Pseudoradiculoar Syndrome
Table of Contents
Definition
“Pseudoradicular syndromes” refer to clinical conditions that cause pain in the lower limb area or upper limb area, involving the same areas of the nerve root dermatomes but not directly affecting the nerve roots in the body. These syndromes can be caused by various diseases, some of which are relatively rare.
The term “pseudo radicular” distinguishes this condition from true radiculopathy, where the symptoms are caused by a specific nerve root being affected. The pseudo-radicular syndrome often presents with similar symptoms to radiculopathy, including pain, tingling, and numbness. or weakness in a specific region of the body.
Classification
The pseudo-radicular syndromes are subdivided into two main groups based on their underlying mechanisms:
Pseudoradicular syndromes due to reflex mechanisms: This includes conditions like zygapophyseal joint syndrome (a problem with the facet joints of the spine), iliolumbar syndrome (involving the iliolumbar ligament and related structures), and hip joint pathology.
Pseudoradicular syndromes due to pathology of an anatomical structure in the lower limb: This group includes conditions like fibromyalgia, myofascial pain syndromes, tendinopathies of the lower limbs, fascia lata and iliotibial band pathology, piriformis syndrome (involving the piriformis muscle and sciatic nerve), ischial tuberosity fracture, and peripheral nerve entrapment.
Cause of Pseudo radicular Syndrome
- Muscle imbalance: An imbalance in muscle strength or flexibility can lead to abnormal movement patterns and increased stress on surrounding structures, including nerves. This can result in symptoms that mimic pseudo-radicular pain.
- Trigger points: Trigger points are localized areas of muscle tightness and tenderness that can refer to pain in other parts of the body.
- Myofascial pain syndrome: This condition involves the development of trigger points and muscle pain in specific muscle groups.
- joint dysfunction: Dysfunctional joints, such as spinal facet joints, sacroiliac joints,s or other joints in the body, can cause referred pain that mimics pseudo radicular syndrome.
- ligamentous strain: Injury or strain to the ligament surrounding the spine or joints can cause pain that radiates along the nerve pathway, leading to psedoradicular syndrome.
Sign of Pseudo radicular Syndrome
Buttock pain
Sciatica-like pain
Numbness and tingling
Muscle Weakness
Pain with specific movement
Symptoms of the Pseudo radicular Syndrome
- radiating pain
- numbness or tingling
- muscles weakness
- changes in reflex
- sensitivity to touch
Type of Psedoradicular Syndrome
Piriformis syndrome: This syndrome occurs when the piriformis muscles, located in the buttocks, compress or irritate the sciatic nerve It can cause pain, tingling, or numbness in the buttocks and down the leg, similar to sciatica.
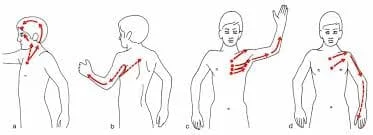
Thoracic outlet syndrome: arises from the compression of nerves or blood vessels in the thoracic outlet, which is the space between the collarbones and the first rib. It can lead to pain, numbness, or tingling in the neck, shoulder, arm, or hand.
Myofascial pain syndrome: involves the development of trigger points, which are hypersensitive knots in the muscles. These trigger points can cause referred pain mimicking radicular symptoms, even though the nerves are unaffected.
Fibromyalgia: Although fibromyalgia primarily causes widespread pain, it can also manifest with pseudo-radicular symptoms such as tin.
Diagnosis of Pseudo Radicular
- medical history
- physical examination
- diagnostic tests
Diagnosing the cause of radicular pain can be challenging, and even with advanced imaging techniques and collaboration among clinicians, neuro-radiologists, and neurosurgeons, there can still be room for error.
Treatment
Conservative Treatment
Initially, conventional treatments are usually attempted before considering more invasive interventions. These may include pain medication: Nonsteroidal anti-inflammatory drugs(NSAIDs)or analgesics may be prescribed to manage pain and inflammation.
Physical Therapy: Specific exercises and stretches could improve flexibility, strengthen the muscles, and decrease pain.
Physiotherapy treatment
Manual Therapy: Hands-on techniques performed by physiotherapists such as joint mobilization, soft tissue mobilization, and gentle spinal manipulation, can help reduce pain, improve joint mobility, and relieve muscle tension.
Therapeutic Exercise: Specific exercises are prescribed for strengthening the surrounding muscles, improving flexibility, and enhancing stability. These may include stretching exercises, core stabilization exercises, posture correction exercises, and targeted strengthening exercises for the affected area.
Nerve Mobilization: Specific techniques are used to mobilize and desensitize the nerve, helping to reduce symptoms such as pain, tingling, or numbness. Nerve gliding exercises and neural tension-reducing maneuvers are commonly employed.
Heat and cold Therapy: Apply Heat and cold to the affected area may provide temporary relief.
Posture correction: Maintaining good posture and ergonomics can help relieve pressure on the affected nerve roots.
Electrical stimulation: Techniques such as transcutaneous electrical nerve stimulation (TENs) or electrical muscle stimulation may be used to provide pain relief and reduce muscle spasms.
Ultrasound Therapy: Using ultrasound waves can help reduce pain and insufflation by promoting tissue healing and improving blood circulation.
postural education: Correcting poor posture is crucial for managing pseudo radicular syndrome. Your physiotherapist will provide education and guidance on maintaining proper posture during daily activities, including sitting, standing, and lifting.
Exercise for the pseudo radicular syndrome
Cat and camel stretch: start on your hands and knees. Slowly arch your back, upward, dropping your head and tailbone (cat pose). Then, lower your belly toward the floor, lifting your head and tailbone(camel pose). Repeat 10 times.

Piriformis stretch: Lie on the patient’s back with both knees bent. Cross one leg over the other, placing the ankle just above the knee of the opposite leg. When your buttock stretches, gently draw the uncrossed leg toward your chest. Hold for 20 to 30 on each side, repeating twice.

Hamstring stretch: Lie on the patient’s back with one leg extended. roll a towel or belt around the ball of the patient’s foot and gently pull the patient’s leg toward your chest, keeping the patient’s knee straight. Hold for 20 to 30 seconds on each side, repeating twice.

Pelvic tilt: Lie on the patient’s back with the patient’s knees bent and feet flat on the base. Slowly tilt the patient’s pelvis upward pressing the patient’s lower back into the base. Hold for a few seconds, then release. Repeat 10 times.

Bridging: Lie on the patient’s back with the patient’s knees flexed and feet flat on the base. Lift your hip off the ground. Then lower your hips back down. Repeat 10 times

Wall squats: Stands with your back against a wall and feet shoulder-width apart. Slide down the wall, bending your knees until you reach a seated position. Hold for 5 to 10 seconds, then push through the patient’s heels to stand back up. Repeat 10 times.

Clamshells: Lie on your side with knees bent and feet together, Keeping the patient’s feet together. keeping the patient’s feet touching, lifting the patient’s top knee while. Keeping feet together. Lower it back down. Repeat 10 times on each side.

Walking: Engage in regular walking for a least 30 min a day. Focus on maintaining good posture and taking even strides.

Surgical treatment
Surgical treatment might be considered as a last option. However, the specific surgical procedures for pseudo radicular syndrome can vary depending on the underlying cause and individual patient factors.
It is essential to consult with a spine specialist or neurosurgeon to determine the most appropriate surgical treatment option, if necessary, based on the individual case.
FAQ
What is the difference between radicular pain and Pseudoradicular pain?
The key difference lies in their underlying causes and the presence of nerve-root involvement. Radicular pain is due to nerve compression, while pseudoradicular pain results from non-nerve-related issues.
Pseudoradicular pain, on the other hand, mimics radicular pain but is not caused by nerve root compression. Instead, it originates from structures like muscles, ligaments, or facet joints in the spine while Radicular pain is caused by the compression or irritation of a spinal nerve root, often due to conditions like herniated discs or spinal stenosis.What activities should you avoid with pseudo radicular syndrome?
Avoid activities like hard lifting that aggravate the area’s symptoms to maintain it. Avoid too much rest. Stay active around the house, and go on walks several times per day. The movement would decline your pain and stiffness, and asses you feel better.
What is the primary symptom of pseudo radicular syndrome?
Sharp shooting pain in the back, arms, and legs that may worsen with certain activities, even something as simple as coughing or sneezing. Weakness or loss of reflexes in the legs. Numbness of the skin, “pins and needles,” or other abnormal sensations (paresthesia) in the legs
Can pseudo-radicular syndrome be cured?
Typically, radiculopathy is treatable without surgery. Depending on the severity, a doctor may recommend medication, including non-steroidal drugs, such as ibuprofen, aspirin, or naproxen. oral corticosteroids or injectable steroids.
Does pseudo-radicular pain follow a dermatome?
Classically, pseudo-radicular pain has been described as following a dermatomal distribution. Research has shown, however, that pseudo-radicular pain, whether caused by disk herniation or spinal stenosis, may not follow a dermatomal distribution.