The Ulnar Nerve
Table of Contents
What is Ulnar Nerve?
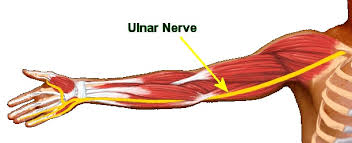
The ulnar nerve arises from C8-T1 nerve roots which form the medial cord of the brachial plexus. The cubital nerve travels down the hand where it moves behind the medial epicondyle of the humerus at the elbow. The nervous doesn’t give branches within the axilla or within the upper arm. It starts providing muscular and cutaneous branches within the upper forearm and hand. After the nerve passes behind the medial epicondyle, it enters the forearm between the 2 heads of the flexor carpi ulnaris muscle. The nervus ulnaris may become concentrated or irritated because it moves behind the medial epicondyle. The nervus ulnaris runs via the cubital tunnel that runs under the medial epicondyle. The nerve provides branches to the flexor carpi ulnaris and medial 1/2 flexor digitorum profundus
The nervus then runs beside the ulnar bone of the forearm into the wrist. because the nerve descends into the forearm, it stays medially above the flexor digitorum profundus and under the flexor carpi ulnaris giving branches to those muscles. within the lower part of the forearm, the nerve lies lateral to the flexor carpi ulnaris muscle and medial to the arteria ulnaris. The nervus ulnaris arrives in the palm of the hand via the Guyon canal. The nerve and artery move superficially to the flexor retinaculum.
At the wrist, the nervus lies just lateral to the wrist bone. The superficial branch of the nerve supplies and moves under the Palmaris brevis muscles and divides into palmar digital nerves. The deep branch of the nerve stimulates the three hypothenar muscles, the 2 medial lumbricals, the seven interossei, the adductor pollicis, and the deep head of the flexor pollicis brevis. It provisions all intrinsic hand muscles which lie medial to the flexor pollicis except the last lateral two lumbricals.
Anatomical Course of Ulnar Nerve
The nerve arises from the nerve plexus within the axilla region. it’s a continuity of the medial cord and includes fibers from spinal roots C8 and T1.
After arising from the plexus brachialis, the cubital nerve descends during a plane between the arterial blood vessel (lateral) and also the vena axillaris (medial). It returns down the medial part of the arm with the arteria brachialis situated laterally.
At the midpoint of the arm, the nervus ulnaris penetrates the medial fascial septum to enter the posterior compartment of the arm. It moves posterior to the elbow via the ulnar tunnel (small space between the medial epicondyle and olecranon). It also provides arise to an articular branch which supplies the cubital joint.
In the forearm, the nerve pains the 2 heads of the flexor carpi ulnaris, and runs deep into the muscle, beside the ulna. Three main branches arise within the forearm:
At the wrist, the nervus ulnaris travels superficially to the flexor retinaculum and is medial to the arterial blood vessel. It pain arrives in the hand through the ulnar canal (Guyon’s canal). within the hand, the nerve terminates by providing arise to superficial and deep branches.
Branches and innervation of Ulnar Nerve
In the forearm, the cubital nerve pierces the 2 heads of the flexor carpi ulnaris, and travels deep to the muscle, alongside the ulna. Three main branches arise within the forearm:
The cubital nerve usually doesn’t have any major branches within the arm. within the forearm, the nerve gives rise to articular branches, muscular branches, and therefore the palmar and dorsal cutaneous branches. within the hand, the nerve provides two terminal branches: the superficial branch nerve and the deep branch of the nerve.
Articular branches
As the cubital nerve passes between the medial epicondyle and olecranon and thru the cubital tunnel, it gives rise to articular branches that provide innervation to the ginglymoid joint.
Muscular branches
Two muscular branches emerge from the nervus ulnaris within the proximal forearm. These supply motor innervation to the flexor carpi ulnaris and also the medial half of the flexor digitorum profundus.
Palmar cutaneous branch
The palmar cutaneous branch arises from the nervus around the mid-portion of the forearm. This nerve runs along the arterial blood vessel to the distal forearm, where it perforates the deep fascia. It provides sensory innervation to the skin at the base of the medial palm, which overlies the medial carpal bones.
Dorsal cutaneous branch
The dorsal cutaneous branch of the cubital nerve emerges within the distal forearm, proximal to the wrist. This nerve route posteriorly, deep to the flexor carpi ulnaris and perforates the deep fascia to insert the medial aspect of the dorsum of the hand. Here, it divides into two or three dorsal digital nerves to produce sensation to the skin on the medial side of the dorsum of the hand yet because of the proximal regions of the medial 1½ digits (little finger and half the ring finger).
Superficial branch of nervus ulnaris
The superficial branch of the nervus ulnaris supplies sensory innervation to the anterior aspect of the ulnar 1½ digits (little finger and half the ring finger) and medial palmar skin. Additionally, it provides motor innervation to the palmar brevis muscle within the hypothenar region of the hand. It arises from the nerve just distal to the pisiform and infrequently divides into two palmar digital nerves.
Deep branch of nervus ulnaris
The deep branch of the nerve emerges from the identical region of the nerve because of the superficial branch. It courses between the muscles of the hypothenar region into the deep aspect of the palm, alongside the deep palmar branch of the arterial blood vessel. This nerve provides motor innervation to the overwhelming majority of hand muscles. These involve all the interossei (3 palmar and 4 dorsal), the hypothenar muscles (abductor, flexor, and opponens digiti minimi muscles), the medial two lumbricals, the deep head of flexor pollicis brevis and adductor pollicis.
To summarize, the nervus supplies motor innervation to the flexor carpi ulnaris, the medial half of the flexor digitorum profundus, and every one of the intrinsic hand muscles with the exception of the muscles such as lateral two lumbricals, opponens pollicis, abductor pollicis brevis, and flexor pollicis brevis.
The nerve provides sensory supply to the subsequent areas of the hand:
- The skin of the palmar and dorsal part of the medial 1½ digits and close palm.
- The skin on the medial side of the dorsum of the hand.
The nervous could be a major peripheral nerve of the upper limb.
Structure
The nerve gives motor innervation to a part of the forearm and the majority of the hand. It provides sensory cutaneous innervation to the medial forearm, medial wrist, and medial one and one-half digits. The nervus ulnaris and its branches send motor innervation to the flexor carpi ulnaris and flexor digitorum profundus within the forearm, and hypothenar muscles (opponens digiti minimi, abductor digiti minimi, and flexor digiti minimi brevis). Within the hand, the cubital nerve gives motor innervation to the third and fourth lumbricals, dorsal interossei, palmar interossei, adductor pollicis, flexor pollicis brevis, and palmaris brevis.
Functions of Ulnar Nerve
Motor Functions
The cubital nerve innervates muscles within the anterior compartment of the forearm, and within the hand.
Anterior Forearm
In the anterior forearm, the muscular branch of the nerve supplies two muscles:
Flexor carpi ulnaris – adducts and flexes the hand at the wrist.
Flexor digitorum profundus (medial half) – flexes the ring and pinky fingers at the distal hinge joint
The remaining muscles within the anterior forearm are innervated by the median nerve.
Hand
The majority of the intrinsic hand muscles are stimulated by the deep branch of the ulnar nerve:
- Hypothenar muscles ( opponens digiti minimi, flexor digiti minimi brevis, abductor digiti minimi)
- Medial two lumbricals
- Adductor pollicis
- Palmar and dorsal interossei of the hand
- The palmaris brevis is an irregularity to the offer rule and is stimulated by the superficial branch of the nerve. The opposite muscles of the hand (lateral two lumbricals and also the thenar eminence) are stimulated by the median nerve.
Sensory Functions
There are three branches of the nerve that are chargeable for its sensory innervation.
Two of those branches arise within the forearm, and travel into the hand:
- Palmar cutaneous branch – innervates the medial half of the palm.
- Dorsal cutaneous branch – innervates the dorsal surface of the medial one and a half fingers, and also the associated dorsal hand area.
- The last branch arises within the hand itself
Superficial branch – stimulates the palmar surface of the medial one and a half fingers.
Nerves
The nerve bears both sensory and motor fibers from the C8 and T1 dorsal rami. The nerve route along the medial arm from the anterior to the posterior compartment, via the medial intermuscular septum, is called the arcade of Struthers. The portico is formed by the medial head of the biceps, medial intermuscular septum, and internal brachial ligament. Then it runs posterior to the medial epicondyle of the humerus, providing off its first branch giving vestibular to the articulatio cubiti. At the distal elbow, the nervus ulnaris passes underneath Osbourne’s ligament (retinaculum between the 2 heads of the flexor carpi ulnaris muscle). Then It remains via the flexor and pronator muscles of the forearm and into the wrist, superficial to the flexor retinaculum. The nervus arrives at the hand via Guyon’s canal, a fibro-osseous tunnel formed by the pisiform and hook of the hamate bone. Within the hand, the cubital nerve branches give rise to a palmar cutaneous and dorsal cutaneous branch. The dorsal cutaneous nerve branches are further divided into radial and ulnar branches giving sensation to the dorsal hand.
Muscles
The cubital nerve stimulates the flexor muscles of the forearm involving the flexor carpi ulnaris and flexor digitorum profundus. It also enables the intrinsic muscles of the hand involving the palmaris brevis, lumbricals, hypothenar, and interossei muscles. Within the hand, the superficial branch of the nervus ulnaris stimulates palmaris brevis muscle and sensory to the hypothenar muscles, the fourth usual digital nerve, and ulnar proper nerve. The deep branch stimulates hypothenar muscles, opponens digiti minimi, interosseous muscles, third and fourth lumbricals, adductor pollicis, and medial head of the flexor pollicis brevis.
Physiologic Variants
Anatomical variants are important to spot to promptly and properly diagnose nerve dysfunction to stop the delay of treatment. Two nerve variations include Martin-Gruber and Riche-Cannieu anastomoses.
Martin-Gruber anastomosis could be a communication between the median and nervus ulnaris within the forearm anywhere distal to the medial epicondyle. With this anatomical variation, the motor nerves stimulating the intrinsic ulnar muscles are bears by the anterior interosseous branch of the median nerve. within the middle forearm, these fibers leave the anterior interosseous nerve to difficulty the nerve. Therefore, with this variation, patients can present with functional intrinsic hand muscles in spite of dysfunction of the nervus.
Riche-Cannieu anastomosis occurs when the median and ulnar nerves connect within the palm. This variant displays as motor fibers that are typically carried by the median nerve, now carried by the cubital nerve to the hand and then cross over within the palm. this can be clinically significant within the setting of carpal tunnel syndrome. Patients with progressive median nerve pathology could have normal function of the quality median nerve distribution.
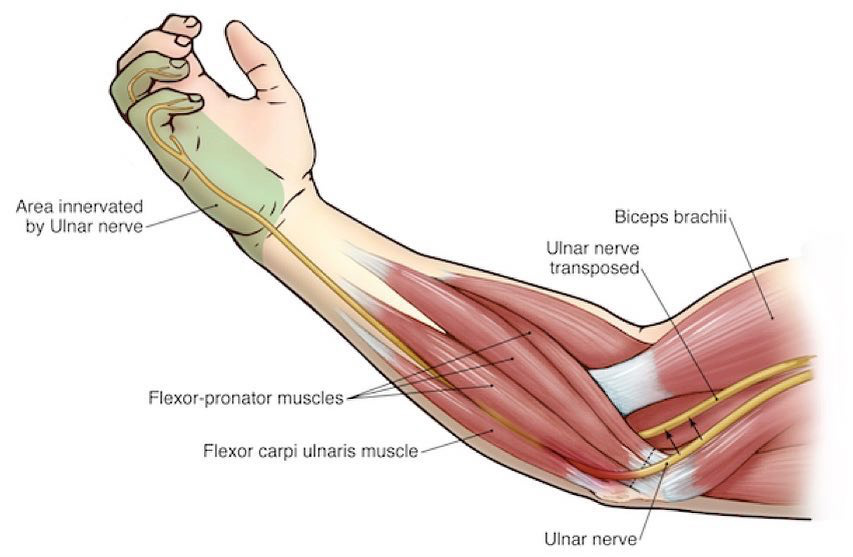
Surgical Considerations
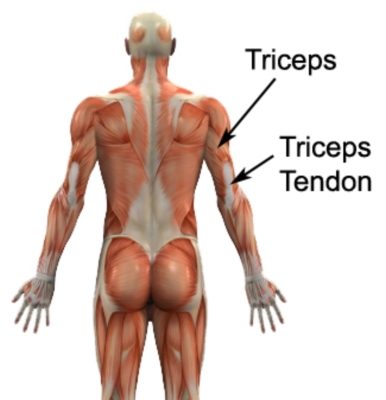
The most common site of cubital nerve entrapment is at the elbow within the cubital tunnel. Cubital tunnel decompression with possible nerve transposition could be a relatively common orthopedic procedure. The cubital tunnel is comprised of Osbourne’s ligament (cubital tunnel retinaculum) and also the deep layer of the aponeurosis of the two heads of the flexor carpi ulnaris muscle. Osbourne’s ligament is the proximal roof of the cubital tunnel and prevents subluxation of the nerve with elbow flexion. In surgical decompression for cubital tunnel syndrome, Osbourne’s fascia is incised to alleviate pain and paresthesia caused by nerve injury. Transposition of the nerve from the arcade of Struthers to the flexor carpi ulnaris is additionally one of the recommended surgical treatments. The arcade of Struthers is made by the inner brachial ligament, medial head of the triceps, and medial intermuscular septum just proximal to the medial epicondyle of the humerus. this can be another possible site of nerve compression.
Another surgical consideration includes incidental cubital nerve damage during carpal tunnel release surgery. During surgical intervention for carpal tunnel syndrome, a little incision is formed near the wrist crease. The surgeon will dissect through the soft tissues of the wrist down the transverse carpal ligament to alleviate compression of the median nerve. Damage to the deep motor branch of the nerve can occur during this dissection because the branch courses are just medial to the carpal tunnel along the hamate wrist bone. Although nervous damage could be a rare complication of carpal tunnel release surgery, it’s important for the incision to stay in line with the radial border of the ring finger.
Clinical Significance
Ulnar nerve Injury
Ulnar nerve injuries are quite common and may occur at various sites along their course through the upper limb. The usual places of injury or compression involve the posterior to the medial epicondyle, the cubital tunnel, and Guyon’s canal. Injuries to the nerves are characterized by paresthesia (tingling), numbness, and reckoning the severity may lead to considerable impairment of both motor and sensory functioning within the hand.
The feature show of a nerve injury is the “claw hand”. Individuals with this deformity have hyperextension of the metacarpophalangeal joints (due to the shortage of innervation to the medial two lumbricals and also the unopposed action of the extensors of this joint) and flexion of the interphalangeal joints of 4th and 5th fingers, due to the unrestricted action of the flexor digitorum profundus. The severity of this deformity, however, depends on the placement of the injury. Higher (proximal) injuries, like at the elbow, may denervate the ulnar a part of flexor digitorum profundus such the flexed appearance might not be apparent.
Sensory loss following a nervus ulnaris injury also depends on the location of the injury. this is often normally determined by assessing the function of the dorsal cutaneous branch which arises within the distal forearm and supplies the medial side of the dorsum of the hand.
Usually, the more proximal a nerve injury, the more serious it’s. the other is true after we consider the nerve. this is often because the flexor digitorum profundus (in the forearm) that flexes the fingers is partially innervated by the nerve. A proximal injury transfers stimulation to both the forearm muscles and hand muscles. A distal injury, on the opposite hand, only denervates the hand muscles; hence the still functioning finger flexors give the patient a pronounced clawed appearance within the ring and tiny fingers. With a proximal injury ensuing in an open palm, there is more ability for hand function. This phenomenon is specified as the ulnar paradox.
Proximal cubital nerve compression often occurs when someone rests their elbow on the table for a protracted time, or on a window (for long-distance drivers). It also can occur as an athletic injury, particularly in throwing athletes e.g. baseball pitchers, cricketers, and javelin throwers. The rapid movement of the ginglymus from flexion into whip-like extension can lead to compression of the nerve.
Cyclists often suffer nerve problems as they rest the medial border of their hand on their handlebars, leading to the compression of the hamate and so distal nerve compression (handlebar neuropathy).
Klumpke palsy
Klumpke palsy is the indication of a lower trunk injury to the nerve plexus. most ordinarily, lower trunk injuries are a result of an upward force on an infant’s arm or upward traction on the arm in an adult. Injury can even be a result of traumatic vaginal delivery with the traction of a baby’s abducted arm because of a large birth weight infant or small passage. Klumpke palsy includes a functional deficit of the intrinsic hand muscles presenting clinically with a whole claw hand. Clinically, observe hyperextension of MCP joint because of loss of flexors, radial deviation of the wrist because of loss of flexor carpi ulnaris, and wasting of intrinsic hand muscles such as lumbricals, interossei, thenar, and hypothenar muscles with flexion of the distal interphalangeal and proximal interphalangeal joints. This syndrome is additionally called straphanger’s syndrome.
Horner syndrome (ptosis, miosis, and anhidrosis) can occur thanks to the loss of sympathetic input from T1.
The most common site of nervus ulnaris injury is near the elbow. Nerve pathology will be caused by anatomic damage from fracture of the medial epicondyle, osteophyte infection, soft tissue mass, or synovitis at the ginglymoid joint. The nerve may additionally be damaged thanks to compression from prolonged periods of elbow flexion like sleep, exercise, driving, typing, or talking on the phone. Cubital tunnel syndrome could be a peripheral neuropathy thanks to chronic compression or repetitive trauma of the nervus ulnaris at the elbow between the medial epicondyle of the humerus and also the appendage of the ulna.
Congenital laxity of the cubital tunnel retinaculum may be seen, resulting in hypermobility of the nervous. this could result in repetitive subluxation and possible anterior dislocation when the elbow is flexed. Repetitive trauma at this location may lead to inflammation from recurrent friction over the medial epicondyle.
Ulnar nerve impingement can even occur at the wrist because of compression through Guyon’s canal, local trauma, ganglion cysts, and external neurological disease. The nervus ulnaris and artery enter Guyon’s canal, a fibro-osseous tunnel formed by the pisiform and hook of the hamate. The nervus ulnaris bifurcates within the canal into superficial and deep branches. neurological disorders at the wrist may be caused by bikers with excess pressure from handlebars and prolonged compression while typing at a desk.
Diagnosis of nervus ulnaris injury is often made with a radical history and musculoskeletal and neurological physical exam. However, EMG and nerve conduction studies will be used as an adjunct so as to diagnose and localize the lesion.
The nervus ulnaris could be a major peripheral nerve of the upper limb.
In this article, we shall have a look at the anatomy of the cubital nerve – its anatomical course, motor and sensory functions, and its clinical correlations.
Froment’s Sign
Froment’s sign may be a test for nervus ulnaris palsy – specifically paralysis of the adductor pollicis:
The patient is asked to carry a bit of paper between the thumb and finger because the paper is pulled away.
They should be ready to hold the paper there with no difficulty (via adduction of the thumb).
A test is positive when the patient is not able to adduct the thumb. Instead, they flex the thumb at the ginglymoid joint to undertake to keep up a hold on the paper.
Damage to the Elbow
Mechanism of injury: Trauma at the amount of the medial epicondyle (e.g. isolated medial epicondyle fracture, supracondylar fracture). It may be compressed within the cubital tunnel.
Motor functions:
All the muscles innervated by the cubital nerve are affected.
Flexion of the wrist can still occur but is in the course of abduction (due to paralysis of flexor carpi ulnaris and medial half flexor digitorum profundus).
Abduction and adduction of the fingers cannot happen, due to paralysis of the interossei.
Movement of the 4th and 5th digits is defective, due to paralysis of the medial two lumbricals and hypothenar muscles.
Adduction of the thumb is damaged, and the patient will have a positive Froment’s sign, due to paralysis of adductor pollicis.
Sensory functions: All sensory branches are affected, so there’ll be a loss of sensation over the parts that the nerve stimulates.
Characteristic signs: Patient cannot grip paper between fingers, positive Froment’s sign, wasting of hypothenar eminence.
Damage to the Wrist
Mechanism of injury: Lacerations to the anterior wrist.
Motor functions:
Only the intrinsic muscles of the hand are impacted.
Abduction and adduction of the fingers cannot occur, because of paralysis of the interossei.
Movement of the 4th and 5th digits is broken, thanks to paralysis of the medial two lumbricals and hypothenar muscles.
Adduction of the thumb is impacted, and the patient will have a positive Froment’s sign, to paralysis of adductor pollicis.
Sensory functions: The palmar and superficial branches are generally severed, but the dorsal branches aren’t impaired. This ensuring in sensory loss over the palmar side of the medial one and a half fingers only.
Characteristic signs: Patient cannot properly grip paper placed between fingers, which means Froment’s sign is positive, wasting of the hypothenar eminence
Clinical Relevance
The cubital nerve is most at risk of injury at the elbow and therefore the wrist leading to varying degrees of motor and sensory loss. Mechanism of injury involves local trauma, nerve impingement, lacerations at the wrist, and Guyon canal cyst. Feature signs of injury to the ulnar nerve are the inability to grip paper between the fingers with long-term cases leading to ulnar claw hand deformity.
There are two complications including the cubital nerve or its branches:
- Cubital Tunnel Syndrome
- Guyon canal syndrome
The following clinical features will characterize the cubital nerve injury:
- flattening of the medial border of the forearm
- sensation loss at distal interphalangeal joints of 4th and 5th digit
- loss of hypothenar eminence
- loss of adduction of the thumb
- loss of abduction of fingers
- marked clawing of 4th and 5th digits
- slight clawing of 4th and 5th digit
- sensory, trophic, and vasomotor changes
- adduction of the thumb
Diminished sensation:
- Palmar surface of the one and a half fingers medially.
- Dorsal surface of the one and a half fingers medially.
Neurodynamics
The upper limb neurodynamic test for the ulnar nerve(ULNT3) is done with the patient supine. The joints are transferred sequentially and to the tip of the range or until symptoms are produced. Patients are to be educated to report the onset of any sensation like a stretch, tingling, or pain anywhere within the arm or neck.
ULNT3 sequencing:
- Shoulder external rotation
- Shoulder girdle depression
- Shoulder abduction
- Wrist and Finger extension
- Elbow flexion
- Shoulder abduction
FAQ
What does the nervus ulnaris control?
The cubital nerve transmits electrical signals to muscles within the forearm and hand. The cubital nerve is additionally to blame for sensation within the fourth and fifth fingers (ring and tiny fingers) of the hand, a part of the palm, and also the underside of the forearm.
What are the symptoms of cubital nerve damage?
Symptoms
Abnormal sensations within the pinky and a part of the finger, usually on the palm side.
Weakness, loss of coordination of the fingers.
Clawlike deformity of the hand and wrist.
Pain, numbness, decreased sensation, tingling, or burning sensation within the areas controlled by the nerve.Can the nerve repair itself?
While cubital nerve entrapment is typically not serious, it can have permanent consequences without prompt treatment, including paralysis and loss of feeling within the affected hand or arm. However, with proper diagnosis and treatment, the general public with nervous entrapment can make a full recovery.
How long does a nervus go to heal?
Ulnar Nerve Release Estimated Recovery Timeline
Recovery from cubital tunnel release surgery varies from patient to patient, taking anywhere from several weeks to many months. Symptoms like numbness or tingling may improve quickly or may take up to 6 months to travel away.How does one have it away from nervous pain?
Consider sleeping on your back together with your arms at your sides or on pillows to stay your elbows and wrists in a perfect position. don’t fold them across your chest.
Will an elbow brace help the ulnar nerve?
Wearing a cubital tunnel syndrome brace can help reduce ulnar nerve-related pain or symptoms including numbness or tingling of your annualry and pinky finger (carpal tunnel symptoms of the arm affect the opposite fingers), weakening grip and finger coordination, and muscle wasting of the hand.



17 Comments