Guyon Canal Syndrome (Ulnar tunnel syndrome)
Table of Contents
What is a Guyon Canal Syndrome?
Guyon Canal syndrome, also known as ulnar tunnel syndrome or ulnar neuropathy at the wrist, is a condition that affects the ulnar nerve as it passes through a narrow space called the Guyon’s canal.
- Guyon canal syndrome is mainly also known as ulnar tunnel syndrome or handlebar palsy. It is defined as a compression of the distal ulnar nerve at the level of the wrist as it enters the hand through a space also called the ulnar tunnel or Guyon canal. The clinical presentation can be purely sensory, purely motor, and both depending on the location of the nerve compression. The ulnar nerve is one of the main major nerves of the hand and travels down the neck through the medial epicondyle, then passes under the forearm muscles and then to the little finger alongside the palm.

Clinically Relevant Anatomy
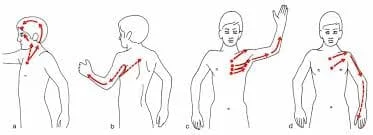
- The ulnar nerve emerges from the medial cord (C8-T1) of the brachial plexus, it travels into the axilla and passes into the anterior compartment of the arm, then it pierces the intramuscular septum or travels in the mainly posterior compartment. It then runs posterior to the medial epicondyle of the Humerus into the cubital fossa. The nerve then passes between the main flexor carpi ulnaris and the main flexor digitorum profundus muscles.
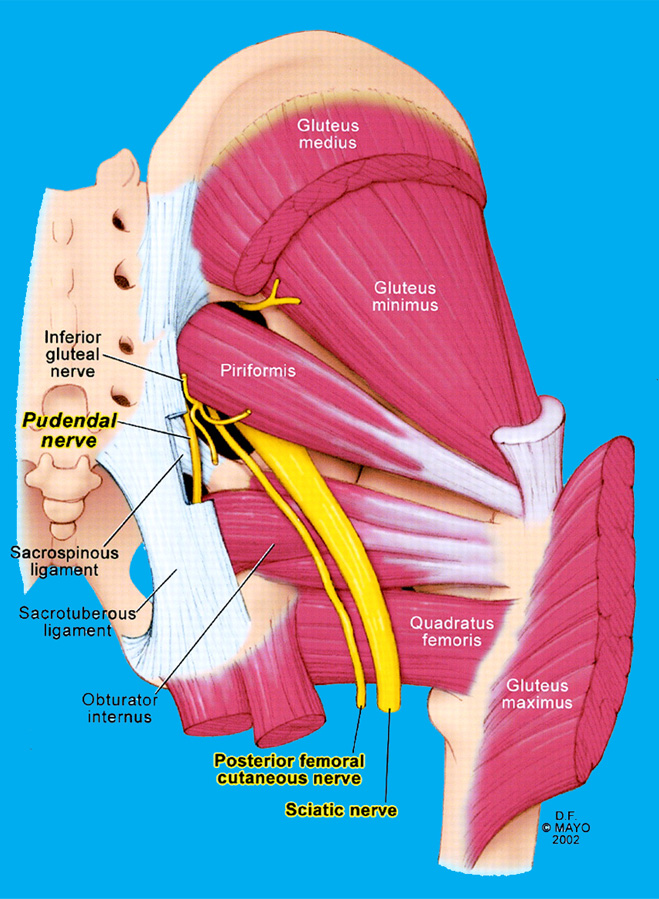
- The main ulnar nerve gives off a dorsal cutaneous branch 8.3 cm proximal to the pisiform bone before it enters Guyon’s canal. The main Guyon Canal extends between the proximal border of the pisiform bone and distally at the hook of the hamate. The ulnar nerve and ulnar artery travel through the Guyon canal as they enter from the distal forearm to the main hand.
The boundaries of the Guyon Canal are:
- Roof: palmar carpal ligament, or hypothenar connective tissue.
- Floor: transverse carpal ligament, isogametes ligament, metacarpal ligament, flexor digitorum profundus tendons, or opponens digit minimi
- Medial wall: pisiform, abductor digit mini, and mainly flexor carpi ulnaris tendon.
- Lateral wall: hook of hamate, transverse carpal ligament, or the flexor tendons.
Causes of Guyon Canal Syndrome:
- Injury to the distal ulnar nerve can be due to compression, trauma, inflammation, and vascular insufficiency
- Ganglion cysts, they’re one of the very common causes of Guyon canal syndrome
- Tumors
- Anatomical anomalies can be the hypertrophic muscle of normal anatomy and an unusual location
- Ulnar artery thrombosis and aneurysm (e.g., Hypothenar Hammer Syndrome)
- Fractures and dislocations (e.g., The hook of hamate Fracture/Displacement)
- A repetitive micro injury such as repetitive trauma to the hypothenar by the handlebar in cyclists)
- The Carpel tunnel syndrome can lead to anatomical changes in the ulnar tunnel leading to functional impairments
- Iatrogenic
Epidemiology:
- The very commonly reported cases of Guyon canal syndrome are due to a ganglion cyst and repetitive trauma. However, the incidence of Ulnar tunnel syndrome in the general population has not yet been accurately estimated due to the lack of research.
Pathophysiology:
Zone 1: proximal to the motor and sensory bifurcation
- Area of the distal portion of the mostly ulnar nerve (main trunk) before it splits into its superficial sensory or deep motor divisions
- Etiologies include hook of hamate fracture/malunion/nonunion and ganglion cysts
- Zone 1 main Guyon canal injury to the mostly ulnar nerve results in both motor and sensory symptoms
Zone 2 (most commonly affected): distal to the motor and sensory bifurcation, or radial to zone 3
- Corresponds to the main deep terminal motor branch of the ulnar nerve, if affected, it produces only main motor symptoms (e.g.weakness)
- Etiologies include hook of hamate fracture/malunion/nonunion and ganglion cysts
- This main deep branch of the ulnar nerve innervates all the interosseous muscles, fourth or fifth lumbricals, hypothenar muscles (opponens digit mini, abductor digit mini, flexor digit mini brevis), or adductor pollicis muscle.
Zone 3: distal to motor/sensory bifurcation, or ulnar to zone 2
- The superficial sensory terminal branch of the ulnar nerve is compressed in this area leading to sensory symptoms only such as numbness or tingling, and burning sensation.
- Causes include main ulnar artery aneurysm and/or thrombosis
Symptoms of Guyon Canal Syndrome:
The symptoms of Guyon Canal syndrome can vary in severity and may include:
- Numbness or tingling: The most common symptom is a sensation of numbness or tingling in the ring finger and little finger. This sensation may extend to the palm side of the hand.
- Weakness: Weakness in the hand, specifically in the muscles that control the ring finger and little finger, may occur. This can result in difficulty with tasks that require fine motor skills, such as gripping objects, writing, or typing.
- Loss of dexterity: Decreased dexterity and coordination in the affected hand may be experienced. Tasks that involve precise movements of the fingers, such as buttoning clothes or manipulating small objects, may become challenging.
- Pain or discomfort: Some individuals may experience pain or discomfort in the hand or wrist. The pain can be sharp, throbbing, or aching in nature and may worsen with activities that involve wrist movement or pressure on the affected area.
- Hand clumsiness: Due to the weakness and altered sensation in the hand, individuals with Guyon Canal syndrome may have difficulty with tasks requiring fine motor skills, resulting in a sense of clumsiness or dropping objects more frequently.
It’s important to note that symptoms may worsen or become more noticeable during activities that involve repetitive wrist movements or prolonged pressure on the affected area.
- pain or paresthesias in ulnar 1-1/2 digits
- weakness to intrinsics, ring or small finger digital flexion, and thumb adduction
Diagnosis:
Physical exam:
- inspection and palpation
- clawing of ring or little fingers
- caused by loss of intrinsics flexing the MCPs or extending the IP joints
Allen test:
- helps mainly diagnose ulnar artery thrombosis
Neurovascular exam:
- ulnar nerve palsy results in paralysis of the main intrinsic muscles (adductor pollicis, deep head FPB, interossei, or lumbricals 3 or 4)
- weakened grasp
- loss of MP joint flexion power
- weak pinch
- loss of thumb adduction
Froment sign:
- IP flexion compensates for the loss of thumb adduction when attempting to hold a piece of paper
- loss of MCP flexion or adduction by adductor pollicis (ulnar n.)
- compensatory main IP hyperflexion by FPL (AIN)
Jeane’s sign:
- a compensatory thumb MCP hyperextension or thumb adduction by EPL (radial n.)
- compensates for main loss of IP extension or thumb adduction by adductor pollicis (ulna n.)
Wartenberg sign:
- abduction posturing of the mainly little finger
Imaging Studies
- A hand x-ray and computed tomogram (CT) scan can be used to evaluate for fractures (especially hamate fractures).
- Magnetic resonance imaging of the hand can show anatomical variations within the Guyon canal or evaluate for structures responsible for mechanical compression of the ulnar nerve (e.g., lipomas, ganglion cysts, and aberrant muscle).
- Angiography can be used for the evaluation of ulnar artery aneurysms and thrombosis.
- Electromyography (EMG) or nerve conduction velocity (NCV) are used to assess peripheral nerve compromise or localize the level at which the nerve is affected (i.e., differentiate between ulnar nerve entrapment within Guyon canal at the wrist vs. cubital tunnel at the elbow vs. main C8-T1 radiculopathy).
Treatment of Guyon Canal Syndrome:
- The decision to choose conservative vs. main surgical management depends on the duration and severity of symptoms, as well as the exact etiology determined to be the main cause of the symptoms. Such as Professional athletes mainly baseball players are at risk of injury mainly hook of hamate fractures that can occur mainly due to acute trauma and repetitive injury during the performance. In this setting, the general consensus of hand surgeons is to perform a main isolated hook of hamate incision, which has reliably demonstrated low/minimal rates of postoperative complications, return to play within 3 to 4 weeks, or have high patient satisfaction scores.
General Considerations:
- Treatment of Guyon canal syndrome is similar to that of main carpal tunnel syndrome. Its spectrum consists of conservative management or surgical decompression. Conservative management involves patient instructions or splinting. Instructions are centered around the avoidance of mechanical compression or repetitive stress at the Guyon canal. In the case of cyclists, the utilization of many ergonomically favored handlebar positions can be used. Repetitive or prolonged wrist extension movement should be minimized as this exerts compressive forces on the main ulnar nerve in the hand.
- Wrist splinting must keep the wrist in a main neutral position but may allow fingers to move around freely. A splint is to be worn at least at night for a recommended duration of one or 12 weeks.
- According to a European Handguide study published in the British Medical Journal, an expert panel of medical professionals had reached a consensus of utilizing conservative management for symptoms that are mild to moderate in severity and with acute to subacute duration lasting up to mainly three months. For moderate to severe symptoms lasting three months and longer surgical decompression was favored. Surgical treatment may also include main post-surgical exercises, especially in those with a reduced range of motion at the joint. Post-operative splinting was not required always However it can be used in those patients who have a habit of loading the affected wrist joint.
- Additional treatments that can be used include therapeutic ultrasound or nerve gliding exercises. In the case of ulnar artery thrombosis and an aneurysm (hypothenar hammer syndrome), asymptomatic patients do not have to be treated surgically. However, when symptomatic, treatment will mainly range from antiplatelet medication to surgical correction e.g., bypass
Techniques:
- Local surgical decompression
- release hypothenar muscle origin
- decompress ganglion cysts
- resect hook of hamate
- vascular treatment of main ulnar artery thrombosis
- explore or release all three zones in main Guyon’s canal
- Tendon transfers
- correct claw fingers
- mostly used grafts are ECRL, ECRB, and palmaris longus muscle
- tendons must pass volar to the transverse metacarpal ligament in order to flex the main proximal phalanx
- attach to the A2 pulley of the ring or small fingers using a two-tailed or four-tailed graft.
- restore power pinch
- Smith transfer using ECRB or FDS of the ring finger
- restore adduction of the small finger
- transfer ulnar insertion of EDM to A1 pulley and radial collateral ligament of the small finger
Physiotherapy Treatment in Guyon Canal Syndrome
Physiotherapy plays a significant role in the management of Guyon Canal syndrome. The goals of physiotherapy treatment for Guyon Canal syndrome include relieving symptoms, improving hand function, reducing pain, and preventing further progression of the condition. Here are some common physiotherapy interventions that may be employed:
- Splinting: Wearing a splint or brace that immobilizes the wrist in a neutral position can help relieve pressure on the ulnar nerve and reduce symptoms. A physiotherapist can provide custom-made or off-the-shelf splints to support the wrist and hand.
- Nerve gliding exercises: Specific exercises that involve gentle and controlled movements of the wrist, fingers, and thumb can help mobilize and glide the ulnar nerve within the Guyon’s canal. These exercises can promote nerve flexibility, reduce adhesions, and improve nerve function.
- Strengthening exercises: Strengthening the muscles of the hand, particularly those responsible for grip and finger movements, can enhance hand function and compensate for any weakness resulting from Guyon Canal syndrome. A physiotherapist can prescribe targeted exercises using hand grippers, resistance bands, or therapy putty.
- Range of motion exercises: Gentle stretching and range of motion exercises for the wrist, fingers, and thumb can help maintain joint mobility and prevent stiffness or contractures.
- Ergonomic modifications: Assessing and modifying the patient’s work or daily activities to optimize wrist and hand positioning can alleviate strain on the ulnar nerve. A physiotherapist can provide recommendations on proper ergonomics, such as adjusting workstation setup or using ergonomic tools.
- Pain management techniques: Various pain management modalities may be employed, including heat or cold therapy, ultrasound, transcutaneous electrical nerve stimulation (TENS), or manual therapy techniques, to reduce pain and promote tissue healing.
- Education and activity modification: Educating the patient about the condition, its causes, and strategies to prevent aggravation of symptoms is important. The physiotherapist may provide guidance on activity modification, such as avoiding repetitive wrist movements or using protective padding during activities that put pressure on the wrist.
It’s important to note that the specific treatment approach may vary depending on the individual’s symptoms, severity of the condition, and response to therapy. A physiotherapist will perform a thorough assessment and develop a personalized treatment plan tailored to the patient’s needs.
Differential Diagnosis:
- Alcohol-related neuropathy
- Amyotrophic lateral sclerosis
- Brachial plexus abnormalities
- Cervical disc disease
- Cervical spondylosis
- Epicondylitis
- Pancoast tumor
- Thoracic outlet syndrome
- Traumatic peripheral nerve lesions
Other Issues:
- Guyon canal syndrome is a relatively uncommon mainly ulnar neuropathy. Diagnosis can be challenging due to the variety of presenting signs or symptoms depending on the exact location of nerve compression in addition to the individual anatomic variations within the Guyon canal itself. Although there are several articles suggesting approaches to the diagnosis or management of Guyon canal syndrome, due to a lack of large-scale empirical studies comprehensive guidelines have not yet been firmly established. For example, when a patient suspected of Guyon canal syndrome should be prescribed an MRI.
Enhancing Healthcare Team Outcomes:
- Guyon canal syndrome is a rare neurological disorder of the hand that is very common in young people. The disorder is difficult to diagnose or requires an interprofessional team that includes a hand surgeon, radiologist, neurologist, neuro/orthopedic surgeon, or therapist.
FAQ:
The ulnar nerve or ulnar artery passes through the Guyon canal as they pass from the distal forearm to the hand.
Guyon’s canal main syndrome is an entrapment of the ulnar nerve as it passes through a tunnel in the wrist called Guyon’s canal.
It is similar to carpal tunnel syndrome but involves the nerve is different. Sometimes both conditions can cause a
the main problem on the same hand.
Guyon’s canal main syndrome refers to the compression of the ulnar nerve while it passes from the wrist into the hand through a
space called the ulnar tunnel and Guyon’s canal. Guyon’s canal syndrome is also called main ulnar tunnel syndrome and handlebar
palsy.
Carpal tunnel syndrome symptoms mostly start gradually and symptoms are Tingling or numbness. You may notice tingling or numbness in the fingers or hand. Usually, the thumb and index, middle, and ring fingers are affected, but not the little finger.
Ulnar nerve paralysis is the main condition associated with closed fractures of the ulna of the forearm. In most cases, the cause of paralysis is nerve contusion, which is neuropraxia-type nerve lesion.
Electromyogram. Electrical testing of main ulnar nerve function often helps confirm a diagnosis or can indicate which treatment
is best for you. An electromyogram evaluates how the nerves or muscles work together by measuring the electrical impulse along
nerves, nerve roots, or muscle tissue.