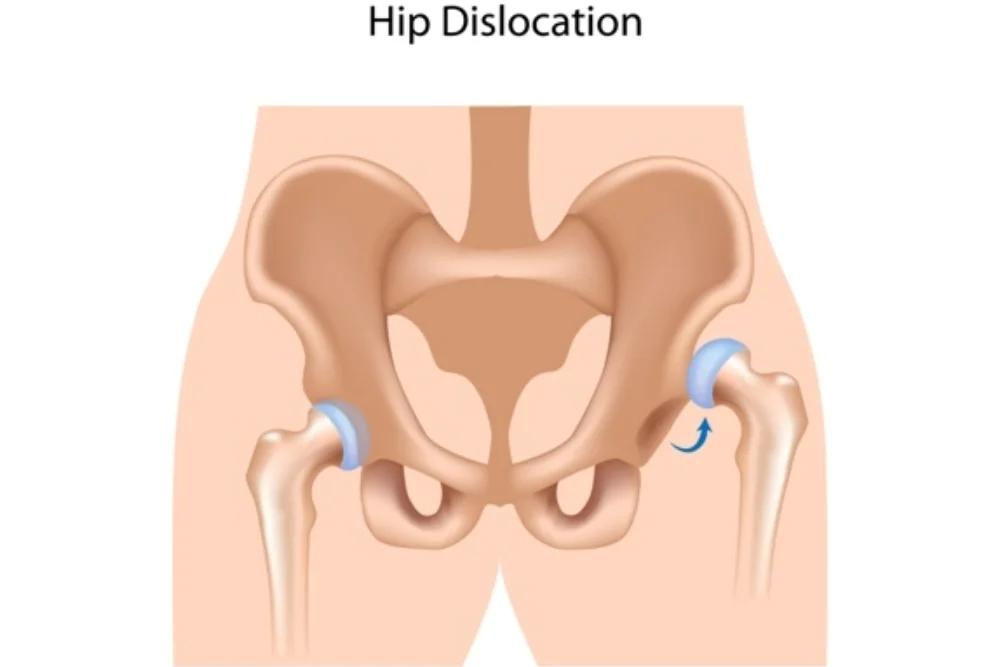
Hip Dislocation
Table of Contents
What is a Hip Dislocation?
Hip dislocation is the femoral head displaced from the socket of the acetabulum. It is a ball-socket type joint. It is a significant traumatic and serious injury.
A hip dislocation is a medical emergency. It causes acute pain and disables the leg until it’s corrected. It can other cause secondary injuries to the blood vessels, nerves, ligaments, and tissues. Hip dislocation can cause long-term damage, especially if it’s not treated correctly. Hip dislocations can occur due to various causes, including traumatic injuries and certain medical conditions. Traumatic dislocations usually result from high-energy incidents such as motor vehicle accidents, falls from heights, or sports-related injuries. Non-traumatic dislocations can be caused by congenital hip abnormalities, connective tissue disorders, or certain neuromuscular conditions.
Hip dysplasia, a disorder in which the hip joint does not fit properly into the socket during development, can occasionally cause hip dislocation. CONGENITAL DISLOCATION OF THE HIP (CDH) is another name for hip dysplasia. People with hip dysplasia have shallow hip sockets, which don’t hold their joints in place like normal hips do. They may also have loose muscles and ligaments in a surrounding hip, so it takes less force to displace their joint.
What are the types of Hip Dislocation?
- Posterior dislocation
- Anterior dislocation
- Central dislocation
- Posterior Dislocation:
- It is the most commonest out of the three types of dislocations of the hip.
- It occurs when the adducted and flexed femur is pushed backward by a violent thrust to the knee, For example when a passenger’s knee hits against the dashboard of a car.
- The femoral head is pushed backward, sometimes fracturing the posterior hip of the acetabulum.
- Clinical Signs:
- Marked localized pain and tenderness
- The lower limb of attitude is flexion, adduction, and internal rotation at the hip. There are identified shortening of the limb
- Stiff and painful attempted movement
- Localized hematoma
- The femoral head is palpable posteriorly at the gluteal part
- The diminished femoral pulsation
- Anterior dislocation:
- It is rare and occurs due to violent abduction force, with the thigh flexed
- It occurs in road traffic accidents
- The dislocated head of the femur may lie on the obturator foramen or the symphysis pubis
- Clinical Signs:
- Localized pain, stiffness, and tenderness
- Inability to bear weight
- The limb appears to be lengthening as it is externally rotated.
- Central Dislocation:
- This type of dislocation results following a fall on the greater trochanter, or due to road traffic accidents
- The floor of the acetabulum is fractured and the femoral head is pushed into the pelvis
- Clinical Signs:
- Serious localized pain and stiffness
- Hip abduction and rotation are restricted with severe pain on attempted movement of the hip joint
- The lower limb remains in neutral rotation and short
What causes Hip Dislocation?
- Road traffic accidents are the most common injury of serious hip dislocations. The dislocation often occurs when the knee strikes the car dashboard in a collision. This force drives the thigh backward, which can lead the femoral head out of the acetabulum socket. Tie your seatbelt which can decrease your risk of hip dislocation during an accident.
- A fall from a height like a ladder or an industrial accident can generate hip dislocation.
- Hip dislocations can happen less frequently with a collision during a game.
- In Children: If children have developmental hip dysplasia (hip dislocation) it might take much less force to dislocate the joint.
- sometimes due to underlying causes medical conditions, like cerebral palsy or neuromuscular disorders.
What are complications of the Hip Dislocation?
A hip dislocation joint can damage the surrounding structures, which can need to be repaired individually. Sometimes, this damage can have long-term significance including:
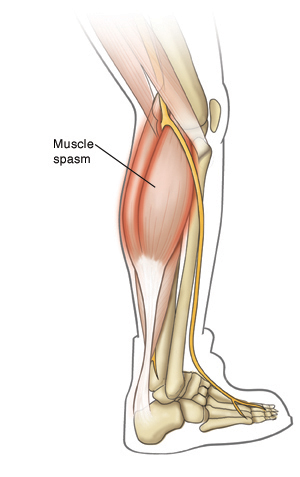
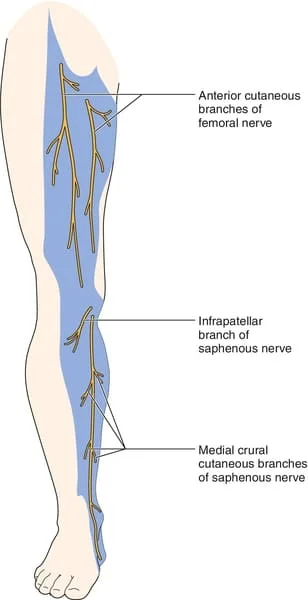
- Nerve damage: The sciatic nerve, which starts in the lower back through the hip and leg, branching into the foot and toes. Compression of your nerve causes severe pain, commonly known as sciatica. Damage to your sciatic nerve can reduce your ability to flex your foot and toes.
- Osteonecrosis: If the femoral artery that runs in front of your joint is damaged, it can affect the circulation of blood to your bone. When blood circulation is poor, your bone tissue begins to die, and hairline fractures started, damaging the structural integrity of your bone. In the later stage, this is called osteonecrosis or avascular necrosis.
- Arthritis: Hip dislocation can harm the cartilage that cushions your ball and Socket joint, and also the ring of cartilage around your joint, known as the labrum. This can lead to arthritis and increases the chances of hip replacement later in life.
- It’s severity and specific complications can vary depending on the type and extent of the hip dislocation, as well as the promptness of medical intervention and treatment. Early medical attention is crucial to minimize the risk of complications and optimize the chances of a successful recovery.
What does a dislocated hip look like?
If you are looking at the injury from the outside, the first thing you will notice is that your leg is locked in a fixed position, rotated either inward or outward. Your hip joint is posteriorly dislocated, ( pulled backward out of its socket) most of the time, which causes your knee and foot to point inward. And Your knee and foot will point outward if you have an anterior dislocation of the hip (when the hip is forced forward out of its socket). Your twisted leg see shorter or longer than the other. Your hip may not be aligned, or you may see swelling or discoloration at the hips around it.
How is a Hip Dislocation diagnosed?
- Medical history: The doctor will inquire about the circumstances leading to the injury, previous hip issues, and any related symptoms.
- Physical examination: The doctor will perform a physical examination, assessing the range of motion, stability, and tenderness of the hip joint. They may also examine the surrounding areas for additional injuries.
- Imaging tests: Anteroposterior pelvis x-ray should confirm the diagnosis
- The X-ray can reveal an excess of the head or neck of the femur and acetabular rim.
- An MRI can find cartilage and labrum.
- CT scans provide accurate bone vision and soft tissues such as ligaments and bursae surrounding the hip joint.
- Scintigraphy (bone scan) is used in the hip to diagnose stress fractures necrosis and tumors
- Ultrasonography is a technique that may be used to detect hip abnormalities and soft tissue problems such as swelling.
What is the medical treatment for Hip Dislocation?
The treatment of hip dislocations is operative and non-operative.
- Non-surgical:
With the hip in 90° of flexion, the traction force is applied in the direction opposite to the dislocation to treat closed hip reduction. To avoid damage to the cartilage and soft tissues, this should be done under either general or regional anesthesia and muscular relaxation. It is also performed in theatre without anesthesia. After the move, the hip’s stability was thoroughly examined. A period of bed rest is recommended depending on the stability of the hip and the extent of the soft tissue injuries. - Surgical:
Failed conservative relocation. Instability following conservative relocation. Associated fractures of the femur head and acetabulum. Loose bone fragments in joint space behind relocation.
Hip Dislocation Physical Therapy – Will Physiotherapy Help?
Yes, Physical therapy will be necessary for hip dislocation. It is essential to consider the time frames for soft tissue healing with rehabilitation following a hip dislocation. Complete restoration following hip dislocation takes 3-6 months.
During immobilization:
- Isometric exercises for the gluteus, hip flexors, quadriceps, and hamstrings should be done as soon as possible to regain control of the hip joint. Small-range movements can be initiated in skeletal traction patients after three weeks.
- When engaging in movements that increase the risk of dislocation, such as hip adduction and internal rotation with flexion for posterior dislocation and hip abduction and external rotation for anterior dislocation.
During mobilization:
- Vigorous exercises should be initiated to recover the range of hip movements, and strength at the displaced hip.
- Knee mobilization becomes vital in patients treated with hip spica.
- Assisted straight leg raise (SLR) should be started and emphasized to regain hip joint control.
- Once controlled hip movements are regained, ambulation can be started with enough assistance by 12 week
Physiotherapy Treatments:
- Reduction of pain
- Progression of weight bearing
- Improving range of motion
- Hip stability
- Hip Dislocation Physical Therapy Exercises
- Gait reduction: Initially with assistive mobility devices (Crutches and walkers) to limit weight bearing and progression
- Improve lower hip range of motion including hip mobilization
- Strengthening muscles around the hip, focusing on hip stabilizers muscles such as Hip abductors, adductors, extensors, and flexors.
- Stretching all hip muscles
- Graded return to activity/sport
Hip dislocation physical therapy treatment plan, therapists may use modalities like :
- Ultrasound
- Electrical stimulation
- Ice; and
- Cold laser
- to reduce pain and inflammation.
Other Exercises:
- Bridging: Lie flat on the back position. Keep your arms with palms down beside the body. Keep feet hip distance apart and bend the knees. Slowly lift your hips upward. Keep it in this position for three to five seconds. This helps the glutes strengthen and increase the stability of the hip joint.
- Supine leg abduction: Lie flat on the back position. Slowly slide one leg away from the body and then back in, maintaining the knees straight. This exercises the gluteus medius and helps to maintain hip stability while walking.
- Side Lying Leg abduction: Lie on one side with one leg on top of the other leg. Slowly lift the top leg gradually towards the ceiling and then lower it back to normal.
- Standing Hip abduction: Standing up and holding on to a nearby object, slowly lift one leg away from the midline of the body and then lower it back to the normal starting position. This is simply a more advanced way to do any of the lying hip abduction exercises and should be done as the patient progresses in rehabilitation.
- Knee raises: While standing and holding onto a chair, slowly raise one leg off the ground and bring it closer to the body while bending the knee. Then lower the leg back down slowly. This helps to maintain hip stability and strengthen the muscles that flex the hip.
- Hip flexion and extension: Standing, holding on to a nearby chair or surface. Swing one leg in front of you and keep it there for three to five seconds. Then swing the leg slowly and return behind your body. Hold the position for 3 to 5 seconds. This exercise helps to increase the range of motion and also strengthens the hip flexor and hip extensor muscles that control the hip joint.
- As recovery progresses, adding ankle weights to any workouts is possible.
Physiotherapy treatment in children for congenital hip dislocation:
- Isometric exercises to the gluteus and quadriceps muscles
- Active Range of motion exercises of hip and knee joint
- AROM for the Hip, Knee, and Ankle joints
- Gentle relaxed passive movements
- Special focus is given to the passively relaxed adduction.
- Isometric, Isotonic, and progressive resistive exercises are planned
- Gradual weight-bearing and walking with the help of assistive devices
- Initially, the wide base walk may be required to maintain the balance
- The patient may be allowed to walk independently after regaining sufficient ROM and muscle strength
How can I stop my hip dislocation again?
Follow these precautions for 6 weeks after injury:
- Sit with your feet flat on the ground and your back neutral. Avoid crossing your legs. When sitting in a chair, try not to lean forward.
- Your knees should remain apart. When you sit or lie down, place a pillow or wedge between your knees. Avoid bending your knees. Avoid raising your knees above your hips.
- Avoid sitting in a low chair. To get up from a seated position, push yourself up using the armrests and your upper body strength.
- Avoid bending at the waist when picking something up off the ground. To pick up the object, use a tool or budge your knees.
What are the dos and don’ts of Dislocation?
If you or someone else experiences a dislocation, seek medical help immediately.
Do’s of Dislocation:
- A healthcare provider should handle the treatment of dislocations.
- Immobilize the injured area.
- Applying ice might help reduce swelling and relieve pain in the affected area. Apply an ice pack or ice cubes wrapped in a cloth to the skin.
- Elevate the injured limb or joint above heart level. This can help minimize swelling and reduce pain.
Don’ts of Dislocation:
- Without the right medical training, trying to move a dislocated joint risks severe harm.
- Delaying medical care or ignoring an injury might cause complications and extend recovery.
- Applying heat can aggravate swelling and inflammation because it might increase blood flow to the affected area.
- Avoid trying to move or rotate the limb or joint that is injured.
What is the prognosis for a Dislocated Hip?
- Hip dislocations depend upon how long it takes to decrease the dislocation other structures nerves, ligaments, and soft tissue are damaged.
- A sciatic nerve injury affects 10% of patients with hip dislocations.
- Femoral head avascular necrosis occurs in 2%–10% of patients with hip dislocations.
- Osteoarthritis in the hip joint develops in about 20% of people with hip dislocation.
- An acetabulum fracture will occur in roughly 70% of patients with posterior hip dislocations.
Summary
It is a severe and often traumatic injury that requires immediate medical attention. Hip dislocation can be very painful. It is essential to consult a healthcare professional for a proper evaluation, diagnosis, and treatment of hip dislocation, as they can provide personalized guidance and care based on the individual’s specific circumstances.
FAQ:
What is the immediate treatment for a Hip Dislocation?
A hip dislocation is a medical emergency. The immediate treatment involves seeking immediate medical attention. Paramedics or medical professionals will typically perform a procedure called a “closed reduction” to put the hip joint back into its socket. This is often done under anesthesia.
What is the recovery process after a Hip Dislocation?
Recovery after a hip dislocation depends on the severity of the injury and any associated complications. It usually involves a period of immobilization using a brace, crutches, or a wheelchair to allow the hip to heal. Physical therapy and rehabilitation exercises are commonly recommended to restore strength, flexibility, and range of motion.
Are there any long-term complications associated with a Hip Dislocation?
While the majority of hip dislocations can be successfully treated, there can be potential complications. These may include hip instability, recurrent dislocations, fractures, nerve or blood vessel damage, avascular necrosis (poor blood supply to the femoral head), or the development of post-traumatic arthritis.
What should I do if I suspect a Hip Dislocation?
If you suspect a hip dislocation, it’s important to seek immediate medical attention. Do not try to move the affected leg or hip yourself, as this can cause further damage. Instead, call for emergency medical assistance or go to the nearest emergency room.
Do you need physiotherapy after Hip Dislocation?
After the hip is reduced, physiotherapy plays a crucial role in the recovery process. The goals of physiotherapy after hip dislocation are to reduce pain, restore joint mobility, strengthen the surrounding muscles, and improve overall function.


One Comment