BACK PAIN: PHYSIOTHERAPY TREATMENT
Table of Contents
WHAT IS BACK PAIN?
Back pain is pain that occurs in the back May Be Upper Back Pain Or Low Back Pain. The back is divided into middle back pain (thoracic), lower back pain (lumbar), or coccydynia (tailbone or sacral pain) based on the segment affected.
Back pain can affect people of any age, for different reasons. As people get older, the chance of developing lower back pain increases, due to factors such as previous occupation and degenerative disk disease.
Lower back pain may be linked to the bony lumbar spine, discs between the vertebrae, ligaments around the spine and discs, spinal cord and nerves, lower back muscles, abdominal and pelvic internal organs, and the skin around the lumbar area.
> Pain in the upper back may be due to disorders of the aorta, tumors in the chest, and spine inflammation.
ANATOMY OF BACK:
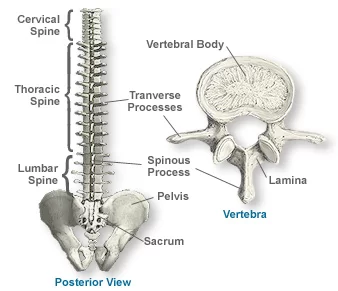
The human back is the large posterior area of the human body, rising from the top of the buttocks to the back of the neck and the shoulders. It is the surface of the body opposite from the chest.
The vertebral column runs the length of the back and creates a central area of recession. The breadth of the back is created by the shoulders at the top and the pelvis at the bottom.
The thoracic spine (upper back or mid-back region) :
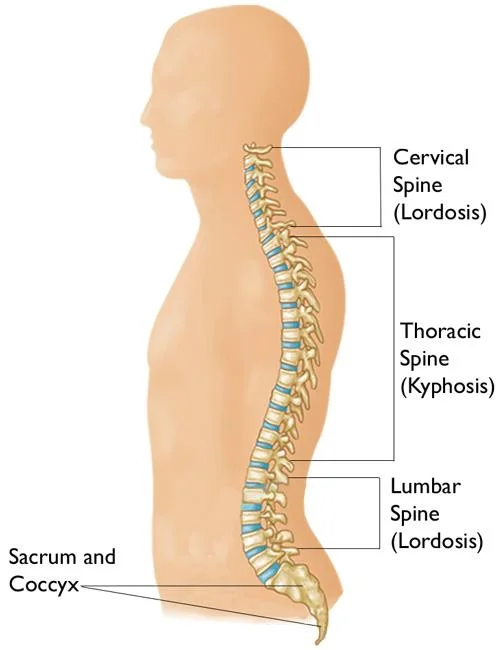
The thoracic spine is made up of 12 vertebrae. It is located below the top 7 vertebrae of the cervical spine and above the lumbar spine. These vertebrae connect to your ribs and form part of the back wall of the thorax (the ribcage area between the neck and the diaphragm). The curve of the thoracic spine is a “C”-shape with the opening of the “C” in the front. This type of curve is called a kyphotic curve.
The thoracic spine has very narrow, thin intervertebral discs. In addition, the ribs are connected to the spine in the thoracic segment. These rib connections, combined with the smaller intervertebral discs, limit the amount of movement in the thoracic spine compared to the lumbar or cervical segments of the spine. There is also less space inside the spinal canal.
The Lumbar Spine (Low Back):
The lowest part of the spine is called the lumbar spine. This area usually has 5 vertebrae. However, sometimes people are born with 6 vertebrae in the lumbar region. The base of your spine (called the sacrum) is a group of specialized vertebrae that connect the spine to the pelvis. When one of the bones forms as a vertebra rather than part of the sacrum, it is called a transitional (or sixth) vertebra.
This occurrence is not dangerous and does not appear to have any serious side effects. The lumbar spine is shaped like a backward “C”, just like the cervical spine. This shape is called a lordotic curve. If you think of the entire spine as having an “S”-like shape, the lumbar region would be the bottom of the “S”. The vertebrae in the lumbar spine are the largest of the entire spine.
The lumbar spinal canal is also larger than the cervical or thoracic segments of the spine. The size of the lumbar spine allows for more space for nerves to move about. When people experience pain in their spine it often occurs in the lumbar region. This is because the lumbar spine is connected to your pelvis, which is where most weight-bearing and body movement takes place. Typically this is where people tend to place too much pressure, such as when lifting up a heavy box, twisting to move a heavy load, or carrying a heavy object. These activities can cause repetitive injuries that can lead to damage to the parts of the lumbar spine.
Sacral spine:
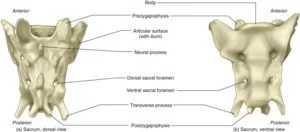
The sacrum is a large, triangular bone at the base of the spine that forms by the fusing of sacral vertebrae S1–S5 between 18 and 30 years of age. The sacrum is situated at the upper, back part of the pelvic cavity, between the two wings of the pelvis. It forms joints with four other bones. The two projections at the sides of the sacrum are called the alae (wings) and articulate with the ilium at the L-shaped sacroiliac joints.
The upper part of the sacrum connects with the last lumbar vertebra, and its lower part with the coccyx (tailbone) via the sacral and coccygeal cornua. The sacrum has three different surfaces which are shaped to accommodate surrounding pelvic structures. Overall it is concave (curved upon itself). The base of the sacrum, the broadest and uppermost part, is tilted forward as the sacral promontory internally. The central part is curved outward toward the posterior, allowing greater room for the pelvic cavity.
In all other quadrupedal vertebrates, the pelvic vertebrae undergo a similar developmental process to form a sacrum in the adult, even while the bony tail (caudal) vertebrae remain unfused. The number of sacral vertebrae varies slightly. For instance, the S1–S5 vertebrae of a horse will fuse, the S1–S3 of a dog will fuse, and four pelvic vertebrae of a rat will fuse between the lumbar and the caudal vertebrae of its tail.
CAUSES OF BACK PAIN:
- Sciatica:
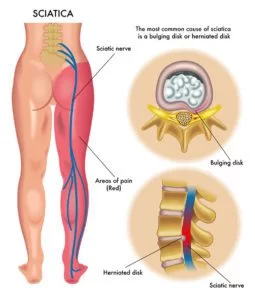
Sciatica refers to compression or pinching of the sciatic nerve, often caused by a herniated disc or bone spur. An injury or trauma to the pelvis, buttocks, or thigh, diabetes, prolonged sitting, and piriformis syndrome—when a small muscle in the buttocks spasms and irritates the sciatic nerve—may also cause sciatica.
Because your sciatic nerve is the longest nerve in the body (running from the base of the spine down both legs), compression of it may lead to lower back pain that spreads into the buttocks, and down the legs into the soles of the feet (usually on one side). In addition to burning and/or cramping pain, patients may experience tingling, numbness, and muscle weakness.
2. Back Muscle or ligament strain:
Repeated heavy lifting or a sudden awkward movement can strain back muscles and spinal ligaments. If you’re in poor physical condition, constant strain on your back can cause painful muscle spasms.
3. Infection
An infection in the spine, called vertebral diskitis or osteomyelitis, causes severe, constant pain. Surprisingly, despite an infection being present, a person may not have a fever. A history of a prior back surgery may provide a clue that an infection is present.
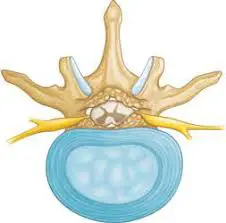
4. Bulging or ruptured disks:
Disks act as cushions between the bones (vertebrae) in your spine. The soft material inside a disk can bulge or rupture and press on a nerve. However, you can have a bulging or ruptured disk without back pain. Disk disease is often found incidentally when you have spine X-rays for some other reason.
5. Ankylosing Spondylitis (AS)
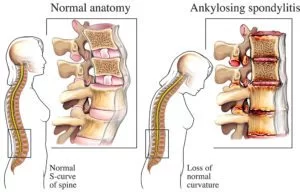
AS is a chronic inflammatory disease of the spine joints (vertebrae) that causes low back pain and stiffness, typically starting before the age of 40. The back pain of AS tends to improve with exercise and worsen at night.
6. Arthritis:
Osteoarthritis can affect the lower back. In some cases, arthritis in the spine can lead to a narrowing of the space around the spinal cord, a condition called spinal stenosis.
7. Cauda equina syndrome:
where the nerves in the lower back become severely compressed.
8. Skeletal irregularities:
A condition in which your spine curves to the side (scoliosis) also can lead to back pain, but generally not until middle age.
9. Osteoporosis:
Your spine’s vertebrae can develop compression fractures if your bones become porous and brittle.
CLASSIFICATION OF BACK PAIN
Superficial: Localized in skin and subcutaneous tissue e.g. skin abscess, laceration, incision, contusion, hematoma, and hair follicle infection.
Deep: Localized in muscles and tendons e.g. muscle tear, muscle injuries, severe spasm, myofascial pain, and fibromyalgia.
acute: Acute back pain lasts less than a month
subacute: back pain lasts over a month but less than three months
chronic: lasts over three months. If the pain has lasted any longer than three days, you should see a physician. Physicians will locate the issue in 4 specific areas of your back: neck (cervical region), upper back (thoracic region), lower back (lumbar region), and tailbone (sacral and coccyx regions).
SIGNS & SYMPTOMS OF BACK PAIN:
> a dull aching sensation in the lower back
> a stabbing or shooting pain that can radiate down the leg to the foot
> an inability to stand up straight without pain
> A decreased range of motion and diminished ability to flex the back
> Muscle ache
DIAGNOSOS OF BACK PAIN
1. X-ray: These images show the alignment of your bones and whether you have arthritis or broken bones. These images alone won’t show problems with your spinal cord, muscles, nerves, or disks.
2. MRI or CT scans: These scans generate images that can reveal herniated disks or problems with bones, muscles, tissue, tendons, nerves, ligaments, and blood vessels.
3. Blood tests: These can help determine whether you have an infection or other condition that might be causing your pain.
4. Bone scan: In rare cases, your doctor might use a bone scan to look for bone tumors or compression fractures caused by osteoporosis.
5. Nerve studies: Electromyography (EMG) measures the electrical impulses produced by the nerves and the responses of your muscles. This test can confirm nerve compression caused by herniated disks or narrowing of your spinal canal (spinal stenosis).
EXAMINATION OF BACK PAIN
PATIENT STANDING:
• Inspect the spine for any developmental or traumatic deformities. Assess the lumbar lordosis; loss of curvature may indicate ankylosing spondylitis. Look for any muscle wasting (buttock, thigh, calf). Check for any discrepancy in leg length by comparing the levels of the iliac crests.
• Movement: Ask the patient to extend the spine, flex forward, and then flex laterally by sliding their palm down their outer thigh. Most patients with non-specific back pain will be slightly stiff in extension, have pain on flexion, and have asymmetric limitation and pain on lateral flexion.
PATIENT SUPINE LYING:
1. Rule out other joint involvement: check the hip joints for range of movement and pain. Perform stress test on sacro-iliac joints (e.g. FABER test), especially in young patients.
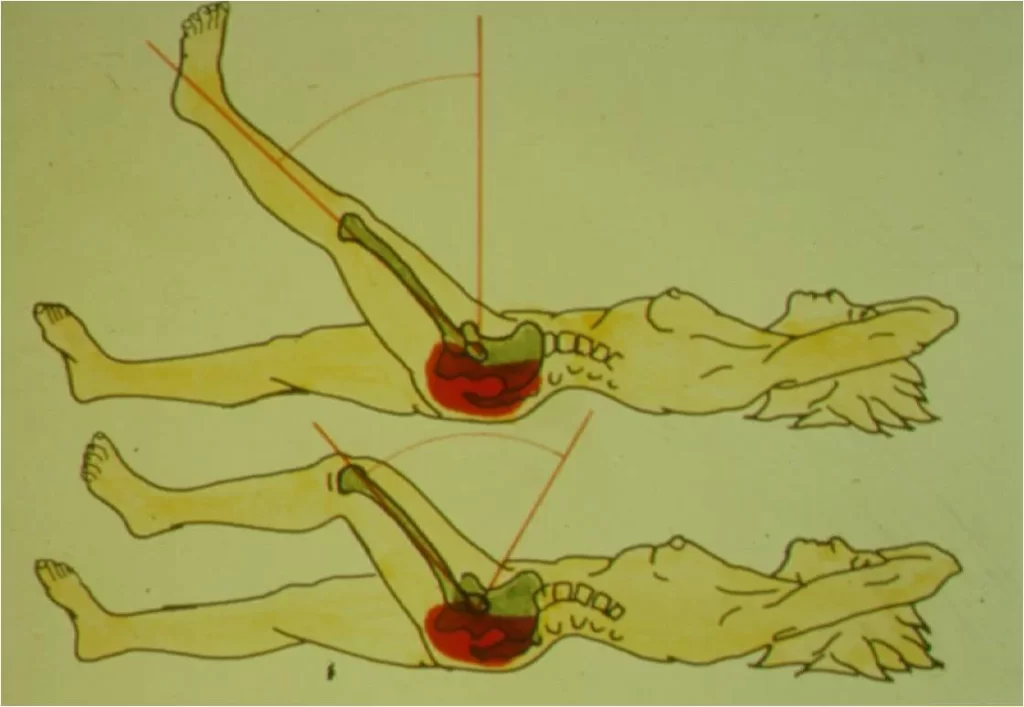
>The FABER test:

The Flexion, Abduction, and External Rotation (FABER) test is used to detect hip or sacro-iliac joint problems. The patient lies in a supine position, and the foot is placed on the opposite knee; in this position groin pain indicates a hip problem rather than a spinal problem. The doctor then presses on the flexed knee and on the opposite anterior superior iliac crest; pain in the sacroiliac area indicates a problem with sacroiliac joints.
2. Test the nerve roots:
Straight leg raise test: This stretches nerve roots L4, L5, and S1. Pick the leg up by the ankle. While keeping the knee fully extended, lift the leg up towards ninety degrees or beyond. If the patient has significant nerve root entrapment shooting leg pain will be reproduced before you get much beyond thirty degrees of elevation. Back pain produced by straight leg raising is common and does not always indicate nerve root involvement.
Femoral nerve traction test:
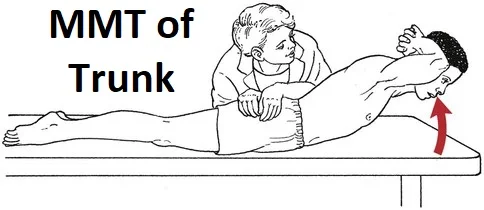
3. Assess muscle power:
Muscle group Nerve root
>Resisted flexion of hip L2 and L3
>Resisted knee flexion S2
>Resisted dorsiflexion of the ankle L4
>Resisted extension of the big toe L5
>Resisted eversion of the foot or –
resisted plantar flexion of the ankle S1
4.. Check the reflexes:
Reflex Nerve root
>Knee jerk L3 and L4
>Ankle jerk L5 and S1
>Plantar refl-ex Up-going toes in adults may indicate upper motor neurone abnormalities such as myelopathy or demyelinating disease, rather than a common low back problem.
5. Check for skin sensory loss:
Disk L3–L4 L4–L5 L5–S1
Nerve root L4 L5 S1
Sensory loss- Medial malleolus Dorsal third Lateral heel
signature zone Metatarsophalangeal joint
Palpate the spine for tenderness and for muscle spasms.
SPECIAL TEST:
For neurological dysfunction:
• Slump test :
For lumbar instability:
• Prone segmental instability test :

>For joint dysfunction:
• One-leg standing (stork standing) lumbar extension test :
>For muscle tightness:
• 90–90 straight leg raise test:

• Ober test:

• Rectus femoris test:

• Thomas test:

>Other tests:
• Sign of the buttock:
RISK FACTORS:
- Aging:
Over time, wear and tear on the spine may result in conditions (e.g., disc degeneration, spinal stenosis) that produce neck and back pain. This means that people over age 30 or 40 are more at risk for back pain than younger individuals. People aged 30 to 60 are more likely to have disc-related disorders, while people over age 60 are more likely to have pain related to osteoarthritis.
2. Genetics:
There is some evidence that certain types of spinal disorders have a genetic component. For example, degenerative disc disease seems to have an inherited component.
3. Occupational hazards:
Any job that requires repetitive bending and lifting has a high incidence of back injury (e.g., construction worker, nurse). Jobs that require long hours of standing without a break (e.g., barber) or sitting in a chair (e.g., software developer) that does not support the back well also puts the person at greater risk.
4. Diet :
A diet high in calories and fat, combined with an inactive lifestyle, can lead to obesity, which can put stress on the back.
5. Race:
Race can be a factor in back problems. African American women, for example, are two to three times more likely than white women to develop spondylolisthesis, a condition in which a vertebra of the lower spine – also called the lumbar spine – slips out of place.
6. Sleeping on the wrong mattress:
A study in The Lancet found that people who chose a medium-firm mattress showed fewer signs of back issues three months after purchasing their mattresses compared to people who bought firm mattresses. Follow Goldilocks’ advice: don’t have a bed that’s too hard or too soft, but rather just right.
7. Smoking:
Cigarette smoking accelerates degeneration of the lower spine. Nicotine restricts blood flow to vertebrae and disks, so they may age and break down more quickly. Smoking may also interfere with the body’s ability to absorb and use calcium, leading to osteoporosis-related bone and back problems.
8. Being depressed, anxious, and/or stressed:
A study published in Arthritis Care and Research suggests that people who suffer from depression have a 60% greater chance of developing LBP in their lifetime than those who don’t. This emphasizes the importance of understanding the bio-psychosocial interpretation of pain, that is, how biological, psychological, and social factors interact to help us understand the cause and outcome of disease and wellness.
9. Pregnant women:
Pregnancy makes women prone to back pain due to the shifting of abdominal organs, the forward redistribution of body weight, and the loosening of ligaments in the pelvic area prior to delivery.
10. Repetitive work:
Certain types of repetitive work, such as factory work or truck driving, put you at risk of back pain. Risky activities include lifting, forceful movements, bending and twisting into awkward positions, repetitive movements, and vibration (such as the vibration that occurs with long-distance truck driving).
TREATMENT
> Over-the-counter (OTC) pain relievers:
Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen (Advil, Motrin IB, others) or naproxen sodium (Aleve), might relieve acute back pain. Take these medications only as directed by your doctor. Overuse can cause serious side effects. If OTC pain relievers don’t relieve your pain, your doctor might suggest prescription NSAIDs.
> Muscle relaxants:
If mild to moderate back pain doesn’t improve with OTC pain relievers, your doctor might also prescribe a muscle relaxant. Muscle relaxants can make you dizzy and sleepy.
> Topical pain relievers:
These are creams, salves, or ointments you rub into your skin at the site of your pain.
> Narcotics:
Drugs containing opioids, such as oxycodone or hydrocodone, may be used for a short time with close supervision by your doctor. Opioids don’t work well for chronic pain, so your prescription will usually provide less than a week’s worth of pills.
> Antidepressants:
Low doses of certain types of antidepressants — particularly tricyclic antidepressants, such as amitriptyline — have been shown to relieve some types of chronic back pain independent of their effect on depression.
> Injections:
If other measures don’t relieve your pain, and if your pain radiates down your leg, your doctor may inject cortisone — an anti-inflammatory medication — or numbing medication into the space around your spinal cord (epidural space). A cortisone injection helps decrease inflammation around the nerve roots, but the pain relief usually lasts less than a few months.
SURGERY
Spinal fusion
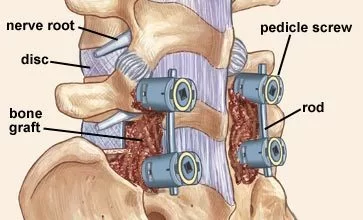
This is the most common surgery for chronic nonspecific back pain with degenerative changes. The doctor will join spinal bones, called vertebrae, together. This limits the motion between them and how far your nerves can stretch. But it probably won’t limit your activity. It’s rare, but the bones don’t always fuse completely. Smoking can make this complication more likely. If it happens, you may need another operation to fix it.
> Laminectomy:
This is the most common surgery for lumbar spinal stenosis. In this procedure, a surgeon removes parts of the bone, bone spurs, or ligaments in your back. This relieves pressure on spinal nerves and can ease pain or weakness, but the procedure can make your spine less stable. If that happens, you’ll probably need a spinal fusion as well. Doctors sometimes do the two procedures together.
> Foraminotomy:
This surgery is used to relieve pain associated with a compressed nerve in the spine. The surgeon cuts away bone at the sides of your vertebrae to widen the space where nerves exit your spine. The extra room may relieve pressure on the nerves and ease your pain. Like a laminectomy, this procedure can also make your spine less stable. So the surgeon may do a spinal fusion at the same time. That’ll increase the amount of time you need for recovery.
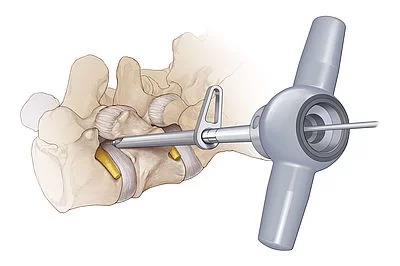
> Diskectomy:
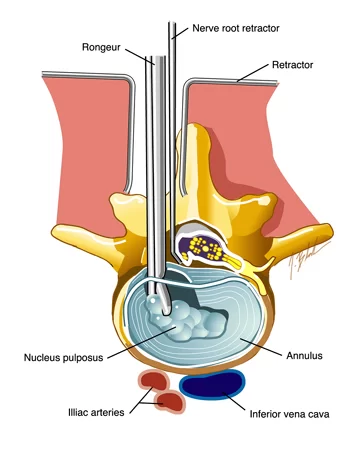
Sometimes a disk, the cushion that separates your vertebrae, can slip out of place, press on a spinal nerve, and cause back pain. In a diskectomy, the surgeon removes all or part of the disk. He may have to make a big cut in your back, or he may be able to do it through a small one called microdiscectomy. Microdiscectomy is performed with an operating microscope through a smaller incision than open discectomy and has become the standard surgical procedure for lumbar disc herniation. Sometimes a diskectomy is part of a larger surgery that includes laminectomy, foraminotomy, or spinal fusion.
> Disk replacement:
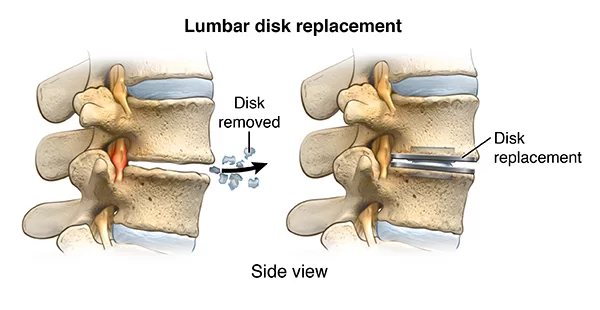
A surgeon removes the damaged spinal disk and inserts an artificial one between your vertebrae. Unlike fusion, this lets you continue to move your spine. Recovery time may be shorter than for a spinal fusion, too. But there is a slight chance the new disk could slip or fall out of place and require repair.
> Interlaminar implant:
This is a minimally invasive alternative to more invasive laminectomy or laminectomy plus fusion surgery. The surgeon implants a U-shaped device between two vertebrae in your lower back. It helps keep the space between them open and eases pressure on your spinal nerves. It can be done at the same time as a laminectomy. Unlike spinal fusion, the implant provides stability and lets you move your back almost like normal. You may not be able to bend backward as easily in that area.
The biggest risk of back surgery: Not knowing for sure if it’s going to help with your pain. The best thing you can do is talk openly with your surgeon so he knows what’s going on with your health and you know what to expect before you go into the operating room.
PHYSIOTHERAPY TREATMENT OF BACK PAIN:
The goal of physiotherapy treatment for back pain is to reduce pain and restore normal function and mobility. When deciding on treatment options for low back pain, patients’ symptoms, physical examination results, and diagnostic tests are taken into consideration.
- Ice or heat
Heat or ice is often used to reduce pain, stiffness, and swelling in middle and upper back pain. Heat can reduce pain and stiffness whilst ice can help reduce pain and swelling.
2. Back Brace
A back brace or corset can provide excellent relief for most lower back pain and sciatica sufferers. Those who gain the most benefit are those who find their pain eases when they wrap/bind a towel or sheet (folded-lengthwise) tightly around their stomach and lower back. If this simple test eases your back pain, you should use a back brace in the short term. Back braces and strong deep core muscles help to avoid a recurrence in the future.
3. TENS / IFT / US Machine:
an electronic pain-relieving device that will reduce your lower back pain and your need for pain-relieving drugs will Reduce.
4. Intermittent Lumbar Traction Machine:
Mechanical lumbar traction operates under the theory that separation of the lumbar vertebrae will decrease impingement of the spinal nerves as well as decrease intradiscal pressure. Newer mechanical traction units apply traction to the spine via a computer-driven table, which controls the level of disc decompression with an average treatment time of 30 minutes.
EXERCISES FOR UPPER & LOWER BACK:
> PELVIC ROTATION
This is a great warm-up exercise and a good way to mobilize and loosen your lower back. Start by lying on your back with your feet on the ground and knees bent and together. Slowly move your knees side to side going as far as you can without causing pain. Continue for 1 minute.
> Single Knee to Chest

Lie on your back and bring one knee up to your chest. Hold for 1-2 seconds and then slowly return to the starting position.
Maintain relaxed breathing throughout the exercise. Repeat the above steps 4-6 times on each leg.
This is a great stretch for the hip, pelvis, and lower back.
>Pectoralis stretch:
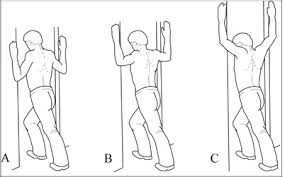
Stand in an open doorway or corner with both hands slightly above your head on the door frame or wall. Slowly lean forward until you feel a stretch in the front of your shoulders. Hold for 15 to 30 seconds. Repeat 3 times.
> Thoracic extension:
Sit in a chair and clasp both arms behind your head. Gently arch backward and look up toward the ceiling. Repeat 10 times. Do this several times each day.
> Arm slide on wall:
Sit or stand with your back against a wall and your elbows and wrists against the wall. Slowly slide your arms upward as high as you can while keeping your elbows and wrists against the wall. Do 2 sets of 8 to 12.
> Cat/Cow:

Kneel on all fours, with the hands beneath your shoulders and knees below your hips. While exhaling, gently arch your spine. And while inhaling, tighten your core muscles and arch your back outwards like a cat. Do 2 sets of 10.
> Thoracic stretch:
Sit on the floor with your legs out straight in front of you. Hold your mid-thighs with your hands. Curl you head and neck toward your belly button. Hold for a count of 15. Repeat 3 times
>Pelvic Tilt:
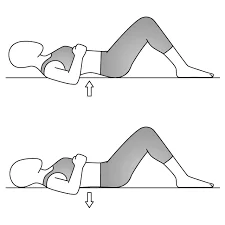
lie on your back and place a small cushion under your head. Bend your knees and keep your feet hip-width apart and placed on the floor. Keep your upper body relaxed and your chin gently tucked-in. Gently flatten your lower back into the floor and contract your stomach muscles. Now tilt your pelvis towards your heels until you feel a gentle arch in your lower back, feeling your back muscles contract and return to the starting position. Place one hand on your stomach and the other under your lower back to feel the correct muscles working. Repeat eight to twelve times, tilting your pelvis back and forth in a slow rocking motion.
>Bridge:

lie on your back with knees bent and your feet placed hip distance apart on the floor. Take a deep breath in and as you breathe out lift your hips off the floor until your shoulders hips and knees are in a straight line. As you breathe in lower your hips to the floor. Repeat eight to twelve times.
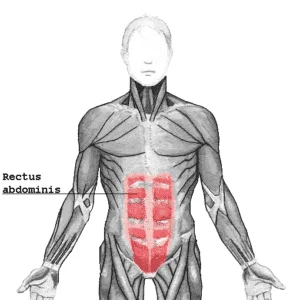
>Isometric Back Extention Exercises:
lying on your back and press the head and heel. Repeat 12 times.
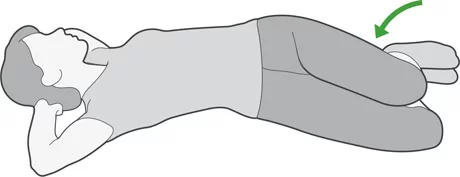
> Piriformis Stretch:

lie on your back and cross the right ankle over the left knee. Grip the thigh of your left leg and take a deep breath in. As you breathe out pull the knee in towards you. Hold the stretch for 20-30 seconds. Repeat two times for each side.
Again this stretch may be too aggressive for acute low back pain. We can help modify it so you do not make it worse.
> Hip flexor Stretch:
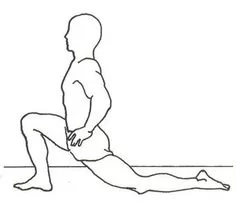
It is also good to stretch out your hip as your hip flexor muscles are very often tight when you have lower back pain. When the hip flexors are tight it can alter your posture leading to what is referred to as ‘donald duck posture’ where your butt sticks out too far. This tightens up your lower back and can lead to lower back pain. To stretch the hip flexors, kneel with one knee on the floor and the other foot in front with the knee bent. Push the hips forward and keep your back upright. Hold the stretch for 20-30 seconds. Repeat two times on each side.
> Hamstring stretch:
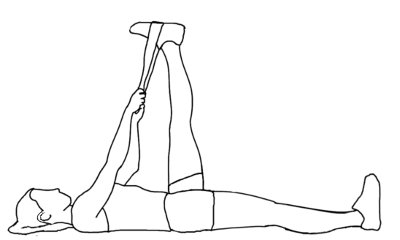
Lay on your back, with one leg STRAIGHT and one leg in the air with a stretch band around your foot. Hold for 30 seconds, repeat both legs 5 times.
DO’S:
> Sit upright in a chair and adjust the monitor just below the eye level.
> Exercise your back regularly – walking, swimming (especially backstroke), and using exercise bikes are all excellent to strengthen your back muscles but anything that you enjoy and helps you keep active will be beneficial.
> Keep active and moving even when you have pain. Gentle walking and stretching will prevent stiffness. Also, try to avoid long periods of bed rest as this is counterproductive.
> Always lift and carry objects close to your body, bend your knees and your hips, not your back, and never twist and bend at the same time.
> Try to maintain a healthy diet and lifestyle as this will help prevent back pain. Quit smoking as it increases your chances of developing back pain.
> Getting the right mattress. No matter how comfortable a squishy-soft feather bed may seem at first, a firmer mattress is usually the best for your back
> Set your car seat properly. Don’t push it so far back that you have to lean and hunch forward to reach the steering wheel.
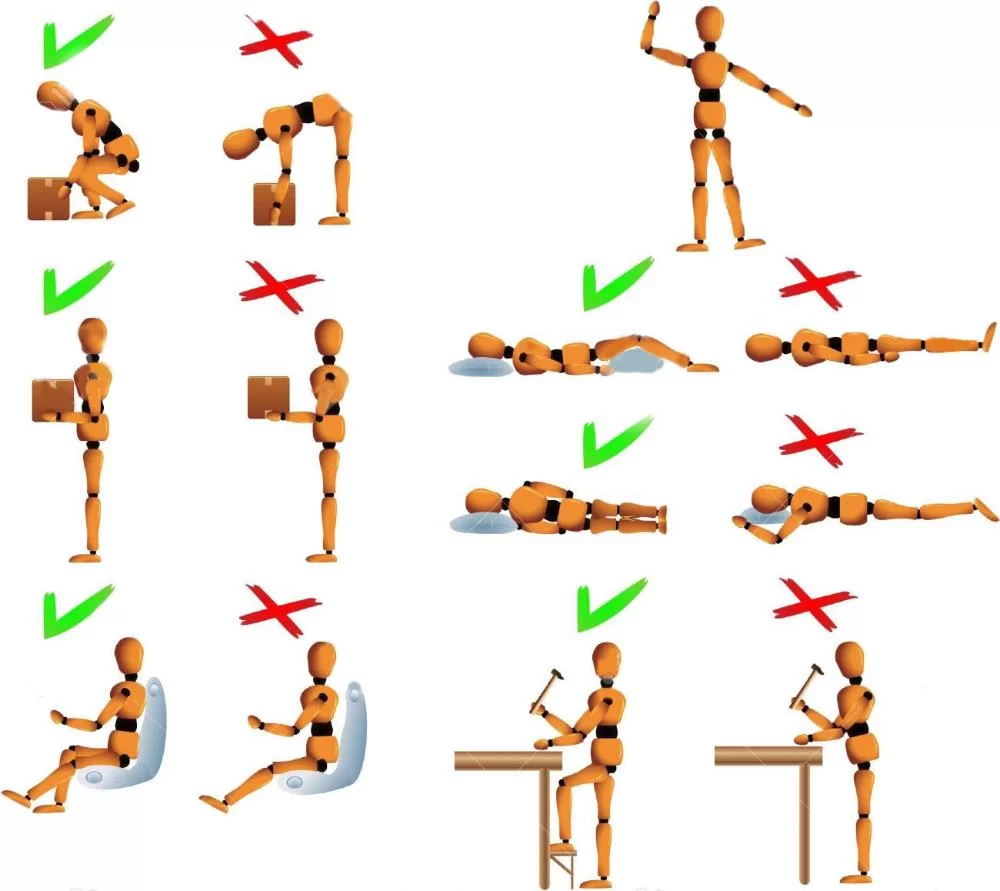
DON’Ts:
> Avoid carrying single sling bags
> Avoid slumping in your chair, hunching over your desk, and walking around with your shoulders hunched up.
> Always use a chair with a backrest and sit with your feet flat on the floor or on a footrest. Don’t forget to change your sitting position every few minutes.
> “Know your limits.” If you’re using the right posture to lift something and still feel pain in your back or joints, stop lifting.





47 Comments