Seizures
Table of Contents
What is the condition of seizures?
- A seizure is an unexpected, uncontrolled electrical disturbance in the brain.
- It can cause changes in your behavior, movements, or feelings, and in levels of consciousness.
- Having two or more seizures at least 24 hours apart that are not brought on by an identifiable cause is commonly considered to be epilepsy.
- There are many types of seizures, which range in symptoms & severity.
- Seizure types differ by where in the brain they begin and how far they spread.
- Most of the seizures last from 30 seconds to two minutes.
- A seizure that lasts longer than five minutes is a medically urgent situation.
- Seizures are more usual than you might think.
- Seizures can occur after a stroke, a closed head injury, an infection like meningitis, or another illness.
- Many times, though, the cause of a seizure is unspecified.
- Most seizure disorders can be controlled with medication, yet management of seizures can still have a significant impact on your daily life.
- The good news is that you can work with your doctor to balance seizure control & medication side effects.
What are the types of seizures?
Focal seizures
- Focal seizures result from unusual electrical activity in one area of your brain.
Focal seizures can happen with or without loss of consciousness:
- Focal seizures with impaired awareness.
- These seizures include a change or loss of consciousness or awareness that feels like being in a dream.
- You may seem awake, yet you stare into space & do not respond normally to your environment or you perform repetitive movements.
- These may involve hand rubbing, mouth movements, repeating some words, or walking in circles.
- You may not remember the seizure or even know that it happened.
- Focal seizures without loss of consciousness.
- These seizures may alter emotions or change the way things look, smell, feel, taste or sound, yet you do not lose consciousness.
- You may instantly feel angry, joyful, or sad.
- Some people have nausea or uncommon feelings that are difficult to describe.
- These seizures may also result in difficulty speaking, involuntary jerking of a body part, such as an arm or a leg, & spontaneous sensory symptoms such as tingling, dizziness, and seeing flashing lights.
- Symptoms of focal seizures may be confused with other neurological disorders, like migraine, narcolepsy, or mental illness.
Generalized seizures
- Seizures that seem to involve all areas of the brain are called generalized seizures.
Different types of generalized seizures involve:
Absence seizures:
- Absence seizures, previously known as petit mal seizures, often happen in children and are characterized by staring into space or by subtle body movements, such as eye blinking or lip smacking. They commonly last for five to 10 seconds but may happen up to hundreds of times per day. These seizures may happen in clusters and cause a brief loss of awareness.
- Absence seizures include brief, instant lapses of consciousness.
- They are more usual in children than in adults.
- Someone having an absence seizure may look like he or she is staring blankly into space for some seconds.
- Then, there is a fast return to a normal level of alertness.
- This type of seizure commonly does not lead to physical injury.
- Absence seizures commonly can be controlled with anti-seizure medications.
- Certain children who have them also develop other seizures.
- Many children grow beyond the absence of seizures in their teens.
What are the symptoms of the seizure?
- An indication of a simple absence seizure is an empty stare, which may be mistaken for a lapse in attention that lasts about ten seconds, though it may last as long as twenty seconds, without any confusion, headache, or drowsiness afterward.
Signs and symptoms of absence seizures involve:
- Sudden stop in motion without falling,
- Lip smacking,
- Eyelid flutters,
- Chewing motions,
- Finger rubbing,
- Small movements of both hands.
- Later, there is no memory of the incident.
- Certain people have many episodes daily, which interfere with school or daily activities.
- A child may have absent seizures for a certain time before an adult notices the seizures because they are so brief.
- A decline in a child’s learning ability may be the first sign of this disorder.
- Teachers may comment about a child’s inability to pay attention or that a child is frequently daydreaming.
What are the causes of the seizures?
- Many children appear to have a genetic predisposition to the absence of seizures.
- In common, seizures are caused by abnormal electrical impulses from nerve cells (neurons) in the brain.
- The brain’s nerve cells commonly send electrical and chemical signals across the synapses that connect them.
- In people who have seizures, the brain’s common electrical activity is altered.
- During an absence seizure, these electrical signals repeat themselves over & over in a three-second pattern.
- People who have seizures may also have altered levels of the chemical messengers that assist the nerve cells to communicate with one another (neurotransmitters).
What are the risk factors for seizures?
Certain factors are common to children who have absent seizures, involving:
- Age: Absence seizures are more usual in children between the ages of 4 and 14.
- Sex: Absence seizures are more usual in girls.
- Family members who have seizures: Nearly half of the children with absence seizures have a close relative who has seizures.
What are the complications of seizures?
While most children outgrow absence seizures, certain:
- Must take anti-seizure medications throughout life to cure seizures,
- Eventually have full convulsions, like a generalized tonic-clonic seizure.
Other complications can involve:
- Learning difficulties
- Behavior problems
- Social isolation.
When to see a doctor
Contact your doctor:
- The first time you see a seizure
- If this is a new type of seizure
- If the seizures continue to happen despite taking anti-seizure medication.
Tonic seizures:
- Tonic seizures cause stiffening of your muscles. These seizures commonly affect muscles in your back, arms, and legs and may cause you to lose consciousness and fall to the ground.
What is a tonic seizure?
- Muscle “tone” is the muscle’s usual tension at rest.
- In a tonic seizure, the tone is greatly increased: the body, arms, or legs become instantly stiff or tense.
- A person may be aware or have only less change in awareness during a tonic seizure.
- They usually happen during sleep and commonly involve all or most of the brain, affecting both sides of the body.
- They are short, commonly less than 20 seconds.
- A person may fall down if standing when a tonic seizure starts.
Where does a tonic seizure begin in the brain?
When it starts in one part of the brain:
- Stiffening of a part of the body may begin in one area & stay local.
- These are called focal tonic seizures.
When it starts on both sides of the brain:
- The full body or both sides of the body may become stiff or tense from the beginning.
- These are called generalized tonic seizures.
Who is at risk for tonic seizures?
- Tonic seizures can occur in anyone.
- They are more typical in people who have Lennox-Gastaut syndrome or other syndromes with mixed seizure types.
How can I ask if someone is having one?
- Stiffening or other movements can be seen in other neurological problems, especially in children.
- A written description or video of what occurs during the seizure is very important.
- For example, tonic seizures start instantly with forceful movements.
- Events that start more slowly may be due to another condition.
What happens after a tonic seizure?
- When a tonic seizure ends, the person may or may not be sleepy or confused.
- Commonly, no first aid is needed unless a person is not fully aware during or after the seizure.
- Preventing harm is a key part of first aid for tonic seizures.
- Certain people may need to wear protective equipment like a helmet to prevent head injuries from falls.
If someone has tonic seizures, how often will they occur?
- It depends & varies between people.
- Some people may have just one seizure and others may have tonic seizures that happen often or in clusters of many a day.
How are tonic seizures diagnosed?
- Imaging tests like MRI (magnetic resonance imaging) scans to look for lesions or parts of the brain causing tonic & other types of generalized seizures.
- EEG (electroencephalogram) tests can assist tell the difference between tonic seizures & other symptoms.
How are tonic seizures treated?
- Seizure medicines are an important way of treating & preventing tonic seizures.
- If seizures are not controlled with medications, other options may be possible, like dietary therapies, devices, or even surgery.
- Knowing where a seizure starts and what part of the brain is involved assists you learn what options may be possible.
- If seizures are not controlled, seek out the assistance of an epilepsy specialist or visit an epilepsy center to explore treatment options.
What should I do if I believe my loved one or myself may have tonic seizures?
- If you think that you or your loved one may be having tonic seizures, ask your doctor as soon as possible.
- Getting the correct diagnosis early can assist lead to better treatment.
Atonic seizures:
- Atonic seizures, also known as drop seizures, cause a loss of muscle control, which may cause you to instantly collapse, fall down, or drop your head.

What are the atonic seizures?
- A seizure occurs when electrical activity in the brain surges suddenly.
- Atonic seizures are a type of seizure that causes instant loss of muscle strength.
- These seizures are also called akinetic seizures, drop attacks or drop seizures.
- The instant lack of muscle strength, or tone, can cause the person to fall to the ground.
- The person commonly remains conscious, and may not always fall down.
- Their head may drop, their eyelids may droop, & they may drop anything they were holding.
- These types of seizures frequently begin in childhood and may last into adulthood.
- Sometimes they are linked to other conditions, such as Lennox-Gastaut syndrome.
What are the symptoms of the seizures?
- Atonic seizures result in an instant loss of muscle strength while the seizure is occurring.
Other symptoms may involve:
- Going limp and falling to the ground
- Remaining conscious
- Experiencing a brief loss of consciousness
- Drooping eyelids
- Head nods
- Jerking.
- Because these seizures often result in a fall, the patient may require first aid once the seizure is over.
- Certain people who have these seizures often may choose to wear protective gear, like a helmet.
What are the causes and risk factors of seizures?
- The cause of atonic seizures is frequently unknown.
- Certain patients may be more likely to have seizures because of changes in their genes.
- Atonic seizures most often affect children yet can occur in patients of any age.
- Rapid breathing (hyperventilation) & flickering lights can trigger seizures.
What is the diagnosis of the seizures?
- The most practical test in diagnosing seizures is an electroencephalogram (EEG).
- This records the electrical activity in the brain.
- EEG can show uncommon electrical activity patterns.
- Various types of seizures can be identified with these patterns.
- Magnetic resonance imaging (MRI) & computed tomography (CT) scans may be used to study the condition.
- These images can also show where the seizure is occurring in the brain.
- The scans can also rule out other possible causes like as a stroke.
What is the treatment for seizures?
- Patients may need to wear helmets to cure head injuries during seizures if falling is common.
- Medication is the most usual treatment.
- Anti-seizure (or anti-epileptic) medications can very assist.
- It may take a few tries to find the right drug & the right dose.
- The doctor will monitor for side effects to notice the best option.
These medications involve:
- Ethosuximide (Zarontin) is most frequently used as the first drug treatment.
- Valproic acid (Depakene) is another option.
- It is not recommended for women who are pregnant or want to become pregnant as it can grow the risk of birth defects.
- Lamotrigine (Lamictal) has fewer side effects than the other two medications yet may also be less helpful.
- Clobazam (Onfi).
- Some types of seizures may be controlled with a ketogenic diet.
- This is a high-fat, low-carbohydrate diet used most frequently for children who have not responded to medications.
- A vagus nerve stimulator is sometimes implanted & used along with anti-epileptic medication to reduce seizures.
- The vagus nerve stimulator is a device placed under the skin of the chest that sends electrical energy through the vagus nerve in the neck to the brain.
Clonic seizures:
- Clonic seizures are associated with repeated, rhythmic, jerking muscle movements. These seizures commonly affect the neck, face, and arms on both sides of the body.
What is a clonic seizure?
- “Clonus” (KLOH-us) means fast stiffening and relaxing of a muscle that occurs repeatedly.
- In another word, it is repeated jerking.
- The movements can not be stopped by restraining or repositioning the arms or legs.
- Clonic (KLON-ik) seizures are rare & most commonly happen in babies.
- Most often, clonic movements are shown as part of a tonic-clonic seizure.
- Jerking movements alone, as with a clonic seizure, may last some seconds to a minute.
- Jerking or clonic movements that follow the stiffening of muscles, as in a tonic-clonic seizure, can last seconds to one or two minutes.
- A clonic seizure may occasionally be hard to distinguish from a myoclonic seizure.
- The jerking is more consistent & sustained during a clonic seizure.
Where does a clonic seizure start in the brain?
When it starts in one part of the brain:
- Clonic seizures can start in the motor part on one side of the brain.
- These are called focal clonic seizures.
- The jerking movements would affect just one side or area of the body or face.
When it starts on both parts of the brain:
- Clonic seizures can also affect both parts of the brain at once.
- These would be called generalized clonic seizures.
- The jerking movements would affect both parts of the body or the whole body at once.
Who is at risk for clonic seizures?
- Clonic seizures can affect people of all ages, involving newborns.
- In infants, the clonic seizures are very brief and do not happen very often.
- They may also go away on their own for a less period of time.
- Clonic seizures that do not go away on their own will need long-term treatment.
What is it like to have a clonic seizure?
- Clonic seizures consist of repeated jerking movements of the arms & legs, occasionally on both sides of the body.
- If the clonic seizure has a focal onset (starts in one part of the brain), the person may be conscious during it.
- If the clonic seizure has a generalized onset (affects the whole brain), commonly the person is not aware during it.
- If a person is standing when a clonic seizure happens, they may fall.
- Sometimes a focal clonic seizure affects both the motor & sensory parts of the brain.
- It may also involve tingling or numbness of the body part with the jerking.
What happens after a clonic seizure?
- After a clonic seizure, the person may simply continue what they are doing, especially if they were aware when it occurred.
- If a person was not fully aware, they may need to rest for a few minutes before returning to common activity.
- The most important first aid step is to cure the person from injury when the jerking happens or if they fall.
- Do not try to prevent the person’s movements.
- If a clonic seizure goes into a tonic-clonic one, the person will most likely be tired & confused after the seizure.
- Let them rest as needed & follow care & comfort first aid.
If someone has clonic seizures, how often will they occur?
- The frequency of seizures depends a lot on the cause & the person.
- Certain people may have rare seizures, & others may have them more frequently.
How can I ask if someone is having a clonic seizure?
- Clonic seizures consist of rhythmic jerking movements of the arms and legs, occasionally on both sides of the body, that can be seen by the person observing.
- Occasionally “jitteriness” in a young infant can be mistaken for a clonic seizure, especially if it is serious (during crying, for instance).
- Changing the position of the baby’s arms or legs should decrease or stop jitteriness.
- A jittery infant also will be more aware than an infant who is having a clonic seizure.
- Children with other neurological problems can have repeated jerking that could be mistaken for clonic seizures.
- EEG (electroencephalogram) testing may be needed to see what occurs in the brain when the symptoms occur.
How are clonic seizures diagnosed?
- The best description of the symptoms is the first step.
- Written reports of what occurs from the person having the seizure & from observers can be very helpful.
- Bring the video recordings of events to the doctor’s visit if you have them.
- An electroencephalogram is done to show the electrical activity of the brain.
- Video electroencephalogram telemetry that can record the electrical activity and what it looks like during an event is helpful if seizures don’t respond to treatment.
- This test may also be done to sort out the clonic seizures from other causes.
How are clonic seizures treated?
- Some seizure medicines help prevent clonic seizures.
- Knowing where seizures begin – in one part (focal onset) or both sides (generalized onset) of the brain – will help decide which medicine may be best to use.
What should I do if I think my loved ones or myself may have clonic seizures?
- If you think you or your loved one may be having clonic seizures, ask your doctor as soon as possible.
- Getting these diagnosed early can assist lead to better treatment.
Myoclonic seizures:
- Myoclonic seizures commonly appear as sudden brief jerks or twitches of your arms and legs. There is frequently no loss of consciousness.
What is a myoclonic seizure?
- Myoclonic (MY-o-KLON-ik) seizures are short, shock-like jerks of a muscle or a group of muscles.
- “Myo” means muscle and “clonus” (KLOH-us) means quickly alternating contraction and relaxation—jerking or twitching—of a muscle.
- commonly they do not last more than a second or two.
- There can be just one, yet sometimes many will occur within a short time.
- Even people without epilepsy can experience myoclonus in hiccups or in an unexpected jerk that may wake you up as you are just falling asleep.
- These things are usual.
- In epilepsy, myoclonic seizures commonly cause abnormal movements on both sides of the body at the same time.
They happen in a variety of epilepsy syndromes that have different characteristics:
Juvenile myoclonic epilepsy: The seizures usually include the neck, shoulders, and upper arms. In many patients, the seizures most often happen soon after waking up. They commonly begin around puberty or sometimes in early adulthood in people with a normal range of intelligence. In most cases, these seizures can be well controlled with medication yet they must be continued throughout life.
Lennox-Gastaut syndrome: This is an uncommon syndrome that usually involves other types of seizures as well. It begins in early childhood. Myoclonic seizures usually include the neck, shoulders, upper arms, & often the face. They may be quite strong & are difficult to control.
Progressive myoclonic epilepsy: The rare syndromes in this category feature a combination of myoclonic seizures & tonic-clonic seizures. Treatment is commonly not successful for very long, as the patient deteriorates over time.
Who is at risk for myoclonic seizures?
- The epileptic syndromes that most commonly involve myoclonic seizures usually begin in childhood, but the seizures can occur at any age.
- Other characteristics depend on the particular syndrome.
What happens after a myoclonic seizure?
- When a myoclonic seizure ends, the person commonly continues doing whatever they were doing before and during the seizure.
- They are awake & able to think clearly.
- No first aid is required because of this seizure.
If someone is having a myoclonic seizure, how often will it happen?
- There can be just one, yet sometimes many will occur within a short time.
How can I ask if someone is having a myoclonic seizure?
- These seizures can be easily overlooked because they are so brief & appear as extra-normal movements.
- These seizures can be mistaken for tics, tremors, or clumsiness.
How are myoclonic seizures diagnosed?
- The seizures themselves are easy to identify.
- The syndromes commonly can be diagnosed on the basis of medical history and often an EEG test.
How are myoclonic seizures treated?
- There are several medicines that can assist prevent myoclonic seizures.
- Myoclonic seizures frequently respond well to the appropriate medicine.
What should I do if I believe my child, loved one, or myself may have myoclonic seizures?
- If you think that you or your loved one are having myoclonic seizures, talk to your child’s doctor or your own & share your concerns right away.
- Because myoclonic seizures are often associated with some syndromes, seeing a doctor quickly to make a diagnosis & begin treatment is essential.
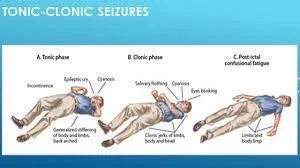
Tonic-clonic seizures:
- Tonic-clonic seizures, before known as grand mal seizures, are the most dramatic type of epileptic seizure and can cause an abrupt loss of consciousness, body stiffening & shaking, & sometimes loss of bladder control or biting your tongue. They may last for some minutes.
- Tonic & clonic seizures affect the muscles.
- Tonic seizures cause a stiffening of muscles periods of clonic seizures are characterized by jerking or twitching.
- Tonic & clonic seizures can start on one part of the brain (partial or focal seizures), or on both sides of the brain simultaneously (generalized).
- Tonic and clonic seizure activity can occur in the same seizure.
- A tonic-clonic seizure is a modern period for a grand mal seizure.
If a character near you has a seizure:
- Do not put anything in the person’s mouth.
- Do not restrain them.
- Make sure the area around the person is clear of objects that could harm them.
- Treatment for tonic & clonic seizures may include medication, nerve stimulation, dietary therapy, surgery, or a combination of these approaches.
- Tonic & Clonic Seizures: Partial or Generalized
- A seizure that originates in both halves (hemispheres) of the brain simultaneously, causing stiffness or twitching over the body, is known as a generalized tonic or clonic seizure.
- A tonic or clonic seizure can also begin in one area of the brain (called a partial or focal seizure), affecting only one portion of the body such as an arm or a leg.
Tonic or clonic seizures can start as partial & become generalized.
Tonic Seizures
- A tonic seizure causes an instant stiffness or tension in the muscles of the arms, legs, or trunk.
- The stiffness lasts about twenty seconds and is most likely to happen during sleep.
- Tonic seizures that happen while the person is standing may cause them to fall.
- After the seizure, the person may feel tired or confused.
- People with Lennox-Gastaut syndrome or other types of epilepsy with mixed seizures are most likely to have tonic seizures, yet they can happen to anyone.
Clonic Seizures
- Clonic seizures are characterized by repeated jerking movements of the arms and legs on one or both sides of the body, occasionally with numbness or tingling.
- If it is a focal (partial) seizure, the person may be aware of what’s occurring.
- During the generalized seizure, the person may be unconscious.
- Clonic seizures can happen in people of all ages, including newborns and infants.
What to Do When Someone Has a Seizure?
- First aid for a person having a tonic or clonic seizure includes protecting the person from injury, such as moving furniture or other items out of the way.
- It is important not to attempt to restrain the person or put anything in their mouth — “swallowing the tongue” is impossible.
- Later, the person is likely to be tired, embarrassed, or confused.
- Offer supportive care & reassurance.
- 1st-time seizures should be evaluated by a doctor.
Diagnosis & Treatment of Tonic & Clonic Seizures
- Creating a written report by describing the details of the seizure can be assisted when the patient or parent sees the doctor.
- A video of the seizure taking place, if available, can assist the doctor make a diagnosis.
- To diagnose tonic & clonic seizures, the physician is likely to use imaging tests like magnetic resonance imaging (MRI) to look for scarred areas in the brain, as well as electroencephalography (EEG) to assist differentiate seizures from other problems.
- Tonic & clonic seizures, like other seizures and seizure disorders, need an individualized approach.
- The doctor may commend treatment with anti-seizure medication, nerve stimulation, dietary therapy, or surgery.
What are the Symptoms of the seizures?
Seizures can have different symptoms depending on the type of seizure, yet may involve:
- Uncontrollable, spastic movements of your body parts, particularly your arms or legs
- Stiffening & then loosening of the limbs or muscles
- Loss of consciousness
- Staring into space
- Confusion
- Sudden emotional states that can involve a feeling of doom, deja vu, fear, or euphoria
- Sweating & nausea
- Involuntary movements of your tongue or mouth, such as screaming, or crying
- Rapid blinking
- Falling to the ground.
What are the Causes of the seizures?
Seizures can occur with no explanation, but there are also conditions and events that can bring them on, involving:
- Stroke
- Cancer
- Brain tumors
- Head injuries
- Electrolyte imbalance
- Very low blood sugar
- Repetitive sounds or flashing lights, like in video games
- Some medications, like antipsychotics and certain asthma drugs
- Withdrawal from certain medications, like Xanax, narcotics, or alcohol
- Use of narcotics, such as cocaine and heroin
- Brain infections, like meningitis
- A high fever
- COVID-19
What are the effects of seizures?
- Living with epilepsy and experiencing repeated seizures can have both short & long-term effects.
- These can range from a drop in quality of life to increased risks of mental health conditions.
Short-term effects
- Certain seizures can cause you to lose total control of your body.
- This can lead to falls & other movements that can result in injury.
- People with epilepsy typically have more than Trusted Source physical issues, like as bruising and fractures, than people without the condition.
- Being prone to seizures may also affect your quality of life.
- For example, you may no longer be able to drive.
- You may want to avoid situations where a seizure could cause serious harm, like swimming or traveling alone.
- It is important to wear a medical identification bracelet that tells emergency responders that you have epilepsy.
Long-term effects
- If you do not get treatment for seizures, their symptoms can become worse and progressively last longer.
- Prolonged seizures can lead to coma or death.
- While death as a direct result of seizures is rare, the risk of premature death in people with epilepsy is up to three times higher than Trusted Source than in the general populace.
- Living with epilepsy & seizures can also have an impact on your mental health.
- People with epilepsy have a higher rate of Trusted sources of bipolar disorder & depression than people without the condition.
How are seizures diagnosed?
- Doctors can have a different time diagnosing seizure types.
- Your doctor may recommend specific tests to accurately diagnose a seizure and assist ensure that the treatments they recommend will be effective.
- Your doctor will consider your complete medical history & the events leading up to the seizure.
- For example, migraine, headaches, sleep disorders, & extreme psychological stress can cause seizure-like symptoms.
- Lab tests may assist your doctor rule out other conditions that can cause seizure-like activity.
The tests may include:
- blood testing to check for electrolyte imbalances,
- a spinal tap to rule out the infection,
- a toxicology screening to test for drugs, poisons, or toxins,
- An electroencephalogram (EEG) can assist your doctor to diagnose a seizure.
- This test measures your brain waves.
- Viewing brain waves during a seizure can assist your doctor in diagnosing the type of seizure.
- Imaging scans such as a CT scan or MRI scan can also assist by providing a clear picture of the brain.
- These scans allow your doctor to look for abnormalities like blocked blood flow or a tumor.
Seizures vs Epilepsy
| No | Seizure | Epilepsy |
| 1. Definition | A seizure is a single occurrence of a jerky movement and other features of a fit. | Epilepsy is two or more two unprovoked seizures occurring in an individual. |
| 2. Incidence | Approximately 80/1,00,000 per year | Approximately 45/1,00,000 per year |
| 3. Prevalence | Lifetime prevalence – 9% | Point prevalence – 0.5-1% The cumulative risk of epilepsy: 1.3% – 3.1% |
| 4. Causes | multiple causes including brain tumor, brain injury, internal injury, epilepsy, drug, and alcohol withdrawal | Multiple causes include brain tumor, brain injury, internal injury, drug and alcohol withdrawal, brain bleeding, mental trauma |
| 5. Diagnosis | Neurological exam, EEG test, CT or MRI, and blood test | Neurological exam, physical exam, EEG, ECG, MRI, CT, and blood test |
| 6. Treatment | Do not need any treatment with anti-epileptic drugs or surgery | Anti-epileptic drugs are used and non-responding patients might need surgery |
How are seizures treated?
- Treatments for seizures depend on the cause.
- By treating the cause of the seizures, you may be able to cure future seizures from occurring.
- The treatment for seizures due to epilepsy involves:
Medications
- Anti-epileptic drugs are sometimes the first treatment option for people experiencing multiple seizures.
- They target the signaling activities in specific brain cells and can effectively control seizures in approximately seventy percent of cases.
- There are many types of anti-epileptic drugs.
- You and your doctor may have to work to find out which is the best medication for treating your condition.
Brain surgery
- Doctors may recommend surgical options for treating epilepsy & seizures if medications do not work.
Surgical procedures to treat epilepsy involve:
- respective surgery,
- multiple subpial transections,
- hemispherectomy,
- corpus callosotomy,
- Brain surgery for epilepsy can improve quality of life but does carry a risk of complications. Consult with your doctor to discuss whether surgery is the right decision for you.
Nerve stimulation
- In addition to brain surgery, surgeons can insert nerve stimulation devices into the body to treat epilepsy.
- Vagus nerve stimulation includes placing electrodes around the vagus nerve in your neck and a generator for these electrodes in the upper chest.
- These devices then stimulate the nerve with electrical signals, which can assist manage seizures.
- Responsive neurostimulation systems work by stimulating the brain to manage seizures. Doctors can program these devices to assess and respond to nerve activity associated with seizures, sometimes stopping them.
- These less invasive surgical options can assist in safely reducing seizure frequency and severity.
- Doctors may also suggest deep brain stimulation therapy.
- This is where a surgeon places the electrodes onto the thalamus.
- The thalamus is a part of the brain that processes signals from almost each and every sensory system.
- It regulates consciousness, alertness, & sleep cycles.
- Electrical signals from these electrodes assist regulate the excitability of certain parts of the brain.
- This can help reduce the frequency of seizures.
How can you prevent seizures?
- In many instances, a seizure is not preventable.
- Yet maintaining a healthy lifestyle can give you the best chance of reducing your risk.
You can do the following:
- Get plenty of sleep.
- Eat a balanced diet & drink plenty of fluids.
- Exercise regularly.
- Engage in stress-reducing techniques.
- Do not take illegal substances.
- If you are on medication for epilepsy or other medical conditions, take them as your doctor recommends.
FAQ
What are the main causes of seizures?
Seizures of all types are caused by unusual electrical activity in the brain.
Causes of seizures can involve abnormal levels of sodium or glucose in the blood.
Brain infection, including meningitis & encephalitis.What are the 4 types of seizures?
There are four important types of epilepsy: focal, generalized, combination focal and generalized, and unknown.
A doctor commonly diagnoses someone with epilepsy if they have had two or more unprovoked seizures.
Medication is the most usual treatment, and two-thirds of adults with epilepsy live seizure-free because of it.What happens during seizures?
A seizure is a medical condition where you have a temporary, unconstrained surge of electrical activity in your brain.
When that occurs, the affected brain cells uncontrollably fire signals to others around them.
This out-of-control electrical activity overloads the affected parts of your brain.How long does a seizure last?
Most of the seizures last from thirty seconds to 2 minutes.
A seizure that lasts longer than 5 minutes is a medical crisis.
Seizures are more usual than you might think.
Seizures can occur after a stroke, a closed head injury, an infection like meningitis, or another illness.How do you stop a seizure from happening?
First Aid
1. Stay other people out of the way.
2. Clear hard or sharp objects apart from the person.
3. Do not try to hold them down or stop the movements.
4. Place them on their side, to assist keep their airway clear.
5. Look at your watch at the beginning of the seizure, to time its length.
6. Do not put anything in their mouth.




29 Comments