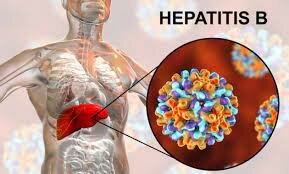
Hepatitis B
Hepatitis B is one of five viruses that may infect the liver, causing inflammation. It is spread through bodily fluids. Most individuals only have a brief, acute infection. But for some individuals, it becomes chronic. Chronic infection may do serious long-term damage to the liver. Hepatitis B is preventable with a vaccine, but it has no cure.
Table of Contents
What is Hepatitis B?
- Hepatitis B is a viral infection that affects the liver.
- It causes inflammation in the liver tissues, which is what “hepatitis” means.
- It initiates an acute infection that is generally short-lived.
- But in some individuals, it turns into a chronic infection that never goes away.
- Long-term inflammation does serious damage to the liver over time.
- It may accelerate cirrhosis and liver failure.
- Like other chronic liver diseases, hepatitis B infection may do this damage without causing symptoms.
- Many individuals do not understand they are infected.
Why is it called “Hepatitis B”?
- There are too many different viruses that may infect the liver and cause inflammation (hepatitis).
- They involved hepatitis A, B, C, D, and E.
- Each is a little different in how they are transmitted, how they affect the human body, and how they are treated (or prevented).
What characteristics hepatitis B from other hepatitis viruses?
- Some distinguishing features of hepatitis B involve:
- Hepatitis B has a safe and effective vaccine that makes it adjectively.
- The World Health Organization (WHO) suggests
- vaccination for all younger babies as soon as possible after birth.
- Hepatitis B disproportionately affects children.
- Only five percent of adults who are infected go on to develop a chronic infection, but thirty percent of children under the age of six do.
- As hepatitis B spreads through bodily fluids, birthing parents may infect their babies at birth. Up to ninety percent of infants infected with hepatitis B develop a chronic infection.
- Chronic hepatitis B symptomatic treatment is available, However, a permanent cure is not possible.
- Antiviral medications may help control the infection, but the person has to take special care of the liver for the rest of her life.
How common is hepatitis B infection?
- Hepatitis B is the most usual liver infection in the world.
- As many as two billion people (or 1 in 3) have been infected globally.
- Roughly 250 million population worldwide are living with chronic hepatitis B infection, but many are unaware.
- It is less usual in America. then in some other places, thanks to the vaccine.
- The Centers for Disease Control and Prevention (CDC) estimates roughly 20,000 new acute infections happen in the U.S. each year.
- An estimated 862,000 individuals in the U.S. are living with chronic hepatitis B.
Symptoms of Hepatitis B
Symptoms of hepatitis B infection, if a person has them, involve fever, nausea, and abdominal pain. Not everyone has symptoms with hepatitis B, but usual symptoms involve the following:
- Not everyone has symptoms. If a person does, they may range from mild to severe. A person can have symptoms (or not) at the time of the acute phase of infection, and a person can also have them (or not) with chronic infection. A person is still contagious with or without symptoms. Typical symptoms of infection involve:

- Fever.
- Loss of appetite.
- Nausea and vomiting.
- Abdominal pain.
- Weakness and fatigue.
- Joint pain.
A person can also have symptoms of liver disease, involving:
- Jaundice (yellowing of your skin and the whites of the eyes).
- Dark-colored urine.
- Light or clay-colored poop.
- Swelling with fluid in the belly or arms and legs.
- With acute infection, symptoms of liver disease can indicate a more severe reaction than normal.
- Although many individuals clear the HBV virus without treatment, you should see a doctor if you have symptoms of liver disease.
- With chronic infection, a person can have mild or vague symptoms on an ongoing basis, or a person can not have symptoms at all for decades. When symptoms appear later, specifically symptoms of liver disease, it can indicate that the liver is beginning to fail.
How do you get hepatitis B?
Hepatitis B infection arises from the hepatitis B virus (HBV). The virus spreads through bodily fluids. Transmission happens when fluids from the body of a person who is infected enter the body of a person who is uninfected. This might happen through:
- Childbirth.
- Sexual contact.
- Contact with an open wound.
- Sharing needles or syringes.
- Sharing a toothbrush or razor.
- Accidental stick from an infected sharp instrument.
- HBV may live on surfaces outside of the body for at least seven days.
- So, used instruments that have not been sterilized may still carry the virus.
- This involves medical instruments and common items such as toothbrushes or razors that can have provoked bleeding.
Besides blood, HBV also lives in some other bodily fluids, including saliva. But dissimilar to some viruses, hepatitis B is not effortlessly transmitted through saliva. That means people are likely to get it from splitting food or eating utensils or from someone coughing or sneezing on them.
Who is more likely to get hepatitis B?
Persons are more likely to get hepatitis B if they belong to a community where the infection is more normal. The more people around a person can be infected, the more chances the virus has to infect the person. Communities with higher rates of infection include:
- People with HIV. As much as 7.5% of individuals with HIV also have chronic hepatitis B.
- People who use intravenous drugs.
- Rates of hepatitis B infection have increased steeply in states recently affected by the opioid crisis.
- People of African, Asian, or Pacific Island descent. Infection rates in these countries range between two percent and eight percent.
- In the U.S., these individuals make up more than half of those with chronic hepatitis B infection.
How do you get chronic hepatitis B?
- Chronic hepatitis B develops when the immune system fails to fight off the virus.
- Most people successfully fight it off at the time of the acute phase of the infection.
- The acute phase is when the immune system identifies the virus and launches its attack.
- When a person has symptoms of illness after an infection, like fever, nausea, and vomiting, those symptoms are part of the immune response.
- The immune system is trying to get rid of the virus by purging and burning it out.
- That is the acute phase.
- Sometimes, some individuals’ immune systems do not succeed in clearing the HBV virus at the time of the acute phase. For too many different reasons, their immune response is weaker than necessary.
- The acute phase only takes place once.
- If the virus survives, there is no other one.
The people might have a weaker immune response to the virus if they:
- Are you a young child whose immune system is still developing?
- Have another infection at the same time.
- Have a chronic medical condition that compromises their immune system.
- Receive immunosuppressant therapy or chemotherapy.
What is reactivated hepatitis B?
- Sometimes after overcoming an acute hepatitis B infection, something causes the immune system to weaken against the virus later in life.
- Maybe the immune system was strong at the time of infection, but now a person has h a condition that weakens it.
- When this happens, the once-defeated virus may become active in the body again.
- Reactivated hepatitis B may be temporary or lasting.
- But because it tends to happen in immune-suppressed individuals, it may be specifically severe and even cause acute liver failure.
How long are you contagious with hepatitis B?
- Persons are contagious as long as the virus is active in the body.
- If a person has an acute infection, it can last from a few weeks to six months and persons are contagious that entire time.
- If a person has a chronic infection, the persons are contagious as long as it lasts, which is generally for life.
What are the practicable complications of hepatitis B infection?
Most complications arise from chronic infection, but some individuals can have complications with acute infection. Though it is not Usually, some individuals experience acute liver failure with acute hepatitis B infection, which is a life-threatening emergency. Complications of chronic hepatitis B may include:
Hepatitis D-
- Hepatitis D, or delta virus, is another viral hepatitis infection that only affects individuals with hepatitis B.
- If individuals have chronic hepatitis B, they may get both viruses.
- This is called superinfection. It doubles the stress on the liver and may lead to acute liver failure.
Cirrhosis
- Chronic liver inflammation leads to cirrhosis in some individuals.
- It takes a long time and is based on many factors, like the overall health of the liver and other conditions that might affect it.
- Cirrhosis occurs when injured liver tissues are slowly
- replaced with scar tissue.
- The scar tissue stops the liver from functioning, which leads to chronic liver failure.
Chronic liver failure-
- Chronic liver failure is a usual process where the liver loses its ability to function over time. It generally
- follows cirrhosis. Even though it occurs slowly, chronic liver failure is life-threatening.
- A person may not live without a functioning liver.
- Liver failure may also cause life-threatening side effects as it progresses.
- The only treatment is a liver transplant.
Liver cancer-
- For reasons that are not entirely clear, individuals with chronic hepatitis are more likely to develop primary liver cancer.
- In fact, doctors consider chronic hepatitis B to be the leading cause of liver cancer.
- Liver cancer itself is one of the leading causes of death in individuals with chronic hepatitis B.
How is hepatitis B diagnosed?
A doctor will ask a person about the symptoms and physically examine her. They might ask about their health history, any history of liver disease in the family, or other factors that might make a person more susceptible to viral hepatitis. As a person might not have symptoms or any known risk factors, the only way to rule out for sure if a person has hepatitis B is by testing the blood. Specific blood tests may tell the doctor all they need to know about the condition, like:
- If the people have an acute or chronic infection.
- If a person has been infected in the past.
- If people have developed immunity to the virus.
- If the infection is interfering with liver function.
- After diagnosis, the doctor may want to order a few more tests to check how the liver is doing.
- They might want to look at radiographic images of the liver tissues.
- In some cases, they might want to take a small sample for testing in the lab (liver
- biopsy).
Recent exposure
- If a person has only recently been exposed to HBV and the virus is still incubating in the body, it might not show up on a blood test yet.
- A doctor can not be able to tell right away if a person has been infected, but they may still treat a patient preventatively.
Treatment of Hepatitis B
A doctor can give you different treatment options based on the status of the infection.
Prophylactic treatment
If a person has reason to believe you or your child has recently been exposed to the virus, a doctor might recommend prophylactic treatments to help reduce the infection from taking hold. These treatments include:
Vaccination-
- Healthcare providers suggest an immediate dose of the hepatitis B vaccine if a person has not had it yet, preferably
- within 24 hours of exposure.
- A person will need two more doses over the next 6 months to become fully vaccinated against the virus.
Hepatitis B immune globulin (HBIG)-
- HBIG is a substance produced from human blood containing naturally-creates antibodies to the hepatitis B virus.
- It is given as a shot to help prevent infection in people who have recently been exposed to the virus.
- These treatments are very effective in preventing babies born to parents with chronic hepatitis B from becoming infected.
- Infants who receive these treatments quickly after birth have a good prognosis, and they may safely breastfeed (chest feed).
Acute treatment
There is no specific medication to treat an acute hepatitis B infection, and many individuals do not need any treatment. But if the person is having severe symptoms, a doctor might monitor the person for complications and offer supportive care, like:
- IV fluids.
- IV nutrition.
- Pain relief.
Treatment for chronic infection
Too many medications are available to treat chronic hepatitis B, but they can not be safe for everyone. A doctor will recommend treatment based on the condition and risk factors. The treatment plan can involve:
Surveillance
A doctor treating a person for chronic hepatitis B will monitor the liver health through regular checkups and testing, ideally every 6 months. They will look for signs of active liver disease that can be affecting the liver’s functioning. Tests can involve:
- Blood tests.
- Imaging tests.
- Elastography (organ stiffness scan).
Medication
- Doctors have found that current medications for hepatitis B are most effective for individuals who show signs of active
- liver disease.
- This may be only 25% of individuals diagnosed with chronic hepatitis B, according to the World Health Organization (WHO).
- Current medications help to increase the immune system and slow down the rate at which the virus reproduces itself.
- They do not kill the virus completely, but they may help keep the liver as healthy as possible for as long as possible. They include:
Immune modulator drugs
- Immune modulators, also identify as interferons, involve peginterferon alfa-2a, and interferon alfa-2 b.
- These are synthetic versions of the antibodies our bodies generate to fight infections.
- They are given by injection for a course of 6 to 12 months.
- They are prescribed for some people and as a first-line treatment for children.
Oral antiviral medications
- Antivirals taken by mouth are the most powerful medications for suppressing HBV.
- The doctor might suggest one or several based on who a patient is and how the patient responds.
- First-line antivirals involve tenofovir disoproxil or tenofovir alafenamide and entecavir.
- Most individual who starts these medications will continue them for life.
Lifestyle changes
- Whether or not a person is taking medication for hepatitis B, a person will require to take steps to protect the liver from further harm throughout life. Doctors particularly suggested that a person avoid alcohol and maintain a healthy, balanced diet.
- Alcohol use and metabolic factors like a high BMI and high triglycerides are two of the leading causes of liver inflammation outside of infection. When a person already has chronic hepatitis, it is best to limit alcohol, sugar, and fat intake to decrease inflammation.
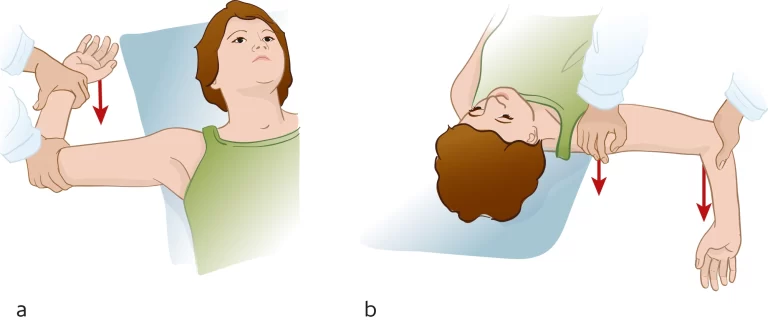
Physiotherapy treatment
- During physical activity, it is necessary to monitor the patient for signs and symptoms of fatigue.
- As for Hepatitis A bed rest is the best form of treatment and being aware of the acuteness of the Hepatitis infection is crucial when screening for physical therapy.
- Supportive therapy and patient education are used to make sure the patient is comfortable and has a sufficient nutritional balance for all three infections. It is also important to remind the patient to abstain from the use of alcohol or intake of fatty substances.
- More and more physicians are identifying the value of exercise for liver patients as exercise causes improvements in quality of life and better prognoses.
The below-given liver benefits have been shown in studies to be associated with regular exercise:
Decreased risk of scarring and cirrhosis in Hepatitis C –
- Regular exercise decreases the incidence of obesity in HCV patients. Studies show that avoiding obesity helps prevent the resulting conditions – fatty liver, elevated blood glucose, diabetes, and elevated blood insulin – That lead to scarring and cirrhosis.
Hoisted mood –
- Depression is the most usual problem among people suffering from chronic liver disease.
Improve blood oxygenation –
- The cardiovascular benefits of daily exercise enhance the oxygen-carrying capability of the blood thus more oxygen is delivered to the liver, which creates a higher-functioning liver.
Reduced atrophy –
- Strength training supports muscle growth and maintenance which may avert or delay the severe muscle wasting seen in advanced liver disease.
Improved energy –
- Over time, regular exercise improves the efficiency of the Cardiovascular System.
- This inverse transportation of oxygen and nutrients to all cells, tissues, organs, and systems, leads to a higher energy level.
Exercise program –
- It incorporates aerobic/cardiovascular conditioning and strength training to have a major effect on liver function.
Aerobic exercises

- Aerobic exercises Such as walking, bicycling, jogging, and swimming will improve the overall cardiovascular system’s ability to oxygenate the blood that goes to the liver and the rest of the body.
Strength training
- It helps maintain bone mass, improves muscle strength and mass, and helps prevent weight gain through elevation of the metabolism.
- Construct a great home exercise program.
Surgery
- If chronic hepatitis leads to complications like cirrhosis and liver failure or liver cancer, a person might need to have surgery to remove part or all of the liver.
- The liver may regenerate itself after partial resection, as long as enough healthy tissue remains.
- If too much of the liver is diseased or failing, however, a person will need a liver transplant to replace it.
- Most donated livers come from recently reduced people, and there is a long waiting list for these.
- But a person may skip the wait if they are able to find a living liver donor.
How to Prevent Hepatitis B?
The best way to prevent infection is vaccination. If a person is vaccinated against the virus, person does not want to worry about accidental exposure in day-to-day life. However, it does take about 6 months to complete the three doses of the hepatitis B vaccine.
In the short term, a person may decrease the risk by:
Practicing safe sex-
- If a person does not know whether the partner is infected, use a latex or polyurethane condom.
- Not sharing personal items that might be exposed to blood, like toothbrushes, razors, medical equipment, or needles.
Planning ahead for travel abroad
- If a person plans to travel to regions where the rate of infection is relatively high, schedule the vaccinations before you go.
Prophylactic treatment
- If a persons think they can have recently been exposed, they may decrease the risk of infection by receiving a dose of vaccine and hepatitis B immune globulin within a few hours.
FAQ
Chronic hepatitis B may develop into a serious disease resulting in long-term health problems, involving liver damage, liver failure, liver cancer, and even death. There were 1,649 deaths related to the hepatitis B virus reported in the past few years, but this is an underestimate.
The most important thing to remember is that hepatitis B is a chronic medical condition (like diabetes and high blood pressure) that may be successfully managed if a person takes good care of their health and their liver. A person should expect to live a long, full life.
A person who becomes HBsAg negative and develops an antibody to HBsAg (anti-HBs) is diagnosed as having resolved hepatitis B. This is an unusual phenomenon in chronic HBV infection. At the time of HBV DNA can still be detectable by PCR in serum and more often in the liver.
They have limited advantage against cccDNA, the seemingly indestructible “mini-chromosome” of the hepatitis B virus that continues to produce virus particles in infected liver cells, even in individuals being treated. A cure, therefore, would have to demolish or silence cccDNA and provide long-term protective immunity.
Recent studies recommend resveratrol, vitamin E, lactoferrin, selenium, curcumin, luteolin-7-O-glucoside, moringa extracts, chlorogenic acid, and epigallocatechin-3-gallate may be effective for patients with hepatitis B. The anti-HBV effect of most of these nutrients has been analyzed in vitro and in animal models.