Juvenile Myoclonic Epilepsy (JME)
Table of Contents
What Is Juvenile Myoclonic Epilepsy?
- Juvenile myoclonic epilepsy (JME) is a type of epilepsy that begins in childhood or the teen years.
- People who have it wake up from rest with quick, jerking movements of their arms and legs. These are called myoclonic jerks.
- Even if you do not have epilepsy, you have probably had these jerks that jolt you awake, often when you are just about to fall asleep.
- But people with JME commonly have other types of seizures as well.
- After the age of thirty, the seizures tend to get better.
- And medications can remain JME under control.
- Yet most people with the condition will need to take the medicine for the rest of their lives, even if they end up having seizures.
What Are the Signs and Symptoms of a Juvenile Myoclonic Seizure?
- Various types of seizures can occur in juvenile myoclonic (my-uh-KLON-ik) epilepsy.
- The first seizures commonly start between the ages of 5 and 16.
People with JME have three various types and their symptoms are:
Myoclonic Seizures
- This kind of seizure is the most usual type in juvenile myoclonic epilepsy and is the hallmark of this condition.
In a myoclonic seizure, a child:
- has short muscle twitches or jerks in the upper arms, shoulders, or neck
- has movements on one or both sides of the body at the very same time
- commonly is awake and can think clearly during and right after the seizure
- The jerking movements in one or both arms and legs — typically start from one to 9 years later, around age 14 or 15.
- Certain kids will only have irregular movements in their fingers.
- This may make them drop things and seems clumsy.
Absence Seizures
- An absence seizure begins suddenly in the middle of an activity and ends abruptly.
During the seizure, a child:
- blanks out or has staring spells that last 5 to 20 seconds,
- may flutter their eyes or look upward,
- is unconscious of what is going on during the seizure,
- returns to normal activity and won’t remember having the seizure after it is over,
- has lip-smacking, chewing movements, and fumbling movements in their hand.
- Absence seizures are commonly the first kind that a child with JME will have.
- They might seem to be daydreaming or zoning out for ten seconds or so during these episodes.
- So you might not even notice when they occur.
Tonic-Clonic Seizures
In this type of seizure, a child:
- has convulsions, or rigid muscles & rhythmic body jerks
- rolls the eyes back
- cries out
- may pee or poop
- can’t respond during seizures
- is confused and sleepy after the seizure
- Seizures in juvenile myoclonic epilepsy typically occur within 30 minutes of waking up in the morning or after a nap.
- They are more likely to happen when someone is tired, stressed, or did not get enough sleep.
- Tonic-clonic seizures usually, start a few months later.
- During these seizures, the muscles all over the child’s body will get stiff & jerk rhythmically.
- They will pass out and may fall to the floor.
- They usually last for 1 to 3 minutes.
- Seizures often occur within 30 minutes to an hour of waking up in the morning or after a nap.
- A cluster of myoclonic jerks may be a warning symptom that a tonic-clonic seizure is coming.
- About 1 in 6 people with JME only have myoclonic jerks and do not have other kinds of seizures.
JME in adults
- Juvenile myoclonic epilepsy is a condition characterized by reoccurring seizures (epilepsy).
- This condition starts in childhood or adolescence, usually between ages 12 and 18, and lasts into adulthood.
- The most usual type of seizure in people with this condition is myoclonic seizures, which cause rapid, uncontrolled muscle jerks.
- People with this condition may have generalized tonic-clonic seizures (also known as grand mal seizures), which cause muscle rigidity, convulsions, and loss of consciousness.
- Sometimes, affected individuals have absence seizures, which cause loss of consciousness for a less period that appear as a staring spell.
- Typically, people with juvenile myoclonic epilepsy develop the characteristic myoclonic seizures in adolescence, then develop generalized tonic-clonic seizures some years later.
- Although seizures can occur at any time, they occur most commonly in the morning, shortly after awakening.
- Seizures can be triggered by a loss of sleep, extreme tiredness, stress, or alcohol consumption.
- Juvenile myoclonic epilepsy harms an estimated 1 in 1,000 people worldwide.
- Approximately five percent of people with epilepsy have juvenile myoclonic epilepsy.
What Causes JME?
- Doctors do not know exactly why some people get JME.
- Yet it may be tied to genes that run in your family.
- About one-third of those with the state have a relative who has seizures.
- It is clear that certain things tend to bring on seizures, though.
- The most common triggers are lack of rest and too much stress.
- Drinking alcohol, which can lead to too little rest and fatigue, is the strongest trigger of myoclonic jerks and tonic-clonic seizures.
- Flickering lights can also trigger seizures for certain people.
- It might occur while watching TV, playing video games, or being outside as light flickers through trees or off waves or snow.
- Certain girls and women get seizures during their periods, too.
What can trigger seizures in people with JME?
- One of the most interesting aspects of juvenile myoclonic epilepsy is that there are two very usual factors that cause seizures: lack of sleep and stress.
- Lack of sleep and fatigue, primarily after drinking too much alcohol, are the most important powerful causes of myoclonic jerks and generalized tonic-clonic seizures in JME.
- Mental and emotional stress are also usual triggers, especially excitement or frustration.
- Certain people with JME have seizures that are triggered by flickering light, such as strobe lights at dances, TV, video games, or light shining through trees or reflecting off ocean waves or snow.
- These are called photosensitive seizures.
Is JME inherited?
- Juvenile myoclonic epilepsy is genetically determined.
- However, most people with Juvenile myoclonic epilepsy do not have abnormal results on testing for specific epilepsy genes.
- About 1/2 (50 to 60%) of families with juvenile myoclonic epilepsy report seizures in either a direct relative or a cousin.
- The inheritance pattern is a complex type, although there are some subtypes with distinct genetic patterns.
How is JME diagnosed?
- Doctors diagnose Juvenile myoclonic epilepsy with an electroencephalogram (EEG), a test that can find unusual patterns in brain waves.
- You’ll have the test while you are asleep and awake.
- To do the check, your medical team places electrodes on your scalp.
- They are connected with wires to a computer that shows the electrical activity of your brain cells.
- The results seem like a graph of spikes and wavy lines.
- Your doctor will scan them to look for patterns that signal Juvenile myoclonic epilepsy.
- Your doctor may also want to do imaging tests of your brain, such as magnetic resonance imaging (MRI) and a computed tomography (CT) scan, to see if there is anything else that could be causing your seizures.
EEG and Sleep-deprived EEG
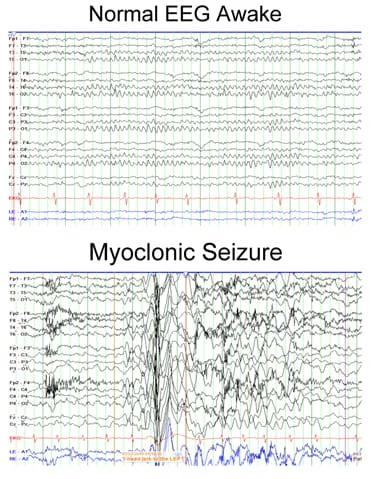
- An Electroencephalography is a brain wave test that detects seizure activity in the brain. Myoclonus is considered a seizure when it is accompanied by Electroencephalography changes.
- A sleep-deprived Electroencephalography is particularly helpful for myoclonic seizures.
- This is because seizures often happen right before or after sleep, and sleep patterns are known to affect seizure activity.
- With JME, the test may show a specific pattern during seizures called ictal Electroencephalography.
- Another pattern, called interictal Electroencephalography, will appear between seizures.
- There are specific Electroencephelography patterns for other types of myoclonic epilepsy and the related syndromes.
- For example, LGS has an interictal steady spike and wave pattern.
How is Juvenile myoclonic epilepsy (JME) treated?
- The treatment of juvenile myoclonic epilepsy begins with educating people about lifestyle and avoidance of seizure triggers.
- Avoiding sleep deprivation is essential. People with juvenile myoclonic epilepsy should make sure they get adequate rest and have appropriate outlets for emotions and stress to lessen the potential for seizures.
Non-pharmacological treatment
- In JME, reduce of sleep and alcohol intake can induce seizures.
- The sleep-wake rhythm has to be regulated.
- The circumstances interfering with normal rest and progressive awakening in the morning should be eliminated.
- If the patient stays up late at night, he should rest longer the next morning.
- Alcoholic drinks will only be permitted in fewer quantities, on social occasions.
- Patients should be advised not to drink in cases of less sleep.
- If the patient has photosensitivity, they should keep away relevant visual stimuli.
- Certain maneuvers reduce the risk of photosensitive seizures, including monocular complete occlusion, increased distance from a video-display terminal, and the provision of ambient back lighting (Harding and Jeavons 1992).
- We suggest these approaches to patients who show photosensitivity on Electroencephalography but do not know how successful these environmental alterations are in Juvenile myoclonic epilepsy.
- It is highly advised that people keep away from drinking alcohol.
Pharmacological treatment
- Most people with Juvenile myoclonic epilepsy will also need one or more anti-seizure medications.
- They can sway seizures in 90% of people with the condition.
These medicines involve:
- Valproic acid
- Lamotrigine
- Clonazepam
- Levetiracetam
- Valproic acid is the most useful seizure medication to treat juvenile myoclonic epilepsy. However, it is not the appropriate 1st choice to treat women in their childbearing years.
- Lamotrigine is broadly used for juvenile myoclonic epilepsy.
- Infrequently, it may lead to worsening of the myoclonic jerks even though it may assist the generalized convulsions & absence of seizures.
- Levetiracetam is another possible drug choice.
- It has been accepted for treating myoclonic seizures in juvenile myoclonic epilepsy.
- However, it has not been effectively studied for all the seizure types that may be seen.
- Other possible options involve topiramate, zonisamide, or clonazepam.
- Clonazepam given in little doses could be effective for myoclonic jerks.
- Medications that should be avoided involve vigabatrin, tiagabine, gabapentin, pregabalin, phenytoin, oxcarbazepine, and carbamazepine, as these can worsen seizures, especially myoclonic jerks and absences in juvenile myoclonic epilepsy.
- Sometimes, carbamazepine and phenytoin may be useful for generalized convulsions.
- If seizures are not controlled, look for specialized care to determine if seizures are properly diagnosed and explore all treatment options.
What is the outlook for people with JME?
- Seizures in most people with juvenile myoclonic epilepsy tend to improve after the fourth decade of life.
- Seizures are commonly well controlled with medications in up to 90% of people.
- People who have many seizure types may require more medications to control them.
- It is likely that lifelong treatment with a seizure drug will be necessary, even in people with well-controlled juvenile myoclonic epilepsy.
- Withdrawal could result in a relapse of seizures, even in people who have been seizure free for multiple years with appropriate drugs.
- In certain people with mild forms of the condition, the dose of seizure medication may be reduced slowly over months, particularly in older individuals.
- If myoclonic seizures come back or persist, medications require to be restarted.
FAQ
What triggers juvenile myoclonic epilepsy?
The most usual triggers are lack of sleep and too much stress.
Drinking alcohol, which can conduct to too little sleep and fatigue, is the strongest trigger of myoclonic jerks and tonic-clonic seizures.
Flickering lights can also trigger seizures for certain people.Does juvenile myoclonic epilepsy go away?
Juvenile Myoclonic Epilepsy Treatment
Most patients with JME do not outgrow their seizures and will require to take medication for the rest of their lives.
Individuals are encouraged to get enough sleep and avoid alcohol to lessen the likelihood of seizures.What are the symptoms of juvenile myoclonic epilepsy?
Seizures in juvenile myoclonic epilepsy typically happen within thirty minutes of waking up in the morning or after a nap.
…
Tonic-Clonic Seizures
has convulsions, rigid muscles, and rhythmic body jerks.
rolls the eyes back.
cries out.
may pee or poop.
can’t respond during the seizure.
is confused and sleepy after the seizure.What type of epilepsy is juvenile myoclonic?
Juvenile myoclonic epilepsy (JME) is the most usual generalized epilepsy syndrome.
It is also called Juvenile Myoclonic Epilepsy of Janz.
It usually is 1st seen in adolescence.
Less usually, it can develop in a child who has had childhood absence epilepsy.Do myoclonic seizures cause brain damage?
This is a very type of epilepsy that worsens over time.
It usually includes brain deterioration or damage that also affects memory, muscle control, thinking ability, and more.
Certain forms of this are eventually fatal.