Lipedema
Table of Contents
What is a Lipedema?
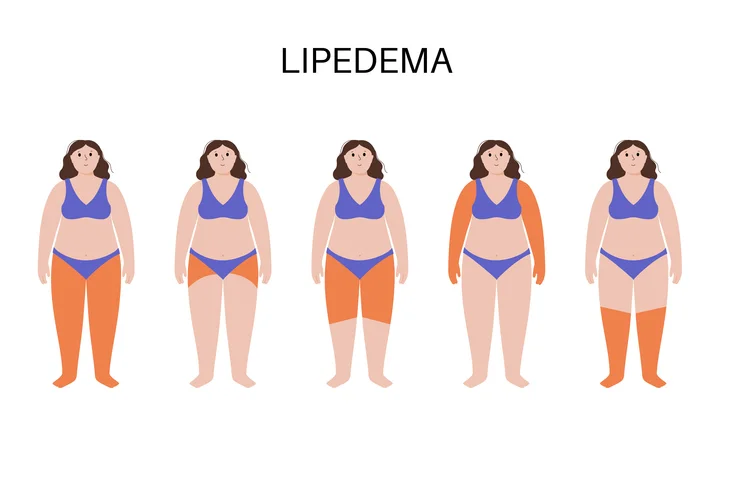
Lipedema is a chronic and progressive disorder characterized by the abnormal accumulation of fat cells in specific areas of the body, primarily in the lower limbs such as the thighs, hips, and lower legs. It predominantly affects women and is often symmetric, meaning both sides of the body are affected equally. Lipedema typically spares the feet, giving rise to a “bracelet” or “cuff” appearance at the ankles.
The condition is believed to have a genetic basis, and it is thought to be triggered or exacerbated by hormonal changes, such as puberty, pregnancy, or menopause. Although the exact cause is not fully understood, it is believed that there is an impaired flow of lymphatic fluid in the affected areas, leading to the accumulation of adipose tissue (fat).
Lipedema is not caused by overeating or a sedentary lifestyle, and it can be challenging to manage through diet and exercise alone. Individuals with lipedema may experience pain, tenderness, and easy bruising in the affected areas, and the condition can lead to reduced mobility and decreased quality of life if left untreated.
Causes of Lipedema
The exact causes of lipedema are not fully understood, but research suggests that both genetic and hormonal factors play a role in its development. Here are some of the key factors believed to contribute to the development of lipedema.
- Genetic Predisposition: Lipedema tends to run in families, indicating a genetic component to the condition. Specific genes or gene mutations may influence how fat cells are distributed and stored in the body, leading to the abnormal accumulation of fat in certain areas.
- Hormonal Influence: Hormones are thought to play a significant role in the development of lipedema, as the condition predominantly affects women and often becomes more pronounced during hormonal changes like puberty, pregnancy, and menopause. Estrogen, in particular, may influence fat metabolism and the function of the lymphatic system, which could contribute to lipedema development.
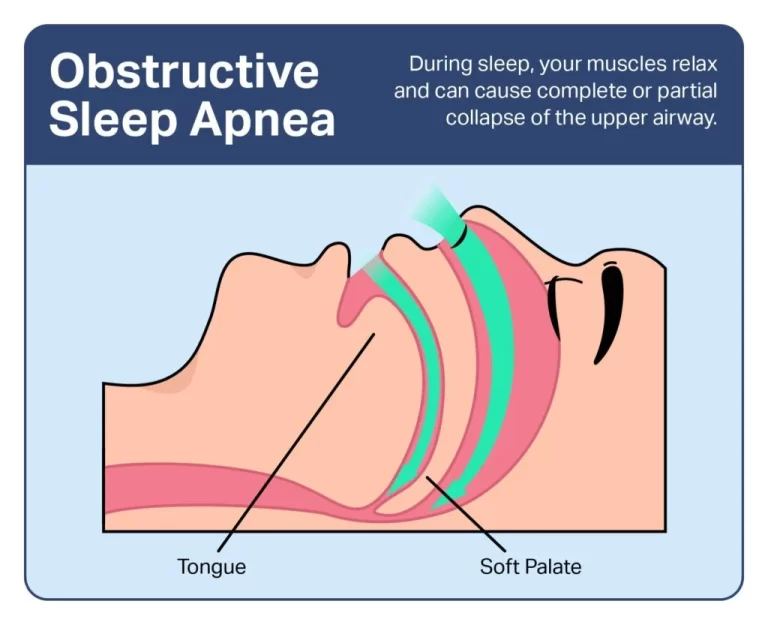
- Lymphatic Dysfunction: The lymphatic system is responsible for draining excess fluid, waste products,and immune cells from tissues. In lipedema, there is believed to be an impaired flow of lymphatic fluid,which can lead to the accumulation of fat cells in the affected areas.
- Inflammatory Processes: Chronic low-level inflammation has been observed in individuals with lipedema. Inflammation may contribute to changes in fat cell metabolism and tissue remodeling, further promoting the abnormal storage of fat.
- Trauma or Trigger Events: Some cases of lipedema have been associated with a history of trauma, such as surgery, injury, or severe stress. These events may act as triggers that worsen or accelerate the development of lipedema in individuals who are already genetically predisposed.
Symptoms of Lipedema
Lipedema is characterized by several distinctive symptoms, primarily involving the distribution of adipose (fat) tissue and associated physical discomfort. The condition typically affects the lower extremities, but in some cases, it can also involve the arms. Here are the common symptoms of lipedema:
- Abnormal Fat Accumulation: Lipedema is characterized by a symmetrical and disproportionate accumulation of fat cells in specific areas of the body, most commonly in the hips, thighs, and lower legs. The fat distribution appears to be out of proportion with the rest of the body, giving affected areas a”column-like” or “pear-shaped” appearance.
- No Involvement of Hands and Feet: One characteristic feature of lipedema is that it usually spares the hands and feet. This means that while the lower limbs may be significantly affected, the hands and feet remain relatively normal in size.
- Easy Bruising: People with lipedema often experience easy bruising and increased sensitivity to pressure in the affected areas. This is because the fat tissue is softer and more fragile than normal fat, making it more susceptible to bruising.
- Pain and Tenderness: Lipedema can cause pain and tenderness in the affected areas. This discomfort may range from mild to severe and can be exacerbated by standing or walking for extended periods.
- Swelling and Edema: Over time, lipedema can lead to swelling (edema) in the affected limbs. The swelling is usually non-pitting, meaning that pressing on the swollen area does not leave an indentation.
- Texture Changes: The skin over the affected areas may have a “mattress-like” or “orange peel” texture due to the accumulation of fat and fluid.
- Progression and Worsening: Lipedema is a progressive condition, meaning that the symptoms tend to worsen over time if left untreated. The excess fat accumulation can become more pronounced and may lead to increased pain and decreased mobility.
- Emotional Impact: Lipedema can have a significant emotional impact on affected individuals due to changes in body shape and size. Many people with lipedema may experience body image concerns and feelings of self-consciousness.
- Lymphedema: Lymphedema is a condition characterized by swelling (edema) caused by a malfunctioning lymphatic system. It often affects one limb, and unlike lipedema, it can involve the hands and feet. Lymphedema can result from surgery, radiation therapy, infection, or congenital malformation of the lymphatic system.
- Dercum’s Disease (Adiposis Dolorosa): Dercum’s disease is a rare condition characterized by painful fatty deposits (lipomas) throughout the body. While it also involves abnormal fat accumulation, it differs from lipedema in terms of pain distribution, lack of tenderness, and the presence of lipomas.
- Obesity: Obesity is a medical condition characterized by excessive body fat accumulation, but it differs from lipedema in terms of fat distribution patterns. Lipedema tends to spare the hands and feet, while obesity leads to a more generalized fat distribution.
- Venous Insufficiency: Venous insufficiency is a condition where the veins in the legs have difficulty returning blood to the heart, leading to swelling, varicose veins, and skin changes. It can sometimes be mistaken for lipedema due to the presence of leg swelling, but it lacks the characteristic fat distribution patterns of lipedema.
- Lipoedema (Lipoedema): Lipoedema is a condition similar to lipedema, but it primarily affects the legs and arms and is often seen in women. While the terms “lipedema” and “lipoedema” are used interchangeably in some regions, it’s important to note that in other areas, “lipoedema” may refer to a slightly different condition.
- Lipohypertrophy: Lipohypertrophy is the abnormal enlargement of fat cells in specific areas of the body, often seen in individuals with poorly controlled diabetes who use insulin injections. It differs from lipedema in its distribution pattern and association with diabetes.
- Lipomas: Lipomas are non-cancerous growths of fat cells that can occur anywhere in the body. Unlike lipedema, lipomas do not have a symmetrical or column-like distribution and are usually not associated with tenderness.
Differential Diagnosis
Since lipedema may share similarities with other conditions like lymph edema, Dercum’s disease, and obesity, the healthcare provider will rule out these and other potential causes of the symptoms.
Diagnosis
Diagnosing lipedema involves a combination of medical history, physical examination, and, in some cases, imaging studies. Because lipedema shares some characteristics with other conditions, it’s important for a healthcare professional to rule out other possible causes of symptoms before confirming the diagnosis. Here’s an overview of the diagnostic process for lipedema:
- Medical History: The healthcare provider will start by taking a detailed medical history, including any symptoms experienced, the pattern of fat distribution, the progression of symptoms, and any family history of similar conditions.
- Physical Examination: A thorough physical examination is essential in diagnosing lipedema. The doctor will closely examine the affected areas and look for characteristic signs, such as disproportionate fat accumulation, tenderness, easy bruising, and non-pitting edema.
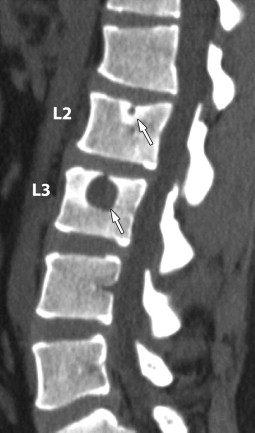
- Imaging Studies: In some cases, imaging studies may be performed to aid in the diagnosis. Ultrasound or magnetic resonance imaging (MRI) can help visualize the distribution of fat, the condition of blood vessels, and the lymphatic system in the affected areas.
- Evaluation of Hands and Feet: An essential aspect of diagnosing lipedema is evaluating whether the hands and feet are spared from fat accumulation. This characteristic sparing is one of the key differentiating features of lipedema from other conditions.
- Evaluation by a Specialist: In cases where the diagnosis is uncertain or complex, consultation with a specialist experienced in the diagnosis and management of lipedema, such as a vascular surgeon or a lymph edema therapist, may be necessary. The diagnosis of lipedema can be challenging due to its similarities with other conditions. It is important for healthcare professionals to consider these potential differential diagnoses to rule them out before confirming lipedema.
Medical Treatment for Lipedema
The medical treatment for lipedema aims to alleviate symptoms, slow disease progression, and improve the overall quality of life for individuals with the condition. While there is no cure for lipedema disease, various approaches can help manage the symptoms effectively. Here are many common medical treatments for lipedema:
- Medications: While there is no medication specifically approved for treating lipedema, some medications may be prescribed to manage associated symptoms. Non-steroidal anti-inflammatory drugs (NSAIDs) may be used to decrease aches and inflammation.
Physiotherapy Treatment
Physiotherapy can play a vital role in the management of lipedema by addressing various aspects of the condition, such as improving mobility, reducing pain, and enhancing overall physical function. Here are some common physiotherapy treatments for lipedema:
Manual Lymphatic Drainage (MLD): MLD is a specialized massage technique that aims to stimulate the lymphatic system and promote the drainage of excess fluid from the affected areas. It can help reduce swelling and edema associated with lipedema and improve lymphatic circulation.
- Compression Therapy: Physiotherapists can provide guidance on using compression outfits effectively. These garments, such as compression stockings or wraps, help support the affected limbs, reduce swelling, and improve overall lymphatic function.
- Decongestive Therapy: Decongestive therapy combines compression therapy, MLD, skin care, and exercise to reduce edema and improve lymphatic circulation. This comprehensive approach can be effective in managing the symptoms of lipedema.
Exercise For Lipedema
Shoulder shrugs
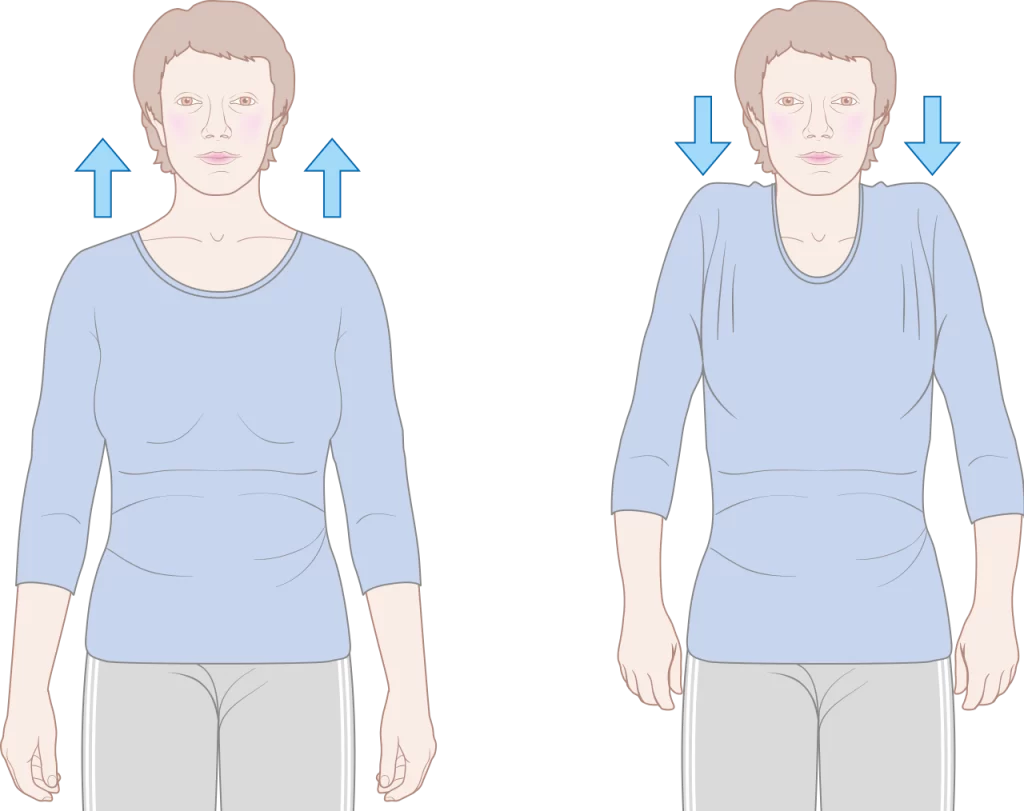
- Stand or sit in a comfortable position. As you inhale, pull both shoulders toward your ears, then exhale, releasing your shoulders to a neutral position. Repeat 10 times.
Neck Rotations

- While sitting, inhale while slowly turning your head to the right for a count of five. Pause for a second, then exhale, bringing your head back to the center for a count of five. Repeat on the other side. Do at least 5 repetitions on both sides.
hip abductions
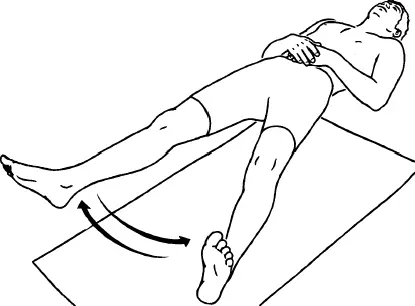
- Lie on your back with your arms against your body and your legs straight out in front of you. Inhale as you slide your right leg across the floor and out to the side. Exhale as you slide your leg back to the center. Repeat on the left side. Do at least 5 repetitions on both sides.
Ankle pumps

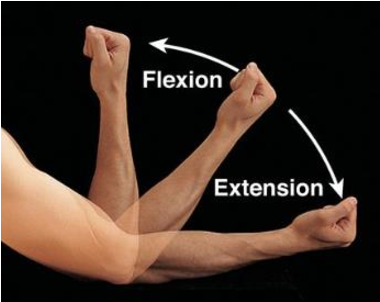
- Lie on your back with your feet and hands on the floor. Inhale and bend the ankle and exhale and extend the ankle 10 times, bending and pointing the toe. Repeat on both sides.
Bend knee fallouts
- Lie on your back area with your knees flexed and feet on the ground. Slowly lower your right knee to the floor, allowing it to open to the side. Slowly raise your leg back to the center and repeat on the other side. Do five times on each side.
Water-Based Exercises
- Exercising in water can be particularly beneficial for individuals with lipedema. Water provides natural compression and buoyancy, which can help reduce swelling and make movement more comfortable. Aquatic exercises, such as water aerobics or swimming, are excellent options.
Flexibility Exercises
- Gentle stretching and range of motion exercises can help maintain joint flexibility and prevent stiffness in the affected areas.
Compression Garments
- Wear properly fitted compression outfits during exercise to provide support to the affected limbs and help manage swelling.
Low-Impact Cardiovascular Exercise
- Engaging in low-impact cardiovascular exercises, such as walking, cycling, or swimming, can help improve cardiovascular fitness without putting excessive stress on the joints. These exercises can also aid in reducing swelling and improving circulation.
Pacing and Rest
- Be mindful of pacing during exercise to avoid overexertion. Take break time as needed and listen to your body parts. normally increase the intensity and duration of exercises over time.
Postural Training
- Correcting posture and teaching proper body mechanics can be beneficial for individuals with lipedema. This can help reduce strain on the lower limbs and improve overall movement patterns.
Lifestyle Modification
- Physiotherapists may provide guidance on lifestyle modifications, such as weight management strategies, diet recommendations, and activity pacing, to help individuals manage their condition effectively.
Pain Management
- Physiotherapists can use some modalities, such as heat or cold therapy, transcutaneous electrical nerve stimulation (TENS), or ultrasound, to help manage pain and discomfort associated with lipedema.
Surgical treatment
Surgical treatment for lipedema is considered when conservative measures, such as compression therapy and lifestyle modifications, have not provided sufficient relief or if there is a need for more significant fat reduction. The main surgical approach for lipedema is liposuction. It’s important to note that surgical intervention is typically reserved for advanced stages of lipedema and should be performed by experienced surgeons with expertise in treating the condition. Here are the surgical treatment options for lipedema:
- Liposuction: Water-assisted liposuction (WAL) or tumescent liposuction are the preferred techniques for lipedema treatment. In WAL, a gentle jet of water is used to dislodge the fat cells, making their removal less traumatic. In tumescent liposuction, a large volume of diluted local anesthesia is infused into the fatty tissue to facilitate the removal of fat cells. Liposuction can effectively reduce the excess fat in the affected areas, providing a more proportionate body contour and improving symptoms.
- Power-Assisted Liposuction (PAL): PAL is a type of liposuction where the surgeon uses a vibrating cannula to break up the fat formerly suctioning it out. This technique may be used in specific cases of lipedema to aid in the removal of fibrotic and dense fat tissue.
- Vibration Amplification of Sound Energy at Resonance Liposuction: VASER liposuction is a specialized liposuction technique that uses ultrasound energy to break down fat cell tissue before removal. It is particularly useful in areas with dense fat cell tissue, like in advanced stages of lipedema.
- Lymphatic Sparing Liposuction: In lipedema surgery, it is essential to avoid damaging the lymphatic vessels as much as possible to prevent worsening lymphatic dysfunction. Lymphatic-sparing liposuction techniques aim to minimize disruption to the lymphatic system during the procedure.
- Post-Surgical Compression Treatment: After liposuction, wearing compression garments is crucial to support the healing process, reduce swelling, and promote skin retraction. Compliance with post-surgical instructions is essential to achieve optimal results.
FAQs
Choose a Healthy Way of Life.
Opt for a Healthy Skincare Routine.
Make Healthy Dietary Changes.
Regular Exercise.
Lifestyle Changes.
Decongestive Therapy and Compression Therapy.
Invasive Therapies.
enlargement of your legs area, and in many cases arms, but usually not your feet or hands.
Affected areas may experience pain, discomfort, heaviness, or tenderness.
affected region of your body can bruise easily, sometimes for no obvious reason.
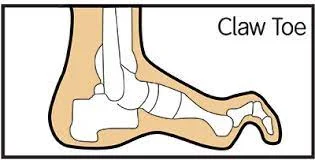
dimpled legs with a lumpy texture, fat may bulge at the knees.
STAGE 1. Smooth skin with an increase of enlarged size of subcutaneous fat tissue. Fat buildup around the pelvis area, buttocks, and hip area.