PAGET’S DISEASE OF BONE
Paget’s disease of bone interferes with your body’s normal recycling process, in which new bone tissue gradually replaces old bone tissue. Over time, the disease can cause affected bones to become fragile and misshapen. Paget’s disease of bone most commonly occurs in the pelvis, skull, spine and legs.
The risk of Paget’s disease of bone increases with age. Your risk also increases if any family members have the disorder. Complications of Paget’s disease of bone can include broken bones, hearing loss and pinched nerves in your spine.
Bisphosphonates — the medications also used to strengthen bones weakened by osteoporosis — are the mainstay of treatment. For patients who have complications, surgery may be necessary.
Table of Contents
The pathogenesis of Paget’s disease
Osteoclastic activity
Mixed osteoclastic – osteoblastic activity
Osteoblastic activity
Malignant degeneration
Initially, there is a marked increase in the rate of bone resorption in localized areas, caused by large and numerous osteoclasts. These localized areas of pathological destruction of bone tissue (osteolysis) are seen radiologically as an advancing lytic wedge in long bones or the skull. When this occurs in the skull, it is called osteoporosis circumscripta. The osteolysis is followed by a compensatory increase in bone formation induced by the bone forming cells, called osteoblasts, that are recruited to the area. This is associated with accelerated deposition of lamellar bone in a disorganized fashion. This intense cellular activity produces a chaotic picture of trabecular bone (“mosaic” pattern), rather than the normal linear lamellar pattern.
The resorbed bone is replaced and the marrow spaces are filled by an excess of fibrous connective tissue with a marked increase in blood vessels, causing the bone to become hypervascular. The bone hypercellularity may then diminish, leaving a dense “pagetic bone,” also known as burned-out Paget’s disease. A later phase of the disease is characterized by the replacement of normal bone marrow with highly vascular fibrous tissue.
Symptoms
Most people who have Paget’s disease of bone have no symptoms. When symptoms occur, the most common complaint is bone pain.
Because this disease causes your body to generate new bone faster than normal, the rapid remodeling produces bone that’s softer and weaker than normal bone, which can lead to bone pain, deformities and fractures.
The disease might affect only one or two areas of your body or might be widespread. Your signs and symptoms, if any, will depend on the affected part of your body.
Pelvis. Paget’s disease of bone in the pelvis can cause hip pain.
Skull. An overgrowth of bone in the skull can cause hearing loss or headaches.
Spine. If your spine is affected, nerve roots can become compressed. This can cause pain, tingling and numbness in an arm or leg.
Leg. As the bones weaken, they may bend — causing you to become bowlegged. Enlarged and misshapen bones in your legs can put extra stress on nearby joints, which may cause osteoarthritis in your knee or hip.
pain
Headache
Muscular
Radicular
Skeletal
Osteoarthritis
Skeletal
Kyphoscoliosis
Bone Bowing (outward bowed femur or forward bowed femur)
Coxa Varus (waddling gait) _Coxa_Valga
Acetabular protrusion
Osteoarthritis
Fractures
Bone enlargement
Vertebral compression
Muscular
Myalgia
Stiffness
Weakness
Neurological
Nerve compression conditions including cranial, spinal, and peripheral nerves
Hearing loss
Mental confusion due to deteriorated cognitive function
Cardiovascular
Heart failure
Increased vascularity (causing increased skin temperature around affected area)
Increased cardiac output
Other
Overall fatigue
Vertigo
Dizziness
Tinnitus
Causes
The cause of Paget’s disease of bone is unknown. Scientists suspect a combination of environmental and genetic factors contribute to the disease. Several genes appear to be linked to getting the disease.
Some scientists believe Paget’s disease of bone is related to a viral infection in your bone cells, but this theory is controversial.
Risk factors
Factors that can increase your risk of Paget’s disease of bone include:
Age. People older than 40 are most likely to develop Paget’s disease of bone.
Sex. Men are more commonly affected than are women.
National origin. Paget’s disease of bone is more common in England, Scotland, central Europe and Greece — as well as countries settled by European immigrants. It’s uncommon in Scandinavia and Asia.
Family history. If you have a relative who has Paget’s disease of bone, you’re more likely to develop the condition.
Complications
In most cases, Paget’s disease of bone progresses slowly. The disease can be managed effectively in nearly all people. Possible complications include:
Fractures and deformities. Affected bones break more easily. Extra blood vessels in these deformed bones cause them to bleed more during repair surgeries. Leg bones can bow, which can affect your ability to walk.
Osteoarthritis. Misshapen bones can increase the amount of stress on nearby joints, which can cause osteoarthritis.
Neurologic problems. When Paget’s disease of bone occurs in an area where nerves pass through the bone, such as the spine and skull, the overgrowth of bone can compress and damage the nerve, causing pain, weakness or tingling in an arm or leg or hearing loss.
Heart failure. Extensive Paget’s disease of bone may force your heart to work harder to pump blood to the affected areas of your body. Sometimes, this increased workload can lead to heart failure.
Bone cancer. Bone cancer occurs in about 1 percent of people with Paget’s disease of bone.
Diagnosis
The first clinical manifestation of Paget’s disease is usually an elevated alkaline phosphatase in the blood.
Paget’s disease may be diagnosed using one or more of the following tests:
Pagetic bone has a characteristic appearance on X-rays. A skeletal survey is therefore indicated.
An elevated level of alkaline phosphatase in the blood in combination with normal calcium, phosphate, and aminotransferase levels in an elderly patient are suggestive of Paget’s disease.
Markers of bone turnover in urine eg. Pyridinoline
Elevated levels of serum and urinary hydroxyproline are also found.
Bone scans are useful in determining the extent and activity of the condition. If a bone scan suggests Paget’s disease, the affected bone(s) should be X-rayed to confirm the diagnosis.
Differential Diagnosis
After obtaining a clinical history and several radiographs and laboratory tests the differential diagnosis can narrowed down to a select few including:
Osteoarthritis
Osteoporosis
Rheumatoid arthritis
Psoriatic arthritis
Ankylosing spondylitis
Diffuse idiopathic skeletal hyperostosis
Pseudogout
Peyronie disease
Bone Metastases
Fibrous Dysplasia
Blastic Metastases
Myelofibrosis
Renal Osteodystrophy
Fluorosis
Mastocytosis
Tuberous Sclerosis
Calvarial Hyperostosis
Many of these conditions may co-exist with Paget’s disease.

Physiotherapy treatment
Pain caused by increased skeletal abnormalities leads to loss of muscle strength, decreased range of motion, and cardiovascular endurance resulting in functional limitations. PhysioTherapy and exercise can assist in maintaining muscle strength, flexibility and joint range of motion, increased endurance, and decrease the chances of deconditioning .
Strengthening muscles around the joints affected and its adjacent joints can help minimize skeletal complications of Paget’s disease .
Improvements in cardiovascular function and cardiac output also can result from physiotherapy improving functional activities such as walking endurance and longer distances .
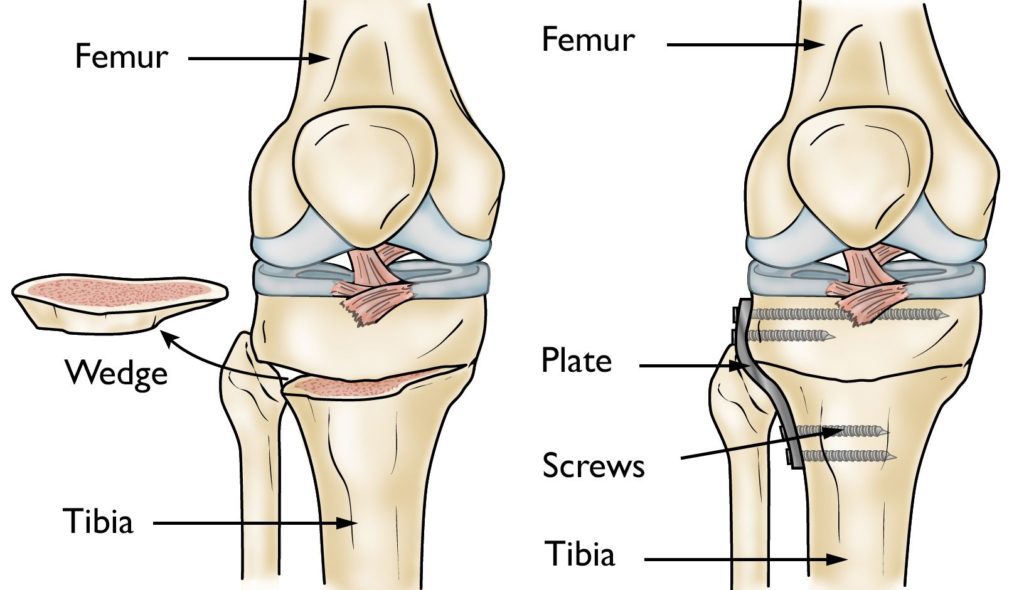
A physiotherapist may also provide orthotics and other assistive devices to help in management of extremity deformities. The physiotherapist can aid in correcting this problem by providing inserts or making appropriate shoe modifications. Bracing may also be beneficial with an open reduction and internal fixation limb surgeries.
Assistive devices for ambulation, such as a cane or walker, can help reduce weight-bearing and pain following these surgeries.
A physiotherapist can also assist a patient with Paget’s disease in home modifications to make the patient safer with mobility around the home.
Modalities can also be beneficial such as superficial heat, transcutaneous electrical nerve stimulation (TENS), and massage, may be helpful for muscle pain, tenderness, and tightness .
Physical therapist should advise precautions, if necessary, for example, avoid activities such as jogging, running, jumping, and aggressive forward bending and twisting exercises, if the spine is affected by Paget’s disease .







3 Comments