Irritable hip syndrome
Table of Contents
What is an Irritable hip syndrome?
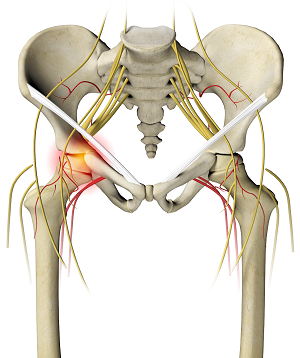
The irritable hip syndrome also known as transient synovitis of the hip is a self-limiting condition in which there is an inflammation of the inner lining of the capsule of the hip joint. The term irritable hip refers to the syndrome of acute hip pain, joint stiffness, limp or non-weight bearing, indicative of an underlying condition such as transient synovitis or orthopedic infections (like septic arthritis or osteomyelitis). In everyday clinical practice, however, irritable hip is commonly used known as transient synovitis. It should not be confused with sciatica nerve compression, a condition describing hip and lower back pain much more common in adults than transient synovitis but with similar signs and symptoms.
The irritable hip syndrome usually affects children between three and ten years old but it has been reported in a 3-month-old infant and in some adults. It is the most common cause of sudden hip pain and limping in young children. Boys are affected two to four times as more as girls. This exact cause is unknown.
An irritable hip syndrome is a diagnosis of exclusion. The diagnosis can be made in the typical setting of pain or limp in young children who are not generally unwell and have no recent trauma. There is a limited range of motion of the hip joint(R.O.M). Nevertheless, a child with irritable hip syndrome of the hip can usually weight bear. This is a vital clinical differentiating sign from septic arthritis. Blood tests may show mild inflammation. An ultrasound scan of the hip joint can show a fluid effusion(collection). Treatment is with nonsteroidal anti-inflammatory drugs and limited weight-bearing in the patient. The condition usually clears itself within 7 to 10 days, but a small group of patients will continue to have symptoms for several weeks. The recurrence rate is 4–17%, most of which is in the first six months.
Symptoms and signs of Irritable hip syndrome
The irritable hip syndrome causes pain in the hip, groin, thigh, or knee on the affected side of the body. Whereas, the child with an irritable hip syndrome of the hip can usually weight bear with varying degrees of limping. There might be a limp or abnormal crawling in infants with or without pain. In small children, the presenting complaint can be unexplained crying for example, when changing a diaper. The condition is nearly always limited to one side of the body. sometimes pain and limp can increase from mild to severe.
many children might have a slightly raised temperature; high fever and general malaise point to peers, these are more serious conditions. On clinical examination, the child typically holds the hip normally bent, turned outwards, and away from the middle line flexion, external rotation, and abduction. Active and passive movements might be limited because of pain, especially abduction and internal rotation. The hip could be tender to palpation. The log roll test involves gently rotating the entire lower limb inward and outward with the patient on his back, to check when muscle guarding occurs. The unaffected hip and the knees, ankles, feet, and spine are found to be really normal.
Complications
In the past, there have been speculations about possible complications after irritable hip syndrome. The current consensus however is that there is no proof of a raised risk of complications after irritable hip syndrome.
One such early suspected complication was coxa Magna, which is an overgrowth of the femoral head and broadening of the femoral neck, accompanied by changes in the acetabulum, which might lead to subluxation of the femur. There was also some controversy about whether continuous high intra-articular pressure in transient synovitis could cause avascular necrosis of the femoral head Legg-Calvé-Perthes disease, but early studies did not confirm any link between the two conditions.
Causes of Irritable hip syndrome
In the acute phase of transient synovitis, inflammation occurs in the synovial membrane that surrounds the hip. The underlying reasons for this are not still clear.
Diagnosis
There are no set standards for the diagnosis of the suspected irritable hip syndrome, so the number of investigations will depend on the have to exclude other, more serious diseases. It’s of great vital to exclude the diagnosis of septic arthritis. This is because if septic arthritis is missed in a child, grave complications can occur. The exclusion of septic arthritis is mainly built upon the physician’s clinical expertise and is supplemented by basic laboratory tests and relevant imaging modalities. Additionally, beware to exclude the diagnosis of acute osteomyelitis, because it’s not uncommonly cooccurring with septic arthritis of the hip in children.
Inflammatory parameters in the blood may be slightly raised these include erythrocyte sedimentation rate, C-reactive protein, and white blood cell count, but increased inflammatory markers are strong predictors of other more serious conditions such as septic arthritis.
X-ray imaging of the hip is more often unremarkable. Subtle radiographic signs include an accentuated pericapsular shadow, widening of the medial joint, lateral displacement of the femoral epiphyses with surface flattening Waldenström sign, prominent obturator shadow, diminution of soft tissue planes around the hip, or slight demineralization of the proximal femur joint. The main reason for radiographic examination is to exclude bony lesions such as occult fractures, slipped upper femoral epiphysis, or bone tumors such as osteoid osteoma. An anteroposterior and frog lateral Lauenstein view of the pelvis and both hip is advisable.
An ultrasound scan of the hip can easily demonstrate fluid inside the joint capsule Fabella sign, although it’s not always present in transient synovitis. Whereas, it can’t reliably distinguish between septic arthritis and transient synovitis. If septic arthritis has to be ruled out, needle aspiration of the fluid could be performed under ultrasound guidance. In transient synovitis, the joint fluid would be clear. In septic arthritis, there would be pus in the joint, which can be sent for bacterial culture and antibiotic sensitivity testing.
some advanced imaging techniques could be used if the clinical picture is unclear; the exact role of different imaging modalities remains uncertain. Many studies have demonstrated findings on magnetic resonance imaging MRI scan that can differentiate between septic arthritis and transient synovitis, for example, the signal intensity of adjacent bone marrow. Skeletal scintigraphy could be entirely normal in transient synovitis, and scintigraphic findings don’t distinguish transient synovitis from other joint conditions in a child. CT scanning does not appear helpful.
Differential diagnoses
Some conditions cause and symptoms similar to those of irritable hip, including:
- Perthes disease: This can damage the head of the femur, or thigh bone, by interrupting the blood supply to the hip joint.
- Fracture or contusion: Either of these injuries to the hip joint can cause it to flare up.
- A tumor in the hip joint: This can cause sensations similar to irritable hip joints.
- Juvenile idiopathic arthritis: This involve chronic joint inflammation with an unknown cause that occurs in children under 16 years of age. It can affect the hip joint.
Other possible issues include septic arthritis and osteomyelitis. Each can cause a very sick child to develop elevated C-reactive protein levels and sedimentation rates. Sedimentation is the process through which red blood cells separate from blood serum, and it is part of the inflammation mechanism. The body sends out C-reactive protein in response to inflammation, which is why raised rates occur with irritable hip symptoms.
Non-surgical treatment for Irritable hip syndrome
An irritable hip is a mild condition that would get better on its own. Complete rest is all that is needed. It shall start to improve in about three days and be better in two weeks.
Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, are helpful for irritable hips as they relieve the pain as well as reduce inflammation around the pain area. Give the ibuprofen according to packet directions every day for 48 hours. Paracetamol might also help with reducing the pain. Never give aspirin to children under the age of 12 years. See our fact sheet for Pain relief for the child.
Antibiotics are not prescribed as the condition is not caused by a bacterial infection.
While your children are recovering:
It is vital to encourage your children to rest at home. They will naturally sit, crawl, walk or lie in the most comfortable positions. Allow your child to gradually go back to their everyday activities as they improve, but they should not play sports or undertake any strenuous activities until they are completely better.
Physiotherapy treatment for the irritable hip syndrome
Acute phase
Rest: Rest prevents worsening of the initial injury. By placing the injured extremity to rest the first 3-7 days after the traumatic part, we can prevent further retraction of the ruptured muscle stump, and reduce the size of the connective tissue scar.
During the initial few days after the injury, a short period of immobilization accelerates the formation of granulation tissue at the site of injury, but it should be noted that the duration of reduced activity mobilization could be limited only until the scar reaches sufficient strength to bear the muscle-contraction induced pulling forces without re-rupture at this point, gradual mobilization should be started followed by a progressively intensified exercise program to optimize the healing by restoring the strength of the injurious muscle, preventing the muscle atrophy, the loss of strength and the extensibility, all of which can follow long term immobilization.
cold application: It is thought to lower intra-muscular temperature and decrease blood flow to the injurious area. Regarding the use of cold on injured skeletal muscle, it has been shown that early use of the cold application is associated with a significantly smaller hematoma between the ruptured myofiber stumps, less inflammation and tissue necrosis, and accelerated early regeneration. But according to the most recent data on the topic, icing of the injured skeletal muscle should continue for an extended period of time( 6 hours) to obtain a substantial effect on limiting the hemorrhaging and tissue necrosis at the part of the injury.
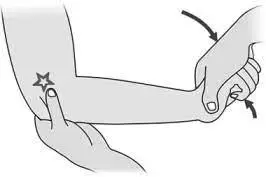
Compression: This may help decrease blood flow at the injury part and accompanied by elevation will serve to decrease both blood flow and excess interstitial fluid accumulation. The goal is to prevent hematoma and interstitial edema, thus decreasing tissue ischemia. However, if the immobilization phase is for a long time, it will be a detrimental effect on muscle regeneration. Cryotherapy, accompanied by compression, should be applied for 15–20 min at a time with 20–50 min between applications. During this time period, the quadriceps should be kept relatively immobile to allow for appropriate healing and prevent further injury around the part.
Elevation: The elevation of an injured extremity above the level of the heart results in a decrease in hydrostatic pressure, subsequently, reduces the accumulation of interstitial fluid, so there is less swelling at the area of injury.
Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, are helpful for irritable hips as they relieve the pain as well as reduce inflammation around the pain area. Give the ibuprofen according to packet directions every day for 48 hours. Paracetamol might also help with reducing the pain. Never give aspirin to children under the age of 12 years. See our fact sheet for Pain relief for the child.
Chronic phase
Ultrasound therapy(US)
Ultrasound is a therapeutic modality that generates ultrasound causes deep heat, provides micro-massage to soft tissue, improves flexibility, promotes healing of tissue as well increases localized blood supply to the area. And ultimately relieving pain.
Short wave diathermy is a deep heating modality that gives heat to provide pain relief, it improves the blood supply to the targeted pain area and removal of waste products.
TENS (transcutaneous electrical nerve stimulation)
Transcutaneous electrical nerve stimulation is an electrical modality that gives pain relief by providing pain modulation. It also stimulates the endogenous opioid system which prevents the release of substance at the anterior grey horn
Exercises for the irritable hip syndrome
External hip rotation: To perform external hip rotation: lie on the bed with both legs out in front. Bend the legs at the knees and press the soles of the feet together. Place a hand on top of both knees and gently push them both down toward the floor. Apply pressure to the knee until there is a stretch, but do not push them further than is comfortable. Hold the stretch for 10 seconds and then relax. Repeat the stretch 5–10 times.
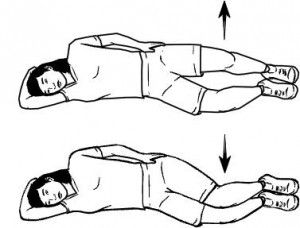
Double hip rotation: To perform double hip rotations: Lie flat on the back. Then, bend the knees and bring them toward the body until the feet are flat on the floor. Gently rotate the knee to the left, lowering them toward the floor. Rotate the head to face the right while keeping the shoulder against the floor. Hold this position for 20–30 seconds. Slowly return both the head and knee to the starting position. Repeat on the opposite side.

Hip and lower back stretch: To perform hip and lower back stretches: Lie flat on the back, bend the knees and bring them toward the body until the feet are flat on the floor. Using the hands, pull both knees in toward the chest. Breathe deeply, pulling the knees closer to the shoulders with each exhalation. Go as far as is comfortable, then hold the position for 20–30 seconds. Breathe normally.

Hip flexion: To perform hip flexion: Stand upright. To perform hip flexion: Stand upright. Extend one arm out to the sides and hold on to a sturdy surface, such as a wall, table, or chair, for support. Slowly raise the right knee to the level of the hip or as far as is comfortable to the patient while keeping the left leg straight. Only hold this position for a second before placing the left foot back on the base. same with the left knee. Do 5–10 repetitions of this exercise.

Hip extension: To perform hip extensions: Stand upright with the legs straight and the feet shoulder-width apart. Extend both arms out in front and hold on to a chair, table, or wall for support. Keeping the right leg straight, lift the left leg backward without bending the knee. Lift the leg as far as possible without causing discomfort, then clench the buttock tightly and hold the position for 5 seconds. Repeat this stretch 5–10 times on each leg. To raise the resistance, try attaching a small weight to the leg.
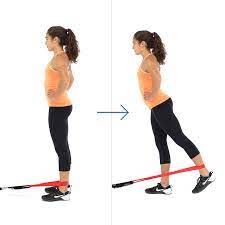
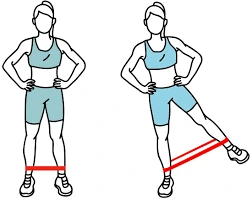
Hip abduction: To perform hip abduction exercises: Stand upright. Extend the left arm out to the side and hold on to something solid, such as a chair, table, or wall. Starting with the foot together, lift the right leg out to the right side. Keep the left leg straight and avoid rotating the hip. Hold the position for 5 seconds and then slowly return the leg to the starting position. Do this exercise 5 to 10 times on one leg, then repeat it on the other side of the leg.
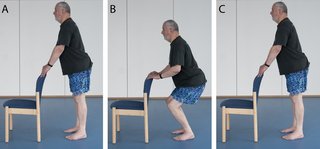
Mini squat: To perform mini squats: Stand upright with the feet shoulder-width apart. If necessary, hold on to a chair, table, or wall for support. Keeping the back straight, gently lower the body by bending the knee until they are above the toe. The feet should remain flat on the base. Hold this position for a few seconds, then slowly straighten the legs to return to the starting position. Repeat these mini squats 5 to 10 times.
Quadriceps exercise:To perform quadriceps exercises.Lie flat on the back and keep the legs straight throughout the exercise. Push the backs of both knees toward the floor and flex both feet by pulling the toes toward the body. Hold the position for 5 seconds, then relax. Do 5–10 repetitions.

surgical treatment for the irritable hip syndrome
When another treatment is ruled out depending upon the conditions, surgical treatment may be considered by the doctor. For instance, When osteoarthritis becomes so severe that the pain is intense or the hip joint becomes deformed, a total hip replacement (arthroplasty) may be a consideration.
FAQ
How long can irritable hips last?
Pain may spread through the hip to the groin, thigh, and knee. The symptoms may cause alarm and discomfort, but an irritable hip is a mild condition that lasts up to 2 weeks.
What not to do if you have a hip problem?
Avoid repeated bending at the hip and direct pressure on the hips. Try not to sleep on the affected side of the hip and avoid prolonged sitting. Pain relievers. Over-the-counter pain relievers such as acetaminophen, ibuprofen, and naproxen sodium (Aleve) may help ease your hip pain.
Is irritable hip contagious?
Children with toxic synovitis may limp, complain of hip and leg pain, or otherwise be reluctant to walk. The condition is not contagious and usually clears up to 2 weeks.
How common is irritable hip?
Irritable hip is a common childhood condition that causes symptoms such as hip pain and limping. Doctors sometimes refer to irritable hips as transient or toxic synovitis. Hip pain isn’t severe, but your children may be reluctant to place weight on the affected leg.
How do I know if my hip pain is serious?
Fever, Bleeding, Exposed bone or muscle, An area that’s warm to the touch, A popping sound, Inability to bear weight.