Distal Radius Fracture
Table of Contents
What is a Distal Radius Fracture?
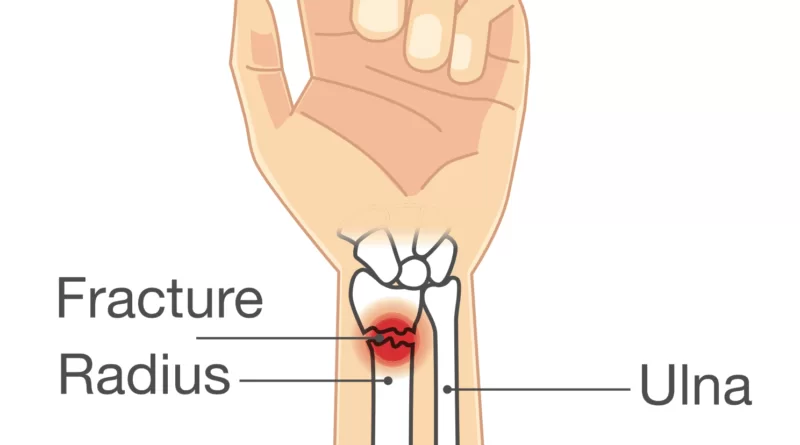
A distal radius fracture, also called a wrist fracture, is a crack in the part of the radius bone which is near the wrist. clinical manifestations present of pain, bruising, and instantaneous-onset swelling. The ulna bone may even be broken. In younger individuals, these fractures commonly happen during sports or motor vehicle accidents. In more senior people, the most common reason is a history of falling on an outstretched hand. Characteristic kinds possess Colles, Smith, Barton, and Chauffeur’s fractures.
The diagnosis is typically questioned and established on clinical manifestation and verified with X-rays. Treatment is with casting for 6 weeks or surgery. Surgery is typically pointed if the joint surface is cracked and does not line up in the proper position, the radius is too short, or the joint surface of the radius is inclined more than 10 percent backward. Among those who are cast, repeated X-rays are suggested within three weeks to confirm that a good position is possessed.
Distal radius fractures are standard and are the most typical kind of fractures that are noticed in juveniles. Distal radius
fractures describe between 25 percent and 50 percent of all broken bones and appear most typically in young men and older women.
A year or two can be needed for healing to happen. Most children with a buckle wrist fracture occasion a broken wrist for life and do have a high chance of re-fracturing the same spot or other negative consequences.
Symptoms of Distal Radius Fracture
The patient usually presents with a history of falling on an outstretched hand and complaints of pain and swelling around the wrist, sometimes deformity around the wrist is also present. Any feeling of numbness should be asked to eliminate median and ulnar nerve damage. Any type of pain in the extremity on the involved side must also be examined to exclude related damage to the involved extremity.
The normal clinical features of a person with a distal radius fracture are the presence of swelling, deformity, tenderness, and lack of wrist movement. “Dinner fork” deformity of the wrist is the reason for the posterior displacement of the carpal bones (Colle’s fracture). The Opposite of that deformity is seen in anterior angulation (Smith’s fracture). The wrist can be radially deviated because of to shortening of the radius bone. Assessment must also rule out a skin wound that may recommend an open fracture, commonly at the side. Tenderness at a region with no obvious deformity can still point to underlying fractures. Reduced sensation particularly at the tips of the radial three-and-one-half digits (thumb, index finger, middle finger, and radial portion of the ring finger) can be due to median nerve injury.
Swelling and displacement can lead to compression on the median nerve which may lead to acute carpal tunnel syndrome and needs immediate treatment. Very infrequently, stress on the muscle components of the hand or forearm is enough to create a compartment syndrome which can display extreme pain and sensory deficiencies in the hand. Posterior displacement of carpal bones found in posteriorly angulated distal radius fracture, making a dinner fork-like called “Dinner fork” deformity.
Complications
Nonunion is infrequent; basically, all of these fractures recover. Malunion, yet, is not unusual and can result in residual pain, weakness in the grip object, decreased range of motion (particularly rotation motion ), and tenacious deformity. Symptomatic malunion may need further surgery. If the joint surface is injured and recovers with more than 1–2 mm of inequality, the wrist joint will be inclined to post-traumatic osteoarthritis. most non-osteoporotic patients will have post-traumatic arthritis, predominantly decreased in radial deviation and wrist flexion. This arthritis can deteriorate as time passes. Displaced fractures of the ulnar styloid corresponding to a distal radius fracture direct to the instability of the DRUJ and lead to loss of forearm rotation.
Nerve injury, particularly of the median nerve and contributing to carpal tunnel syndrome, is generally reported following distal radius fractures. A tendon injury can occur in patients during treatment of both ways- nonoperatively and operatively, considerably typically to the extensor pollicis longus tendon. This can be because of the tendon coming in touch with protruding bone or with the hardware placed next to surgical processes.
Complex regional pain syndrome is also linked with distal radius fractures and can propose with pain, swelling around the wrist, altered color and temperature, or joint contracture
Cause of Distal Radius Fracture
A history of falls on an outstretched hand from standing height is the most common reason for this kind of fracture, although few fractures will be because of high-energy injury. Individuals with a present history of falls on the outstretched hand are commonly fitter and have better reflexes if compared to those who have a present history of elbow or humerus fractures. The characteristics are influenced by the which position of the hand at the duration of impact, the variety of surfaces, the velocity of the impact, and the strength integrity of the bone. Distal radius fractures commonly happen with the wrist tilted posterior from sixty to ninety degrees. The radial styloid fracture will happen if the wrist has deviated to the ulna side and vice versa. If the wrist deviated posterior less, then a proximal forearm fracture would happen, but if the deviating posterior is more, then a carpal bone fracture would happen. With increased bending back, more force is needed to have a fracture. More force is needed to create a fracture in men than in women. Risk of damage additions in those with osteoporosis.
Familiar injuries linked with distal radius fractures are interosseous intercarpal ligament damages, particularly scapholunate (4.7 percent to 46 percent of cases) and lunotriquetral ligament (12 percent to 34 percent of patients) damages. There is an increased risk of interosseous intercarpal damage if the ulnar variance (the disparity in length between the distal end of the ulna and the distal end of the radius) is > 2mm and there is a fracture in the wrist joint. Triangular fibrocartilage complex (TFCC) damage happens in 39 percent to 82 percent of patients. Ulnar styloid process fracture enhanced the risk of TFCC damage by a factor of 5:1. Nonetheless, it is indefinite whether intercarpal ligaments and triangular fibrocartilage injuries are linked with long-term pain and disability for those who are involved.
Diagnosis
Diagnosis can be enunciated clinically when the distal radius is deformed but must be verified by X-ray. The differential diagnosis contains fractures of the scaphoid and dislocations of the wrist. Periodically, fractures may not be noticed on X-rays instantly after the injury. Delay in the X-rays, X-ray computed tomography (CT scan), or Magnetic resonance imaging (MRI) may prove the diagnosis.
An X-ray of the involved wrist is needed if a fracture is presumed. Posteroanterior, lateral, and oblique views may be used concurrently to explain the fracture. X-rays of the intact wrist must also be carried out to specify if any normal anatomic variations present before surgery.
A CT scan is usually perpetrated to further examine the articular anatomy of the fracture, particularly for fracture and displacement within the distal radio-ulnar joint.
Different types of information can be received from X-rays of the wrist:
Lateral view
- Carpal malalignment – Carpal malalignment – Two lines are marked along the long axis of the radius and capitate bone. If the carpal bones are aligned, both lines cross each other within the carpal bones. If the carpal bones are not unaligned, both lines will bisect within the carpal bones. If the carpal bones are unaligned, both lines will bisect beyond the carpal bones. Carpal malignment is oftentimes linked with the posterior or anterior inclination of the radius and will have inadequate strength of the grip and inadequate forearm rotation.
- Tear drop angle – It is the angle between the line that passes through the central axis of the anterior rim of the lunate facet of the radius and the line that passes through the long axis of the radius. Tear drop angle < 45 degrees reveals displacement of the lunate facet.
- Antero-posterior line – On lateral X-ray, it is the line b/w the volar or dorsal rim of the lunate facet of the radius. The usual length is 19 mm. Heightened AP length means the lunate facet fracture.
- Posterior or anterior tilt – A line is pulled joining the most distal ends of the posterior and anterior sides of the radius. the 2nd line to the longitudinal axis of the radius is kept. The angle between the two lines is the angle of the posterior or anterior tilt of the wrist. Dimensions of posterior or anterior tilt must be constructed in a true lateral view of the wrist due to the pronated forearm decreasing the volar tilt and supination increasing it. When the posterior tilt is > 11 degrees, it is linked with a lack of strength of the grip and loss of wrist flexion.
Posteroanterior view
- Radial inclination – It is the angle between a line pulled from the radial styloid to the medial end of the articular surface of the radius and a line pulled perpendicular to the long axis of the radius. lack of radial tilt is related to the lack of strength of the grip.
- Radial length – It is the vertical length in millimeters between a line tangential to the articular surface of the ulna and a tangential line pulled at the most distal point of radius (radial styloid). Shortening of radial length of >4mm is linked with pain in the wrist.
- Ulnar variance – It is the vertical length between a horizontal line parallel to the articular surface of the radius and another horizontal line pulled parallel to the articular surface of the ulnar head. Positive ulnar variance (ulna seems extended than the radius) disturbs the virtue of the triangular fibrocartilage complex and is linked with a lack of strength of the grip and pain in the wrist.
Oblique view
- The portion of the screws at the radial side of the distal end radius is secured by an oblique view of the distal radius in pronation, which enables the position of the degree of contact of the distal end radius and the depression of the radial styloid. On the other hand, a supinated oblique view reveals that the screws on the ulnar side of the distal end radius and the depression of the posterior boundary of the lunate facet are responsible for the distal radius’ ulnar side.
Classification of Distal Radius Fracture
There are numerous classification grouping for distal radius fracture. AO or OTA classification is native to Orthopedic Trauma Association and is the most usually used classification system. A—extra-articular, B—partial articular, and C—complete articular are the 3 major groups that can again be divided into 9 main groups and 27 subgroups rely on the degree of connection and position of displacement. Nevertheless, none of the classification systems show great susceptibility. A qualification modifier (Q) is used for connected ulnar fractures.
For children and teenaged, there are 3 primary categories of fracture: buckle (torus) fractures, green stick fractures, and complete (or off-ended) fractures. Buckle fractures are uncompleted breaks in the bone that possesses the cortex (outside) of the bone. Buckle fractures are steady and are the most communal kind. Greenstick fractures are bone that is damaged only on one side and the bone stick to the other side. Greenstick fractures are unstable and oftentimes take place in junior children.
Complete fractures, where the bone is totally broken, are not stable. In a complete fracture, the bone can be misaligned from its anatomical position. For a complete fracture, unopened fractures are those in which the connective tissue like skin depending on the bone is intact. An open fracture (exposed bone) is a real trauma.
Treatment of Distal Radius Fracture
Correction must be appropriated if the wrist radiology falls outside the standard limits:
- 2-3mm positive ulnar variance
- There should be no carpus misalignment
- If the carpus is aligned, then the dorsal tilt must be<10 degrees
- If the carpus is aligned, there are no limits for palmar inclined
- If the carpus is unaligned, wrist inclination must be neutral
- Gap or step deformity is < 2mm
Treatment options for distal radius fractures include nonoperative management, external fixation, and internal fixation.[Indications for each depend on a variety of factors such as the patient’s age, initial fracture displacement, and metaphyseal and articular alignment, with the ultimate goal to maximize strength and function in the affected upper extremity. Surgeons use these factors combined with radiologic imaging to predict fracture instability, and functional outcomes to help decide which approach would be most appropriate.
Treatment is often directed to restore normal anatomy to avoid the possibility of malunion, which may cause decreased strength in the hand and wrist. The decision to pursue a specific type of management varies greatly by geography, physician specialty (hand surgeons vs. orthopedic surgeons), and advancements in new technology such as the volar locking plating system.
Distal radius fractures are often associated with distal radial ulnar joint (DRUJ) injuries, and the American Academy of Orthopedic Surgeons recommends that post-reduction lateral wrist X-rays should be obtained in all patients with distal radius fractures in order to preclude DRUJ injuries or dislocations.
Most children with these types of fractures do not need surgery.
Nonoperative
Most distal radius fractures are controlled with conservative nonoperative management, which regards immobilization via utilization of plaster or splint with or in the absence of closed reduction. The ratio of the nonoperative approach to distal radius fractures is around 70 percent. Nonoperative management is informed for fractures that are un-displaced, or for displaced fractures that are stabilized and then reduced. Variants in the immobilization method concern the kind of cast, place of immobilization, and the extent of time needed in the cast.
Undisplaced fractures
For those with a low-level condition, a cast and splint can be practical for two weeks. In those who are immature and active, if the fracture is un-displaced, the patient can be followed up in one week. If the fracture is quite un-displaced, a cast and splint can be practical for three weeks. If the fracture is displaced, then manipulative reduction or surgical stabilization is needed. Shorter immobilization is related to improved healing when contrast to extended immobilization.10 percent of the minimally displaced fractures will become unstable in the first two weeks and lead to malfunction. Consequently, follow-up within the first week of fracture is of import. 22 percent of the minimally displaced fractures will be malunited after two weeks. Consequently, follow-ups at two to three weeks are hence also crucial. There is weak indicant to propose that few children with a buckle fracture may not demand cast immobilization.
Where the fracture is not displaced and stabilized, nonoperative treatment regard immobilization. At the start, a back slab or a sugar tong splint is practical to permit swelling to enlarge and afterward, a cast is practical. Count on the nature of the fracture, the cast can be set above the elbow to control forearm rotation. Nevertheless, an above-elbow cast may cause long-term rotational contractual. For torus fractures, a splint may be adequate and casting may be ward off. The position of the wrist in the cast normally has little flexion and ulnar deviation. Yet, neutral and dorsiflex positions may not impact the staleness of the fracture.
Displaced fractures
In a displaced fracture, the hand can be cast until the individual senses convenience. If the fracture impacts the median nerve, just then is a reduction indicated. If the instability threat is < 70 percent, the hand can be manipulated under general anesthesia(MUGA) to perform the reduction. If the post-reduction X-ray of the wrist is acceptable, then the individual may reach for a follow-up at one, two, or three weeks to examine for any displacement of fractures during this time. If the reduction is sustained, then the cast must continue for four to six weeks. In the displaced fracture, surgical management is the right option. If the unreliability risk of the wrist is > 70 percent, then surgical management is necessary.43 percent of displaced fractures will be inconsistent within the initial two weeks.& 47 percent of the staying unstable fractures will become unstable after two weeks. Accordingly, regular inspections are crucial to avert the malunion of the displaced fractures.
Closed reduction of a distal radius fracture concerns first anesthetizing the affected parts with a hematoma block, and intravenous local anesthesia (Bier’s block). Manipulation generally possesses first placing the arm under traction and unlocking the segments. The deformity is then reduced with properly closed manipulation (relying on the kind of deformity) reduction, after which a splint or cast is placed and an X-ray is carried out to confirm that the reduction was successful. The cast is normally kept for about six weeks.
The result of nonoperative treatment
Failure of nonoperative treatment resulting in functional impairment and anatomic deformity is the biggest danger linked with conservative management. Earlier investigations have unveiled that the fracture commonly displaces its initial place even in a cast. Only 27-32% of fractures are in allowable alignment 5 weeks after closed reduction. For those above 60 years old, there will be a posterior angulation of 13, while for those above 60 years old, the posterior angulation can receive as high as 18. In individuals over sixty, functional impairment can stay for > ten years.
Despite these threats with nonoperative treatment, more current systematic appraisals indicate that when indicated, nonsurgical management in the elderly population may result in equivalent functional results as surgical methods. In these analyses, no marked differences in pain scores, the strength of the grip, and the range of motion in patients’ wrists appeared when comparing conservative nonsurgical approaches with surgical management. Although the nonsurgical class exhibited more prominent anatomic misalignment for example deviation in radial aspect and ulnar variance, these distinctions did not occur to have a marked result on general pain and quality of life.
Surgery for Distal Radius Fracture
Surgery is commonly used for displaced or unstable fractures. The method of surgical management involved open reduction internal fixation (ORIF), external fixation, percutaneous pinning, or sometimes a combination of the above. The choice of operative treatment is frequently chosen by the kind of fracture, which can be categorized widely into three classes; partial articular fractures, displaced articular fractures, and metaphyseal unstable extra- or minimal articular fractures.
Significant advances have been made in ORIF treatments. Fragment-specific fixation and fixed-angle volar plating are the two more recent treatments in recent times. This attempt fixation is rigid sufficiently to enable virtually immediate mobility, in an effort to minimize stiffness and improved maximum function; no improved final outcome from early mobilization (prior to six weeks after surgical fixation) has been established.
Although reparation of the radiocarpal alliance is ideal to be of obvious import, the same quantity of angulation, contracting, intra-articular opening, or step which impacts ultimate function is anonymous.
The alignment of the DRUJ is also very vital as this can be the source of pain and lack of rotation after complete recovery and recovery.
An arthroscope can be used at the period of fixation to evaluate for soft-tissue injury and the congruity of the joint surface and may improve the accuracy of joint surface alignment Structures at risk possess the triangular fibrocartilage complex and the scapholunate ligament. Scapholunate damages in radial styloid fractures where the fracture line present distally at the scapholunate interval must be regarded. TFCC injuries compelling obvious DRUJ instability can be addressed at the duration of fixation.
The prognosis differs depending on several variables. If the anatomy (bony alignment) is not correctly fixed, the function may stay inadequate even after recovery. Restoration of the bony alignment is not an all-time success, as soft tissue contributes immensely to the restorative process.
Little joint involvement
These fractures are the most typical of the three groups mentioned above that require surgical management. A minimal articular fracture concerns the joint but does not need a decrease in the joint. Manipulative reduction and immobilization are helpful for metaphyseal unstable fractures. Regardless, several investigations indicate this method is mostly ineffective in patients with high functional demand, and in these circumstances, more stable fixation techniques must be utilized.
Surgical choices have been demonstrated to be victorious in patients with unstable extra-articular or minimal articular distal radius fractures. These choices possess percutaneous pinning, external fixation, and ORIF using plating. Patients with inadequate usefulness demand of their wrists can minister with success with nonsurgical administration; irrespective, in more active and fit patients with fractures that are irreducible by closed means, non-bridging external fixation is selected, as it has somewhat real complications when contrast to other surgical alternatives. Pin tract infection is the commonest complication linked with nonbridging external fixation, which can be resolved with antibiotics and repeated dressing changes, and rarely outcome in reoperation. The external fixator is placed for five to six weeks and can be removed in an outpatient setting.
If the fractures are improbable to be lessened by closed means, open reduction with internal plate fixation is desired. Although major complications (that is injury of the tendon, fracture collapse, or malunion) lead to increased reoperation rates (36.5 percent) corresponding to external fixation (6 percent), ORIF is chosen, as this supplies more reasonable stability and restoration of the anterior inclination. Following the operation, a removable splint is set for two weeks, during which time patients must mobilize the wrist as bearable.
Displaced intra-articular fractures
These fractures, although unusual, repeatedly need surgery in active, healthy patients to address displacement of both the joint and the metaphysis. The two mainstays of restorative are bridging external fixation or ORIF. If deduction can be achieved by closed or percutaneous reduction, then open reduction can generally be prevented. Percutaneous pinning is preferred to plating because of similar clinical and radiological results, as well as cheap costs when compared to plating, instead of the enhanced risk of superficial infections. The level of joint restoration, as opposed to the surgical method, has been found to be a better indicator of functional results.
FAQ
It is peremptory to be seen for medical lookout as soon as possible if you think that you have cracked your distal radius bone. When left non-treated or late-treated, wrist fractures can consequence in advanced complications that can have long-lasting effects. There are various distal radius fracture derivatives are accessible to patients.
If the distal radius fracture is in an adequate place, a splint or cast is practical. It frequently functions as final management until the bone recovers properly. Commonly a cast will stay on for up to 6 weeks. Then you will be granted a dismissive wrist splint to wear for comfortableness and support.
Iron aid our body form collagen to reconstruct bone. It also plays an important role in acquiring oxygen into our bones to aid them in recovery. Best sources: Red meat, dark-meat chicken or turkey, seafood like oily fish, eggs, dried fruits like almonds and cashew, Healthy green vegetables, whole-grain bread, and fortified cereals.
In the mean, plaster casts stay on for about one month, rely on your age, overall health, and kind of fracture. Even once the plaster is terminated, the bone is yet healing so you should take all possible protection for at least another month.
Smith’s fractures, even understood as reverse Colles’ fractures, are defined as a palmar tilt of the distal fragment. Barton’s fracture is the displaced intra-articular coronal plane fracture-subluxation of the posterior lip of the distal radius with a displacement of carpus with the piece.
There are definite bones that are more liable to recover without a cast. They exclude the collarbone, wrist, and a few ankle fractures. These bones have adequate blood circulation, which assists with recovery. In addition, they are not under as much pressure as other bones in the body, so they are little liable to break again.




One Comment