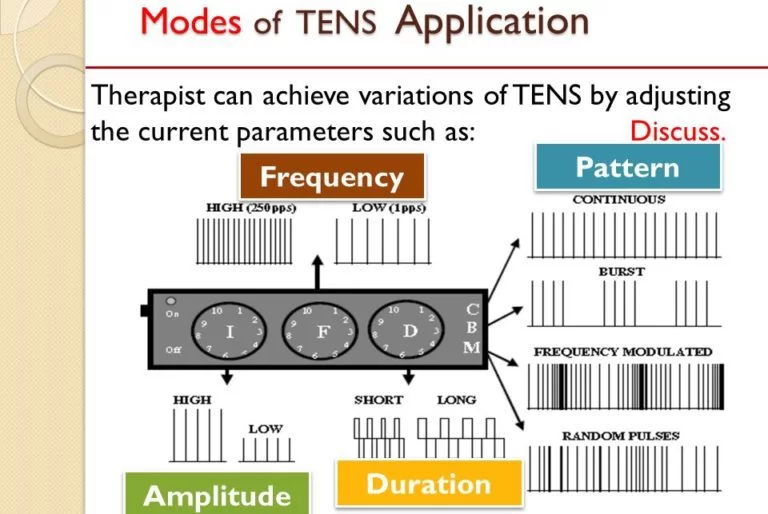
- You can set the TENS machine for different wavelength frequencies, such as a steady flow of electrical current or a burst of electrical current, and for intensity of electrical current. Your physical therapist, acupuncturist, or doctor usually determines these settings.
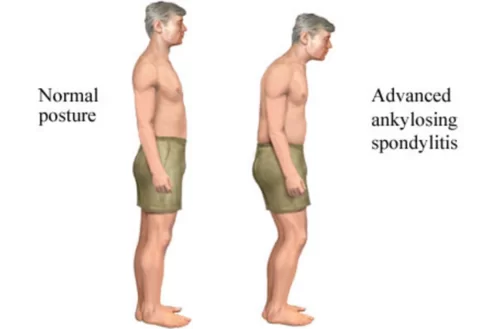
People use TENS to relieve pain for several different types of illnesses and conditions. They use it most often to treat muscle, joint, or bone problems that occur with illnesses such as osteoarthritis or fibromyalgia, or for conditions such as low back pain, neck pain, tendinitis, or bursitis. People have also used TENS to treat sudden (acute) pain, such as labor pain, and long-lasting (chronic) pain, such as cancer pain. Although TENS may help relieve pain for some people, its effectiveness has not been proven.TENS devices available to the domestic market are used as a non-invasive nerve stimulation intended to reduce both acute and chronic pain. One review from 2007 felt that the evidence supports a benefit in chronic musculoskeletal pain while another review (from the Cochrane Collaboration in 2008) deemed the evidence of poor quality and thus no conclusions were possible regarding chronic pain. Results from a task force on neck pain in 2008 found no clinically significant benefit to TENS for the treatment of neck pain when compared to placebo treatment. A 2010 review did not find evidence to support the use of TENS for chronic low back pain. There is tentative evidence that it may be useful for painful diabetic neuropathy. As of 2015, the efficacy of TENS therapy for phantom limb pain is not known as no randomized controlled trials have been performed. - In principle, an adequate intensity of stimulation is necessary to achieve pain relief with TENS. An analysis of treatment fidelity (meaning that the delivery of TENS in a trial was in accordance with current clinical advice, such as using “a strong but comfortable sensation” and suitable, frequent treatment durations) showed that higher fidelity trials tended to have a positive outcome.
- A few studies have shown objective evidence that TENS may modulate or suppress pain signals in the brain. One used evoked cortical potentials to show that electric stimulation of peripheral A-beta sensory fibers reliably suppressed A-delta fiber nociceptive processing. Two other studies used functional magnetic resonance imaging (fMRI): one showed that high-frequency TENS produced a decrease in pain-related cortical activations in patients with carpal tunnel syndrome, while the other showed that low-frequency TENS decreased shoulder impingement pain and modulated pain-induced activation in the brain.
- A head-mounted TENS device called Cefaly was approved by the United States Food and Drug Administration, on March 11, 2014, for the prevention of migraines. The Cefaly device was found effective in preventing migraine attacks in a randomized sham-controlled trial. This was the first TENS device that the FDA approved for pain prevention, as opposed to pain suppression.
Labor pain. - A significant number of TENS machine brands have been targeted for use for labor pain, although a 1997 report of a study done by the University of Oxford said that TENS “has been shown not to be effective in postoperative and labour pain. Use is in obstetric care, particularly in labor. Protocol for Various Methods of TENS
SAFETY IN TENS
- There are several anatomical locations where TENS electrodes are contraindicated:
- Over the eyes due to the risk of increasing intraocular pressure.
Transcerebrally
On the front of the neck due to the risk of an acute hypotension (through a vasovagal response) or even a laryngospasm
Through the chest using anterior and posterior electrode positions, or other transthoracic applications understood as “across a thoracic diameter”; this does not preclude coplanar applications
Internally, except for specific applications of dental, vaginal, and anal stimulation that employ specialized TENS units
On broken skin areas or wounds, although it can be placed around wounds.
Over a tumor/malignancy (based on in vitro experiments where electricity promotes cell growth)
Directly over the spinal column - TENS used across an artificial cardiac pacemaker (or another indwelling stimulator, including across its leads) may cause interference and failure of the implanted device. Serious accidents have been recorded in cases when this principle was not observed. A 2009 review in this area suggests that electrotherapy, including TENS, “are best avoided” in patients with pacemakers or implantable cardioverter-defibrillators (ICDs). They add that “there is no consensus and it may be possible to safely deliver these modalities in a proper setting with device and patient monitoring”, and recommend further research. The review found several reports of ICDs administering inappropriate treatment due to interference with TENS devices, but notes that the reports on pacemakers are mixed: some non-programmable pacemakers were inhibited by TENS, but others were unaffected or auto-reprogrammed.
- The use of TENS is likely to be less effective in areas of numb skin/decreased sensation due to nerve damage. It may also cause skin irritation due to the inability to feel currents until they are too high. There’s an unknown level of risk when placing electrodes over an infection (possibly spreading due to muscle contractions), but cross-contamination with the electrodes themselves is of greater concern. TENS should also be used with caution in people with epilepsy or pregnant women; do not use over an area of the uterus as the effects of electrical stimulation over the developing fetus are not known.
METHODS OF APPLICATION
- TENS devices do offer pre-programmed and/or automated treatment settings. The type of stimulation delivered by the TENS unit aims to excite (stimulate) the sensory nerves, and by so doing, activate specific natural pain relief mechanisms. For convenience, if one considers that there are two primary pain relief mechanisms that can be activated: the Pain Gate Mechanism and the Endogenous Opioid System, the variation in stimulation parameters used to activate these two systems will be briefly considered.
- Pain relief by means of the pain gate mechanism involves activation (excitation) of the A beta (Aβ) sensory fibres, and by doing so, reduces the transmission of the noxious stimulus from the ‘c’ fibres, through the spinal cord and hence on to the higher centres. The Aβ fibres appear to appreciate being stimulated at a relatively high rate (in the order of 90 – 130 Hz or pps). It is difficult to find support for the concept that there is a single frequency that works best for every patient, but this range appears to cover the majority of individuals. Clinically it is important to enable the patient to find their optimal treatment frequency – which will almost certainly vary between individuals. Setting the machine and telling the patient that this is the ‘right’ setting is almost certainly not going to be the maximally effective treatment, though of course, some pain relief may well be achieved.
- An alternative approach is to stimulate the A delta (Aδ) fibres which respond preferentially to a much lower rate of stimulation (in the order of 2 – 5 Hz), which will activate the opioid mechanisms, and provide pain relief by causing the release of an endogenous opiate (encephalin) in the spinal cord which will reduce the activation of the noxious sensory pathways. In a similar way to the pain gate physiology, it is unlikely that there is a single (magic) frequency in this range that works best for everybody – patients should be encouraged to explore the options where possible.
- A third possibility is to stimulate both nerve types at the same time by employing a burst mode stimulation. In this instance, the higher frequency stimulation output (typically at about 100Hz) is interrupted (or burst) at the rate of about 2 – 3 bursts per second. When the machine is ‘on’, it will deliver pulses at the 100Hz rate, thereby activating the Aβ fibres and the pain gate mechanism, but by virtue of the rate of the burst, each burst will produce excitation in the Aδ fibres, therefore stimulating the opioid mechanisms. For some patients, this is by far the most effective approach to pain relief, though as a sensation, numerous patients find it less acceptable than some other forms of TENS as there is more of a ‘grabbing’, ‘clawing’ type sensation and usually more by way of muscle twitching than with the high or low-frequency modes.
- TENS as a treatment technique is non-invasive and has few side effects when compared with drug therapy. The most common complaint is an allergic type skin reaction (about 2-3% of patients) and this is almost always due to the material of the electrodes, the conductive gel, or the tape employed to hold the electrodes in place. Most TENS applications are now made using self-adhesive, pre-gelled electrodes which have several advantages including reduced cross-infection risk, ease of application, lower allergy incidence rates and lower overall cost. Digital TENS machines are becoming more widely available and extra features (like automated frequency sweeps and more complex stimulation patterns) are emerging, though there remains little clinical evidence for enhanced efficacy at the present time.
PROTOCOL FOR VARIOUS METHODS OF TENS
PARAMETER HIGH TENS LOW TENS BRIEF INTENSE TENS
INTENSITY sensory motor noxious
PULSE FQ. 6-100 pps 2-4 pps variable
PULSE DURATION MODE modulated modulated burst modulated
TREATMENT DURATION as needed 30 min 15-30 min
ONSET OF RELIEF <10 min 20-40 min <15 min
FAQs
Electric current is used in transcutaneous electrical nerve stimulation, or TENS, a technique that stimulates nerves to reduce pain. The TENS unit is a tiny, frequently battery-powered gadget that occasionally even fits in a pocket.
Not everyone has success with TENS. It shouldn’t hurt, although it can be uncomfortable. The area of your skin where the electrodes are inserted may become irritated. You cannot use TENS in the shower or bathtub.
The first kind is called Conventional TENS, and it has a high frequency and low intensity. Second, low-frequency and high-intensity TENS are used in acupuncture. Intense TENS, which employs both high frequency and high intensity, is the third kind. Burst mode TENS is the fourth type, and modulated TENS is the fifth.
Transcutaneous electrical nerve stimulation, or TENS, is a non-invasive electrical stimulation treatment not used to stimulate neuron regeneration while used to reduce pain.
A TENS machine can be used as frequently as you’d like without risk. Usually for three to six hours, up to four times a day. Up to four hours of relief is possible with TENS.
TENS reduces pain by stimulating a sophisticated neural network. TENS stimulates large diameter afferent axons at frequencies and intensities used in therapeutic settings. In order to lessen hyperalgesia, the central nervous system receives this afferent input and activates descending inhibitory networks.





46 Comments