Hepatitis C
Table of Contents
What is Hepatitis C?
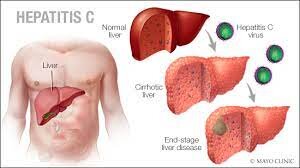
Hepatitis C is a viral infection that harms the liver. It causes inflammation and swelling, which damages the liver tissues over time. “Hepatitis” means inflammation of the liver. There are too many different causes of hepatitis, and some of them are viruses. As compared to other causes of viral hepatitis, though, hepatitis C is much more likely to stay in the body for a long time.
Chronic inflammation over many years does serious harm to the liver. In fact, hepatitis C is one of the main causes of liver failure and liver transplantation in the United States. Most individuals can not tell when their liver is inflamed. They do not develop symptoms until severe damage has already been done.
How common is Hepatitis C?
- Rates of hepatitis C infection in the U.S. have nearly fourfold in the last 10 years.
- According to the Centers for Disease Control and Prevention, nearly four million people in the United States today can have hepatitis C. Many are unaware.
- The CDC now suggests that all U.S. adults be screened for hepatitis C. Globally, the estimated number of infections is 60 million.
What is the main cause of Hepatitis C?
- Hepatitis C is caused by a virus that outspread through contact with blood.
- Infection virus Transmission occurs when the blood of an infected person enters the body of an uninfected person.
- In the U.S., it most usually happens when individuals share needles for injecting intravenous drugs.
- Worldwide, transmission generally happens in medical settings with unsterilized equipment.
How does hepatitis C infection affect a person?
Hepatitis C infection has too many different stages.
Incubation
- When a person first gets a virus, it goes through what is called an incubation period.
- This is when it is busy replicating itself in the body.
- The virus keeps reproducing until it reaches the threshold where the body identifies the infection.
- Then the immune system kicks in, and that is when a person starts to notice symptoms.
Acute infection
- With hepatitis C, the incubation period can last from 2 weeks to 6 months.
- The acute stage of infection starts when the immune system kicks in.
- It is also when a person starts to experience symptoms.
- Most viral infections at the initial stage cause symptoms of illness, like fever and inflammation in the body.
- With hepatitis, though, the inflammation is mainly in the liver, and a person might not notice it.
- Only 20% of individuals with acute hepatitis C infection have symptoms.
- Individuals who have symptoms may treat the infection with antivirals.
- But most do not have symptoms and do not know to seek treatment.
- The acute stage lasts up to 3 months.
- Within this period, up to 20% of individuals effectively fight off the virus and spontaneously clear it from their bodies.
Chronic infection
- Most individuals (80%) are not able to clear the virus by themselves and develop a long-term, chronic infection.
- This means that their livers are continuously inflamed and swollen.
- Chronic hepatitis causes liver injury by a process identified as cirrhosis.
- The continuous inflammation of the liver eventually leads to scarring.
- Cirrhosis progresses gradually over several decades.
- It might go faster if a person has additional liver damage from other causes, like excessive alcohol use.
- It might go slower if the liver is in better condition overall.
- But the end result is that scar tissue prevents the liver from doing its job.
- The risk of cirrhosis from chronic hepatitis C infection is about twenty-five after twenty years.
Other Causes
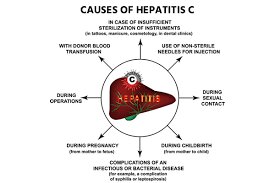
- The hepatitis C virus (HCV) outspreads through contact with blood.
- Transmission takes place when the blood of infected individuals enters the body of an uninfected person.
- In the U.S., the most usual way this takes place is by sharing needles for injecting intravenous drugs.
- But there are all sorts of accidental ways that a person might come into contact with another person’s blood.
For example:
- Exposure to needles or sharp objects at work, specifically in healthcare.
- Tattoos or body piercings are done with unsterilized equipment.
- Sharing a razor or toothbrush with some people who might have bled using it.
- List common, sexual contact that leads to blood exposure.
- Before 1992, hepatitis C was usually spread through blood transfusions and organ transplants.
- Now, doctors regularly screen for the virus before using donated blood or organs.
- While it is no longer a risk from these causes, doctors suggested that everyone who did receive a transfusion or transplant before 1992 get tested for HCV.
Who is most usually affected by hepatitis C infection?
The persons are more likely to be infected with hepatitis C if you:
- Use intravenous drugs.
- Have HIV.
- Obtain a blood transfusion or organ transplant before 1992.
- Obtain blood clotting factor for hemophilia before 1987.
- Were born between 1945 and 1965.
- Were born to a mother with hepatitis C.
What are the symptoms of hepatitis C?
- Most individuals do not have any symptoms.
- A small number can have symptoms at the time of the acute stage of infection.
- They may be indefinite, flu-like symptoms, or they may be like the symptoms of liver disease, involving stomach pain and jaundice.
- Much later on, a person can start to notice symptoms of late-stage liver disease when the liver is beginning to fail.
What are the primary warning signs of hepatitis C?
Acute symptoms of hepatitis C infection can resemble flu symptoms, like:
- Fever.
- Fatigue.
- Body aches.
- Loss of appetite.

They can also look like the symptoms of acute liver failure, such as:
- Jaundice (yellowing of lighter skin and the whites of the eyes).
- Abdominal pain (specifically in the upper right quadrant).
- Nausea and vomiting.
- Dark-colored pee and light-colored poop.
What are the symptoms of advanced liver disease?
If a person does not have early warning symptoms, a person can have late warning symptoms of hepatitis when they begin to experience the effects of cirrhosis after too many years of chronic infection. A person can have all of the symptoms above, and may also notice:
- Swelling with fluid in the arms and legs (edema).
- Swelling with fluid in the abdomen (ascites).
- Itchy skin.
- Unexplained weight loss.
- Easy bruising and bleeding.
- Difficulty thinking or remembering, confusion (hepatic encephalopathy).
How is hepatitis C diagnosed?
- Screening for hepatitis C infection starts with a normal blood test.
- The lab technician will draw a small amount of blood from a vein in the arm and send it to the lab for testing.
- If a person has been infected with the virus, the blood sample will have antibodies against hepatitis C.
- If a person tests positive for antibodies, the doctor will follow up with some extra blood tests.
- A blood test called an RNA PCR test looks for proof of the actual virus in your blood, not just the antibodies.
- This test is important to confirm that persons are still infected.
- A person might still have antibodies even if the person has spontaneously cleared the virus.
- The doctor may also use this test to measure the quantity of the virus in the blood and to rule out which strain a person has.
Other tests
It may include:
Liver function tests
- Liver function tests are a series of blood tests that evaluate the health of the liver.
Elastography
- An elastography is a noninvasive imaging test that measures the stiffness or fibrosis of the liver tissue. It uses ultrasound or MRI.
Liver biopsy
- As a last resort, when other tests are not conclusive, a doctor can take a sample of tissue from the liver to test in the lab.
- They may generally, do this through a hollow needle inserted through the abdominal wall in a simple bedside procedure.
Treatment of Hepatitis C
- It does not generally go away without treatment, but occasionally it does.
- If persons are among the few who are able to spontaneously clear the virus, this will take place at the time of the acute stage of infection.
- The acute stage is when the immune system launches its first attack on the virus. It lasts up to 3 months.
- If it succeeds, a person won’t develop a chronic infection.
- If a person does have a chronic infection, it means that the virus has outwitted the immune system and the person will need help to clear it.
- Luckily, recent advances in antiviral medications have made this possible.
- New antivirals can rehabilitate chronic hepatitis C infection in 95–98% of cases, within eight to 24 weeks.
- Due to their side effects, they can not be suitable for every individual.
What is the treatment for Hepatitis C?
There are too many different medications now available to treat hepatitis C. Different medications are suggested to treat different strains of the virus. The length of treatment can be based on the overall condition and the strain (or genotype) persons have. Some respond to better treatment than others.
Medications approved for the rehabilitation of hepatitis C include:
- Sofosbuvir (Sovaldi®).
- Ledipasvir/sofosbuvir (Harvoni®).
- Simeprevir (Olysio®).
- Paritaprevir/ombitasvir/ritonavir/dasabuvir (Viekira Pak®).
- Daclatasvir (Daklinza®).
- Elbasvir/grazoprevir (Zepatier®).
- Sofosbuvir/velpatasvir (Epclusa®).
- Glecaprevir/pibrentasvir (Mavyret®).
- Sofosbuvir/velpatasvir/voxilaprevir (Vosevi®).
- Ombitasvir/paritaprevir/ritonavir (Technivie®).
- Ribavirin (RibaPak®).
- Peginterferon alfa-2a/2b (Pegasys®/PEG-Intron®).
Will a person need additional treatment?
- If a person already has advanced liver disease (cirrhosis), curing the infection can not be enough.
- A person can already be on the threshold of liver failure.
- The only cure for liver failure is liver transplantation.
- If a doctor determines that a person requires a new liver, a person will have to join the waiting list.
- In the meantime, curing hepatitis C is still necessary to protect the health of your new liver.
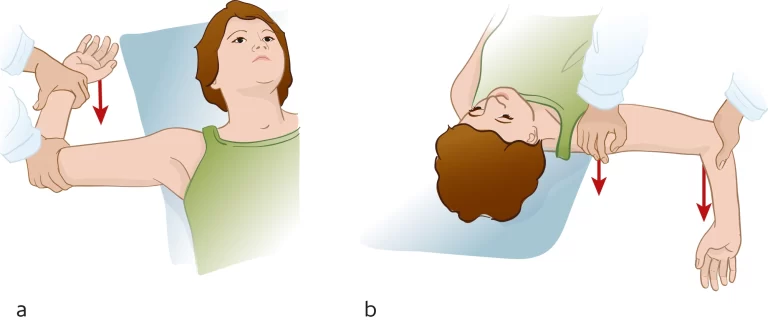
Physiotherapy treatment
- During physical activity, it is necessary to monitor the patient for signs and symptoms of fatigue.
- As for Hepatitis A bed rest is the best form of treatment and being aware of the acuteness of the Hepatitis infection is crucial when screening for physical therapy.
- Supportive therapy and patient education are used to make sure the patient is comfortable and has a sufficient nutritional balance for all three infections.
- It is also important to remind the patient to abstain from the use of alcohol or intake of fatty substances.
- More and more physicians are identifying the value of exercise for liver patients as exercise causes improvements in quality of life and better prognoses.
The below-given liver benefits have been shown in studies to be associated with regular exercise:
Decreased risk of scarring and cirrhosis in Hepatitis C –
- Regular exercise decreases the incidence of obesity in HCV patients.
- Studies show that avoiding obesity helps prevent the resulting conditions – fatty liver, elevated blood glucose, diabetes, and elevated blood insulin – That lead to scarring and cirrhosis.
Hoisted mood –
- Depression is the most usual problem among people suffering from chronic liver disease.
Improve blood oxygenation –
- The cardiovascular benefits of daily exercise enhance the oxygen-carrying capability of the blood thus more oxygen is delivered to the liver, which creates a higher-functioning liver.
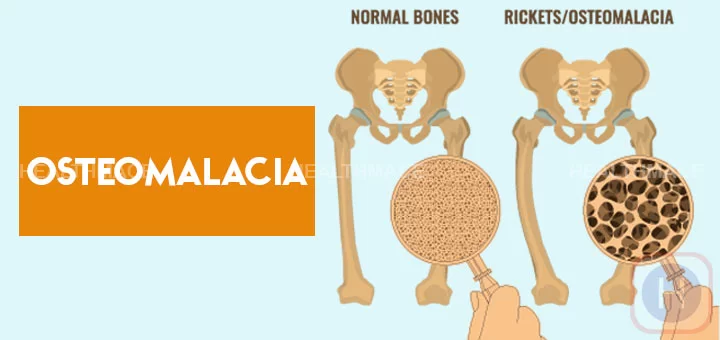
Reduced atrophy –
- Strength training supports muscle growth and maintenance which may avert or delay the severe muscle wasting seen in advanced liver disease.
Improved energy –
- Over time, regular exercise improves the efficiency of the Cardiovascular System.
- This inverse transportation of oxygen and nutrients to all cells, tissues, organs, and systems, leads to a higher energy level.
Exercise program
- It incorporates aerobic/cardiovascular conditioning and strength training to have a major effect on liver function.
Aerobic exercises
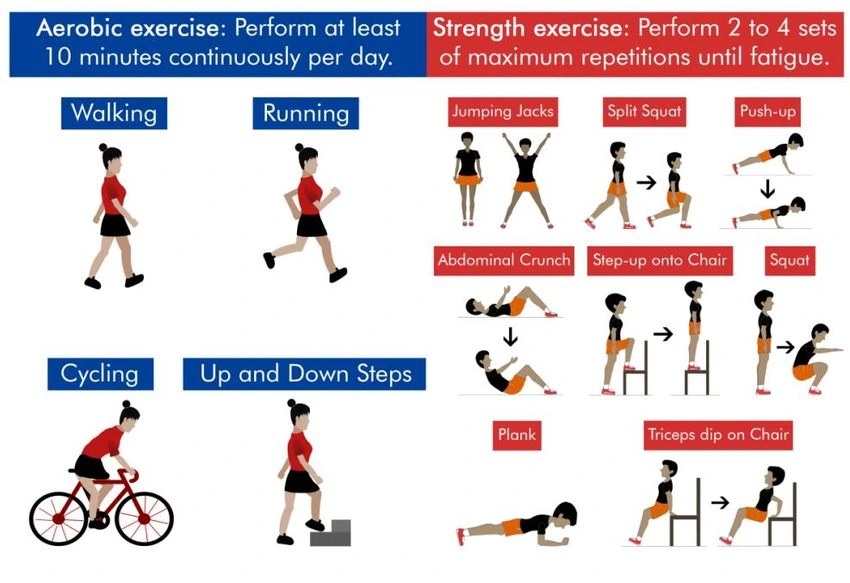
- Such as walking, bicycling, jogging, and swimming will improve the cardiovascular system’s ability to oxygenate the blood that goes to the liver and the rest of the body.
Strength training
- It helps maintain bone mass, improves muscle strength and mass, and helps prevent weight gain through elevation of the metabolism. Construct a great home exercise program.
Prevention
- There is currently no curable vaccine to prevent hepatitis C.
- Although scientists have been working on it for a very long time, hepatitis C has proven difficult to rehabilitate because it has many variations and mutates quickly.
- The only effective way to prevent hepatitis C infection is to avoid contact with infected blood.
- In particular, do not share needles or syringes.
FAQ
Acute hepatitis C generally goes undiagnosed because it rarely causes symptoms. When signs and symptoms are present, they can involve jaundice, along with fatigue, nausea, fever, and muscle aches. Acute symptoms appear 1 to 3 months after exposure to the virus and last two weeks to three months.
Hepatitis B is a possibly life-threatening liver infection caused by the hepatitis B virus (HBV). It is a major worldwide health problem. It may cause chronic infection and put individuals at high risk of death from cirrhosis and liver cancer.
The hepatitis C virus generally spreads through blood. The most usual way that people get it is from injecting drugs — specifically when they share needles or syringes. The risk of getting hepatitis C through sex is minimal, but it is possible.
People with hepatitis C may live many years after diagnosis, but the range varies. One past study showed that patients infected with the hepatitis C virus died on average 15 years sooner than individuals who did not have the illness. With hepatitis C, the liver becomes seriously harmed due to inflammation.
Because of this, individuals with chronic hepatitis C should decrease the amount of iron-rich foods in their diets. These involve red meats, liver, oysters, lentils, apricots, and iron-fortified cereals. However, iron is an important part of the diet so do not cut it out entirely.



One Comment